Tachycardia is one of the most common heart rhythm disorders. The main mechanism for the development of pathology is to increase the automaticity of the sinus node. In this case, the heart rate increases to more than 90 beats per minute. Tachycardia may not have subjective manifestations. Most often it is felt as increased heartbeat. In the presence of pathologies of the cardiovascular system, this type of arrhythmia can worsen the general condition and provoke the development of complications. Therefore, treatment of tachycardia should be prescribed and strictly monitored by a specialist.
What factors affect heart rate?
The most common non-infectious pathology in all countries of the world is diseases of the circulatory system. Based on the results of epidemiological studies dating back to the late 90s of the 20th century, WHO experts came to the conclusion that an increase in heart rate (HR) at rest is one of the risk factors for the development of cardiovascular diseases in healthy people.
According to the national recommendations of the All-Russian Scientific Society of Cardiology, the resting heart rate of a healthy adult should be no more than 80-85 beats per minute and correspond to the pulse rate. The optimal heart rate for an adult at rest is from 60 to 80 beats per minute, while the specific heart rate is individual for each person and depends on a number of factors.
The first is gender. Women have higher normal heart rates than men. This is explained by the specific characteristics of hormonal and emotional backgrounds.
The second is age. In adults, the normal heart rate increases with age: at the age of up to 50 years, the average normal value is 70 beats per minute, at the age of 50-60 years - 74 beats per minute and 79 beats per minute in people over 60 years of age.
In addition, heart rate depends on lifestyle, including physical activity: trained people have a lower heart rate than those leading a sedentary lifestyle. Bad habits also have an impact - smoking, alcohol abuse.
And finally, this indicator correlates with external factors: heart rate increases with lack of sleep, nervous tension, after a heavy meal, increased ambient temperature, etc.
What does tachycardia mean in a child?
Pediatric cardiologists consider it a disease when the number of heart beats per minute exceeds the norm by 20-30.
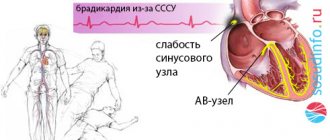
On a note! An impulse originates in the sinus node in the right atrium, which spreads to the atria and causes them to contract. The impulse is briefly delayed in the atrioventricular node between the ventricles and atria and transmitted to the ventricles, causing them to contract. The sinus node independently creates impulses within itself at a certain frequency. This is called "sinus rhythm."
Tachycardia is not an independent disease, but a sign of some other pathology. However, there is physiological tachycardia, which occurs during physical activity, emotional arousal, during eating, and when body temperature rises. This condition is completely harmless and does not threaten the child’s life. Tachycardia can occur even in a newborn child if he laughs, tries to make movements that are new to him, etc.
How to correctly calculate your pulse?
For self-counting, the most common method is palpation (palpation) of the radial artery of the wrist. You need to count your pulse at rest, no earlier than 2 hours after eating, bathing, or massage. The accuracy of the result depends on the correct counting technique.
First, you need to take a watch or stopwatch. Sit down with your hand on a horizontal surface, palm up. Place the index, middle and ring fingers of the opposite hand on the wrist approximately 3 centimeters from the base of the thumb;
When you feel the pulsation, you need to lightly press the artery to the inside of the radius. There is no need to press with force, as the pulse wave may disappear under pressure.
Then you need to count the number of blood pulses within 1 minute. Pulse waves should follow each other at regular intervals; then count the pulse on the second hand.
An increase in heart rate at rest greater than 90 beats per minute is considered tachycardia.
Diagnosis of tachycardia
Electrocardiography
The ECG plays a leading role in the differential diagnosis of tachycardia and in helping to identify its causes. This method allows you to determine the type of pathology, as well as the rhythm and heart rate. If the severity of symptoms of cardiac tachycardia increases, it is advisable to conduct daily Holter ECG monitoring. This method is highly informative. It allows you to identify and analyze any heart rhythm disturbances within 24 hours. Holter monitoring helps detect ischemic changes during normal physical activity.
Echocardiography
It is a standard examination method to exclude heart pathology in case of any rhythm disturbances. Thanks to echocardiography, the doctor receives data on the size of the heart chambers, the thickness of the myocardial walls, and changes in the valve apparatus. This examination allows you to identify violations of local contractility.
Electrophysiological study
This is an invasive method of examining patients with cardiac pathology. Electrophysiological testing is used when appropriate before surgery to treat arrhythmia. Used to diagnose different types of tachycardia in a limited number of patients. This method boils down to determining the nature of the propagation of an electrical impulse throughout the myocardium, making it possible to determine the mechanisms of tachycardia or cardiac conduction disorders.
Additional examinations
Additional research methods are used to identify the causes of cardiac pathology. The specialist may prescribe a blood test (general and thyroid hormone tests) and electroencephalography. In rare cases, an MRI of the heart is performed, usually to detect congenital abnormalities.
Physiological and pathological tachycardia
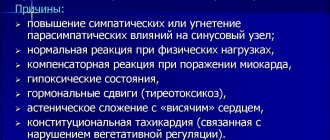
Depending on the causes of occurrence, physiological and pathological tachycardia are distinguished.
Physiological tachycardia occurs during emotional, physical stress, high temperature and humidity, being in hot and stuffy rooms, abuse of tonic drinks - strong tea, coffee, energy drinks, taking certain medications, smoking or drinking alcohol.
In healthy people, physiological tachycardia is an adaptive mechanism and, when the external stimulus is removed, the heart rate returns to normal within 5 minutes.
Pathological tachycardia occurs in cardiovascular, endocrine, acute infectious, oncological and other diseases and accompanying conditions - dehydration, large blood loss, shock conditions, pain syndrome, etc. - or when the functioning of the autonomic nervous system is disrupted.
Thus, tachycardia at rest is most often a symptom of some disease and requires medical examination.
With tachycardia, the heart works under increased load and does not have time to fill with blood in the required volume, the blood supply to all organs deteriorates, and oxygen starvation develops.
The kidneys, organs of vision and gastrointestinal tract, central and peripheral nervous systems suffer, and the course of existing diseases is complicated.
The heart muscle gradually wears out, which can result in heart failure. In addition, there is a life-threatening type of tachycardia, so a visit to the doctor cannot be postponed.
Causes
Among the causes of tachycardia development, cardiac and extracardiac (extracardiac) are distinguished.
The first group includes the following conditions:
- Cardiac ischemia.
- Arterial hypertension.
- Acute and chronic heart failure.
- Endo-, myo- or pericarditis.
- Congenital and acquired valve defects.
- Atherosclerosis of the aorta and other large vessels.
From the nervous system, tachycardia can occur:
- Cardiopsychoneurosis.
- Neuroses and psychoses.
Also, increased heart rate can be caused by:
- Anemia of various origins.
- Hypoxemia (insufficient oxygen saturation of blood cells).
- Hypovolemic and hemorrhagic shock or collapse.
- Diseases of the endocrine system (thyrotoxicosis).
- Oncological diseases (pheochromocytoma).
- Hyperthermia that develops as a result of inflammatory or infectious processes in the body (ARVI, influenza, pneumonia, etc.).
Tachycardia can also occur while taking a number of medications and chemical compounds. These include:
- Hormonal drugs (corticosteroids, thyroid-stimulating drugs).
- Sympathomimetics (Adrenaline).
- Anticholinergics (Platifillin, Atropine).
- Diuretics (Furosemide, Indapamide).
- Drinks containing caffeine or ethyl alcohol.
- Nicotine.
When should you see a doctor?
Alarming symptoms include constant heartbeat at rest with a heart rate of more than 80 beats per minute, different time intervals between pulse beats when counting the pulse, different pulse values on the left and right arms.
You should also consult a doctor in case of fainting, episodes of loss of consciousness, chest pain, a feeling of “interruptions” in the heart, tachycardia after blood loss, vomiting, diarrhea, when tachycardia is combined with shortness of breath, dizziness, insomnia, frequent headaches, increased blood pressure. pressure, increased sweating, trembling hands.
In addition, it is important to inform your doctor if tachycardia occurs even with minor physical activity and does not go away within 5 minutes, as well as if an attack of tachycardia begins suddenly or there are repeated attacks.
An attack of tachycardia is manifested by the following symptoms: within a few minutes, the heart rate increases sharply and can reach 150-200 beats per minute, accompanied by sweating, weakness, and a feeling of fear.
What to do if your heart rate suddenly increases
When the pulse quickens for no apparent reason, it causes fear and anxiety. The main thing in such a situation is not to be nervous and try to determine what is happening in the body. If tachycardia remains the only symptom, you should breathe deeply and remain calm. Warning signs may include pain in the heart area that radiates to the neck or arm, as well as numbness and trembling of the limbs. In most cases, they are absent, and you can calm your heartbeat at home quickly, thanks to several useful methods.
Medicines
In many home medicine cabinets you can find drugs to reduce heart rate. They are available without a doctor's prescription and will help you quickly restore your performance. However, before taking them, it is important to find out the cause of this symptom, since different groups of drugs have different compositions and are indicated for tachycardia of different origins. So, the doctor may recommend the following medications:
- Valocordin, Corvalol - drugs based on phenobarbital and plant extracts, available in the form of drops that need to be diluted in water;
- valerian officinalis - comes in the form of drops and tablets, it helps well with tachycardia caused by nervous tension;
- rosehip or hawthorn fruits, motherwort root - raw materials for the preparation of soothing decoctions, useful for calming the heartbeat;
- if necessary, medications to replenish potassium or magnesium deficiency (Asparkam, Panangin).
IMPORTANT! After taking medications, you should avoid physical activity. It is better to spend this day in a calm environment, avoiding stress and nervous tension.
Corvalol or its analogues should be present in any home medicine cabinet
Cold water
Another way to lower your heart rate is to sharply lower your temperature. The easiest way to do this is with cold water. It is important that the body reacts most quickly to cooling the skin of the face, so it is not necessary to douse yourself completely. It is enough to immerse your face in a container of cold water or use a spray bottle. At home, you can also take an ice cube and wipe your face and temples with it. At the same time, you should monitor your breathing - take deep breaths and exhales.
Gymnastics
You can quickly calm your heartbeat even if you don’t have a first aid kit with medications on hand. One of the simplest and most accessible methods is breathing exercises. Its effectiveness is explained by the basic principles of the cardiovascular system. The pulse speeds up when cells are starved of oxygen and the heart has to pump faster to push out more blood. An increased heart rate leads to increased stress on organs and tissues, which increases the need for oxygen. For this reason, an increase in heart rate is often observed in hot and stuffy rooms.
This circle must be broken in order to normalize the functioning of the heart. The gymnastics are simple and can be performed independently:
- ventilate the room or go outside (in the heat - find the coolest area);
- inhale deeply while raising your arms up - this way a larger volume of oxygen enters the lungs;
- exhale deeply while lowering your arms down.
The exercise is performed slowly, and it is important to focus on breathing. You can also count the number of breathing cycles. It must be repeated until the pulse returns to normal. It is important to understand that if you return to a stuffy, gas-filled room, the attack may recur. For frequent manifestations of tachycardia, it is recommended to frequently ventilate the rooms, as well as install humidifiers and air filters. If the attack cannot be stopped, you should quickly calm the pulse with drugs, and then undergo examination by a doctor.
Breathing exercises also include the prevention of diseases of the cardiovascular system
Valsalva maneuver
This technique is designed specifically to quickly lower your heart rate without taking drugs. Its main goal is to influence the vagus nerve, which is responsible for heart rate. The exercise is performed as follows:
- take a deep breath, while tensing your abdominal muscles;
- pinch your nose with your fingers, close your eyes and mouth;
- in this position, try to exhale the air without relaxing the abdominal muscles.
IMPORTANT! This exercise, like others, is contraindicated in case of acute cardiac dysfunction. Chest pain, numbness of the limbs, dizziness, loss of consciousness - with these symptoms you should not try to reduce your heart rate on your own.
Massage
With the help of massage, you can influence certain areas that are located along the vagus nerve. It belongs to the parasympathetic system and also affects a person’s heart rate. These techniques are simple, but it is important to do them correctly and take your time and not apply too much pressure.
- Massage of the sinocarotid zone. It is located in the neck area, just below the lower jaw. At this point there is a branch of the carotid artery. Use your thumb to press on this point on the left and right sides for 3–5 minutes. This massage simultaneously equalizes heart rate and blood pressure.
- The eyeballs are an area in which a huge number of nerve endings are concentrated. It is enough to close your eyes and gently press them with your fingers for several minutes, and there should be no pain. If necessary, you can open your eyes, slowly look in different directions and repeat the procedure.
You can perform the massage yourself. In this case, you should take a comfortable position and monitor your breathing. Positive changes should be observed within the first 3-10 minutes. If they do not appear, the only way to calm the heart is with medications - your doctor will tell you what to take in each specific case. First aid drugs are Corvalol and Valocordin.
How to relieve an attack of tachycardia?
Unbutton your clothing collar, open a window or balcony, inhale deeply and exhale very slowly; breathe like this for 5-10 minutes. Then hold your breath and, as it were, “push” the air into the lower abdomen - this stimulates the vagus nerve, as a result of which the heartbeat will slow down;
Take Corvalol or Valocordin: dissolve 15-20 drops of the drug in half a glass of water at room temperature;
Wash your face with cold water, lie down on a high pillow, place a towel soaked in cold water on your forehead, try to relax;
Close your eyes and simultaneously press on your eyeballs for 2-3 minutes: press for 10 seconds, break for 10 seconds;
Find the right carotid artery (immediately under the jaw, at this point it connects to the cervical artery) and gently, without pressure, massage it. This technique also stimulates the vagus nerve and slows the heart rate.
If the condition does not improve, the heart rate does not decrease, dizziness appears, a feeling of shortness of breath, darkened vision, call an ambulance.
What is the danger
In addition to unpleasant and uncomfortable sensations, tachycardia can lead to conditions that are more dangerous to health and life. As a result of inadequate work, the heart muscle wears out faster, which entails a number of complications. These include:
- Acute and chronic left ventricular failure (cardiogenic edema and cardiac asthma).
- Arrhythmias of various origins.
- Cardiac conduction disorders.
- Arrhythmic shock.
- Transient cerebrovascular accidents and strokes.
- Increased thrombus formation, which, in turn, can provoke myocardial infarction and pulmonary embolism.
Disease prevention
In order for not only the heart, but also the entire body to be strong and healthy, you must first normalize your diet. It is necessary to exclude all caffeine-containing drinks, as well as chocolate, fried foods and reduce the amount of sugar. The best diet is plant-based and dairy. Fruit juices and fresh vegetables are beneficial. Vitamin complexes will help reinforce the effect of the diet. The child must take magnesium and potassium, which normalize the heart rate. Consult your doctor first. And be sure to include moderate physical activity in your child’s daily routine, such as morning exercises. It stimulates the heart and increases its resistance to the release of excess adrenaline. As a result, irritability decreases and the emotional background normalizes. At the same time, you should not overexert yourself; any activity should be moderate. Swimming, for example, is very useful.
Sources:
- E.L. Boqueria. Ectopic atrial tachycardia in children: clinical picture, diagnosis and treatment // Annals of Arrhythmology, 2006, No. 3, pp. 16-19.
- A.I. Safina, I.Ya. Lutfullin, Z.A. Gainullina. Heart rhythm disturbances in newborns // Practical Medicine, November 2010, No. 6(45), pp. 75-79.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6595346/ Ranjit I. Kylat and Ricardo A. Samson. Permanent junctional reciprocating tachycardia in infants and children // J Arrhythm. 2021 Jun; 35(3): 494–498.
- L.A. Balykova, I.S. Nazarova, A.N. Silence. Treatment of cardiac arrhythmias in children // Practical Medicine, September 2011, No. (53), pp. 30-37.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.