Most often, heart disease is the result of inflammation, tumor or vascular damage. In many cases, when the cause of cardiac pathology is too vague or cannot be established, a diagnosis of cardiomyopathy is made. We are talking about a whole group of diseases that affect people regardless of age and gender, which was classified and sufficiently studied only in 2006. Effective methods for diagnosing and treating various types of cardiomyopathy have now been developed. The CBCP Center for Pathology of the Circulatory Organs also uses the latest technologies in this area.
What is cardiac cardiomyopathy?
This is a group of diseases affecting the myocardium with unclear causes. To make a diagnosis, it is necessary to ensure the absence of congenital heart defects, valves, blood vessels, arterial hypertension, pericarditis, etc. Depending on the type of damage to the heart muscle, dilated, hypertrophic, restrictive and arrhythmogenic forms of this disease are classified. The classification depends on the characteristics of the circulatory disorder in the heart. Using high-quality equipment, all types of cardiomyopathy are diagnosed at an early stage.
Causes of primary and secondary cardiomyopathies
Depending on the causes, primary and secondary cardiomyopathy are distinguished. The causes of the primary disease are divided into 3 groups.
- Congenital ones develop even at the stage of formation of myocardial tissue in the embryo due to the bad habits of the mother, nutritional disorders, and stress.
- Acquired are the result of exposure to viruses, metabolic disorders, and toxic substances.
- Mixed ones combine one or more of the above reasons.
Primary cardiomyopathy is common in children. It can be not only congenital, but also acquired under the influence of reasons leading to disruption of the development of myocardial cells.
A secondary disease develops as a result of exposure to internal or external factors or other pathology. These include:
- accumulation of various pathological inclusions by cells;
- medications, in particular certain antitumor drugs;
- alcohol in large quantities and with prolonged use;
- metabolic disorders in the myocardium as a result of endocrine pathologies;
- unhealthy diet, obesity, diabetes, gastrointestinal diseases;
- long-term diets that cause a lack of vitamins and nutrients.
In Russia, mortality due to secondary cardiomyopathy is an extremely common phenomenon. And since the reasons themselves are very diverse, a high-quality and professional examination is necessary in each individual case.
Cardiomyopathy: symptoms
You may not notice the symptoms of this disease, since they are often not clearly expressed, and in some cases complications become noticeable. However, if cardiac cardiomyopathy has already manifested itself, it is difficult not to notice it.
- During intense physical activity, you feel short of breath and short of air.
- Long-term aching pain in the chest appears.
- Weakness and dizziness are noticeable.
- Constant swelling of the legs, sleep disorders, frequent fainting conditions.
These symptoms indicate disturbances in the contraction of the heart and problems with its blood supply. Contact your cardiologist immediately when they first appear!
Classification of cardiomyopathies and prognosis
As mentioned above, there are 2 main types of cardiomyopathy – primary and secondary. In turn, primary pathology is classified as follows:
- With a dilated cavity, the hearts expand, systolic function and cardiac output are impaired, and heart failure develops. This type is also called “ischemic cardiomyopathy”.
- With hypertrophic , the wall of the ventricles thickens by 1.5 cm or more. Depending on the nature of the lesion, there are symmetrical and asymmetrical, obstructive and non-obstructive forms.
- Restrictive cardiomyopathy can be obliterative or diffuse. The form depends on the nature of the disturbances in the contractile function of the heart muscle, which lead to a lack of blood volume in the chambers of the organ.
- Arrhythmogenic dysplasia is an uncommon phenomenon and is caused by large deposits of fat that lead to arrhythmia. This pathology is also called Fontan's disease.
Secondary cardiomyopathy of the heart is classified depending on the causes that caused it:
- alcoholic;
- diabetic;
- thyrotoxic;
- stressful.
As is clear from the names themselves, the causes of these forms of the disease are alcohol, diabetes or obesity, thyroid pathologies or stress.
Diagnostics
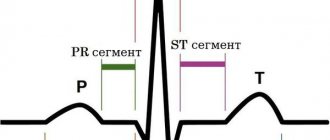
Diagnosis of cardiomyopathy necessarily includes a description of the clinical picture and data from additional studies. The most common method - electrocardiography (ECG) - allows you to record signs of hypertrophy of the heart muscle and identify various forms of rhythm and conduction disorders. Echocardiography (EchoCG) is especially informative, as it helps determine myocardial dysfunction. Thanks to X-ray data, dilatation (persistent increase in the lumen), hypertrophy (increase in volume and mass) of the heart muscle, as well as congestion in the lungs are detected. In some cases, as part of the diagnosis of cardiomyopathy, ventriculography (x-ray examination of the ventricular system), magnetic resonance imaging (MRI) of the heart and multislice computed tomography (MSCT), as well as probing of the cavities of the heart to collect biomaterials for further morphological research are indicated.
Dilated cardiomyopathy (ischemic)
This type of cardiomyopathy is also called “congestive” or “ischemic” - due to a significant deterioration in blood circulation in the dilated chambers of the heart. A common cause (up to 20% of cases) of the development of pathology are:
- changes at the genetic level;
- various immune system failures;
- intoxication and infection.
In some cases, it is believed to be a familial disease. And it can appear by the age of 30.
The symptoms of dilated (ischemic) cardiomyopathy coincide with the general symptoms of heart failure. If you experience shortness of breath during exercise, you quickly get tired, notice swelling, pale skin, blue fingertips - you should immediately go for an ultrasound of the heart (echocardiography). This method is the most informative in this case. The examination also reveals atrial fibrillation.
With advanced disease, the prognosis is disappointing: mortality in ischemic cardiomyopathy reaches 70% in the first 5 years after the onset of pathology. Only timely intervention by cardiologists, a well-designed treatment program, and high-quality drug therapy (ACE inhibitors, beta blockers, etc.) can significantly prolong life.
In the future, your lifestyle will have to be adjusted. In particular, women with dilated ischemic cardiomyopathy are strictly not recommended to become pregnant, as this is one of the most common causes of a sharp deterioration in health.
Causes
The etiology of this pathology has not been fully studied to date. There are a number of probable causes that can cause the development of cardiomyopathy:
- hereditary predisposition (genetic defect that causes improper formation and functioning of myocardial muscle fibers);
- various viral infections (Coxsackie, herpes, influenza, etc.);
- previous myocarditis;
- damage to heart cells by toxins and allergens;
- disturbances of endocrine regulation (negative effects of growth hormone and catecholamines);
- immune system disorders.
Hypertrophic cardiomyopathy
This type of pathology is manifested by enlargement and hypertrophy of cardiac tissue in the left ventricle (enlargement of the right ventricle can also occur, but is extremely rare).
- In this case, a clear asymmetry develops in the heart: for example, the ventricular cavity is significantly reduced, and the left atrium expands.
- Diastolic filling of the ventricle occurs with disturbances and diastolic function is insufficient.
- Part of the ventricle, as well as the interventricular septum, may hypertrophy.
- Due to an increase in diastolic pressure in the pulmonary veins, gas exchange in the lungs is disrupted.
The disease also very often manifests itself in 30-year-old patients. The later stages are characterized by shortness of breath (in 90% of cases), arrhythmia and angina pectoris, and the pressure at the outlet of the left ventricle can rise to 185 mm Hg. Therefore, the main diagnostic methods for this type of cardiomyopathy are various types of ECG and ultrasound of the heart.
Characteristic symptoms include prolonged chest pain, which is typical of angina. During physical exertion, the patient may faint. Blood circulation in the brain also suffers, which is manifested by brief deterioration in attention, memory, and speech.
The prognosis of cardiomyopathy is quite negative if the stage of the disease no longer allows for positive changes in the functioning of the heart. If the diagnosis is made on time and treatment is started in the early stages, then through drug therapy (beta-blockers, diuretics, etc.) it is possible to prolong the patient’s life for a sufficiently long period.
Cardiomyopathies in children
T.A. RUZHENTSOVA
, Candidate of Medical Sciences,
Central Research Institute of Epidemiology of Rospotrebnadzor, Moscow The article summarizes data on the modern classification, causes and methods of diagnosing cardiomyopathies in children.
Various options for clinical symptoms, electrocardiographic, echocardiographic and biochemical changes are considered. The significance of the results of additional examination methods for cardiomyopathy is assessed. Introduction
Currently, non-coronary heart pathology remains one of the most difficult problems in pediatrics and cardiology. With the development of high-tech diagnostic and treatment methods over the past century, significant improvements in prognosis and an increase in life expectancy in patients with coronary heart and brain disease have been noted. However, morbidity and mortality from myocarditis and cardiomyopathies remained at the same level [1]. According to pathological studies, only about a quarter of cases are diagnosed during life [2]. Among those who died from sudden death syndrome between the ages of birth and 18 years, non-coronarogenic changes in the myocardium are found with a frequency of 20–40% [2–6]. A significant obstacle to the timely formulation of a correct diagnosis is the widespread use both in practice and in the literature of terms that are not included in the International Classification of Diseases, X Revision (ICD X), such as “cardiopathy” and “myocardial dystrophy.” The lack of unambiguous generally accepted diagnostic algorithms and management schemes for this category of patients leads to progression of the disease without adequate treatment and, in some patients, to death.
Terminology issues
The term “cardiomyopathy” was first used in 1957 to designate myocardial diseases of unknown etiology, accompanied by heart failure, cardiomegaly, progressive course and fatal outcome [7]. Later, combined cardiac lesions involving the pericardium and/or endocardium were also included in this pathology. In 1961, Goodwin proposed to distinguish acute, subacute and chronic course. In 1980, a WHO expert committee approved a classification dividing cardiomyopathies into dilated, hypertrophic and restrictive. To denote secondary myocardial changes not associated with damage to the coronary arteries, the term “myocardial dystrophy” has become widespread in the domestic literature. However, with the accumulation of results from high-tech methods for diagnosing myocardial diseases over the past decades, ideas about these nosologies have undergone significant changes. In many cases previously considered idiopathic, according to endomyocardial biopsy, the infectious, autoimmune or dysmetabolic nature of the changes was established [7]. Viral agents and inflammatory infiltration are found in most patients with dilated cardiomyopathy and in some patients with other forms. Dystrophic changes in the myocardium, determined by a decrease in the activity of succinate dehydrogenase, a decrease in glycogen, destruction of myofibrils and mitochondria, often accompany typical leukocyte infiltration in neighboring areas. Sometimes the typical signs of dystrophy after a few days or weeks are replaced by inflammatory ones [8–10]. These data made it possible to identify infectious cardiomyopathies as a separate group. The discovered other changes in cardiomyocytes with corresponding nosologies dictated the need to add arrhythmogenic, peripartum (postpartum), metabolic, autoimmune, and toxic cardiomyopathies to the classification. Thus, today, according to the current ICD X, the following types of cardiomyopathy are distinguished [7, 11]:
I. Idiopathic (dilated - I42.0, obstructive hypertrophic - I42.1, non-obstructive hypertrophic - I42.2, restrictive - I42.5). II. Specific (infectious - I43.0, metabolic - I43.1, with nutritional disorders - I43.2, alcohol - I42.6, with the influence of drugs and other external factors - I42.7, with other diseases - I43.8). Cardiomyopathies include endomyocardial (eosinophilic, Loeffler's endocarditis, endomyocardial, or tropical fibrosis) disease (I42.3) and endomyocardial fibroelastosis (I42.4). Postpartum – O90.3 and cardiomyopathy during pregnancy – O99.4 are included in a separate category.
Idiopathic processes in the myocardium are most often caused by inherited genetic abnormalities or spontaneous mutations leading to disruption of the structure and function of myofibrils.
Today, many specialists dealing with the problems of non-coronary heart diseases have recognized the fact of the staged nature of infectious and inflammatory changes with the transformation of myocardial dystrophy into acute myocarditis, and then, in an unfavorable course, into dilated cardiomyopathy [12–16]. It is not always possible to determine a clear boundary between different types of cardiomyopathies, since there are signs of two or more influencing factors. With specific processes, the ultrasound picture often corresponds to dilated, hypertrophic or restrictive cardiomyopathy. One type can change into another over time. In many cases, it is almost impossible to draw a clear line between myocarditis and cardiomyopathy.
Due to the complexity of diagnosing non-coronary myocardial diseases not only in Russia, but also in other developed countries of Europe and America, the non-specificity of symptoms and the current lack of generally accepted diagnostic criteria, the WHO expert committee in 1997 proposed to use the term inflammatory cardiomyopathy in practice - “ inflammatory cardiomyopathy" [11, 17]. They are recommended to designate all cases of infectious myocardial lesions, their consequences, all acute and chronic myocarditis, including autoimmune, all cases of dilated cardiomyopathy [11, 14, 17, 18]. Inflammatory cardiomyopathy, depending on the predominant pathogenesis, has been proposed to be divided into three forms: infectious, autoimmune and idiopathic. In chronic processes, which, in accordance with WHO recommendations, should be classified as secondary cardiomyopathies, replacement and interstitial fibrosis, hypertrophy of muscle fibers with areas of destruction and focal mononuclear infiltrates are revealed.
Clinical picture of the disease in children
Cardiomyopathy can manifest at any age. All manifestations can be expressed to varying degrees. Some children feel quite well, without making any complaints and without causing concern to their parents [7]. Common symptoms may include lethargy, weakness, fatigue, sleep disturbances, lack of appetite, sweating, dizziness, headaches and muscle pain. Parents often note excessive capriciousness of the child, and sometimes significant disturbances in behavior and perception [19, 20]. Insufficient blood supply to the brain, which develops as a result of a low ejection fraction, may be accompanied by convulsions and fainting. There is isolated evidence that with a long course of myocarditis or cardiomyopathy in children, delayed psychomotor development is noted [13].
Patients may complain of shortness of breath during exercise, and sometimes at rest, palpitations. Associated rhythm disturbances, which can give sensations of interruptions and pauses in the work of the heart, episodes of tachycardia or tachyarrhythmia lead to an increase in symptoms of heart failure [13, 21]. The pain has a different character: stabbing, aching, and when there is insufficient blood supply to the myocardium, pressing. In some patients, the pain syndrome may be mild and feel like discomfort. Damage to the posterior diaphragmatic parts of the left ventricle can cause pain in the upper abdomen, nausea, and vomiting, which often represents a rather difficult differential diagnostic task, especially when abdominal and cardiac pathologies are combined. A decrease in blood supply to the abdominal organs due to a decrease in the ejection fraction of the left ventricle leads to an increase in stool up to 5 times, and in children under 1 year of age up to 10 times a day [13, 19]. The stool, as a rule, becomes unformed; in severe myocarditis or cardiomyopathy, streaks of blood may appear. The pain syndrome can spread to all parts of the abdomen. With prolonged course, constipation may occur as a result of the development of ischemic colitis. An increase in pressure in the vascular bed of the pulmonary circulation against the background of a decrease in the pumping function of the left parts of the heart leads to the appearance of a cough in these children, which can be either dry or wet with the discharge of a small amount of whitish sputum [13]. The severity of manifestations of heart failure, as a rule, determines the prognosis in such children.
When examining the patient, changes in the skin characteristic of heart failure are revealed: pallor, acrocyanosis, marbling. In severe cases, there may be swelling of the legs. If the child is in a horizontal position most of the time, then the swelling spreads to the lumbar region, the anterior abdominal wall, arms and face [22, 23]. When palpating the area of the cardiac impulse, its shift to the left and weakening are noted, which indicates an expansion of the cavities of the heart. Percussion is determined by an increase in absolute dullness, mainly to the right, due to the right ventricle, which is more often involved in the infectious process in children, and/or an expansion of the boundaries of relative dullness to the left by 1–2 cm due to hypertrophy or dilatation of the left ventricle. An upward increase in the boundaries indicates involvement of the left atrium in the process. In some cases, the right border of the relative dullness of the heart is determined in the form of a steep arc with a shift to the right, which indicates changes in the right atrium. Dystrophic and hypoxic damage to the myocardium can, like inflammatory ones, lead to a decrease in ventricular contractility and expansion of the chambers of the heart. With adequate therapy, these patients experience rapid normalization of size. However, the lack of timely correction of disorders can lead to the destruction of cardiomyocytes and the formation of irreversible foci of cardiosclerosis. Auscultatory symptoms may vary. In the initial period of the infectious-inflammatory process in the myocardium, pronounced loudness and clarity of tones are characteristic, which is often interpreted as a sign of good condition of the heart muscle. However, when analyzing phonocardiograms, it was found that the basis of these changes is the weakening of myocardial vibration and the coming to the fore of the sound generated as a result of the movements of the valve leaflets. The progression of changes causes a weakening of the first tone at the apex and in the projection of the tricuspid valve against the background of accentuation of the second tone over the pulmonary artery due to a decrease in the performance of the heart muscle and a decrease in blood pressure. A three-part gallop rhythm may appear. Further development of the disease causes muting or deafness of all tones. The exception is hypertrophic cardiomyopathy, for which weakening of the first tone is not typical.
Various forms of cardiac lesions are often accompanied by the appearance or change of pre-existing systolic and/or diastolic murmur [13, 19, 24]. The murmur, resulting from relative mitral valve insufficiency due to left ventricular dilatation and distension of the left atrioventricular ring, is best heard in the fourth intercostal space to the left of the sternum. Systolic murmur in the second - third intercostal space to the right of the sternum, usually less intense, is associated with regurgitation on the tricuspid valve as a result of dilatation of the right ventricle. It is characterized by a scraping character, a small area of distribution and a clear dependence on the phases of breathing: weakened when inhaling and strengthened when exhaling. Diastolic murmurs are heard less frequently and are characterized by low intensity. During dilatation, they arise due to stretching of the fibrous rings of the aortic and pulmonary openings and, as a consequence, secondary insufficiency of one or both semilunar valves.
Cardiomyopathies are often accompanied by various rhythm disturbances: extrasystole; tachycardia that does not correspond to the body temperature and emotional state of the child; bradycardia. More severe forms are accompanied by pronounced tachyarrhythmias or bradyarrhythmias, the nature of which must be clarified based on the results of an electrocardiographic study. Sometimes small lesions in the area of pacemakers or pathways can cause severe life-threatening arrhythmias. Possible paroxysmal tachycardia, atrial flutter and fibrillation, group and polytopic extrasystole, complete atrioventricular block, ventricular fibrillation. Regardless of the etiology, these conditions are always accompanied by heart failure to varying degrees and, in some cases, cardiogenic shock.
Symptoms of myocardial damage include circulatory failure, manifested by hypotension and pulmonary congestion with decreased contractility of the left ventricle, as well as hepatomegaly when the right ventricle is involved in the process. The auscultatory picture of congestive left ventricular failure is characterized by weakening of breathing in the lower parts of the lungs with the appearance of moist rales there, which often dictates the need for differential diagnosis of myocarditis, cardiomyopathy and pneumonia. When the patient is in a predominantly horizontal position during the day, wheezing can be heard in small or moderate amounts in all areas of auscultation.
Diagnosis of the disease
To clarify the diagnosis and determine treatment tactics, it is necessary to use additional examination methods. Electrocardiograms (ECG) record various disturbances in excitability, conduction, de- and repolarization, signs of overload or hypertrophy of one or more chambers of the heart. Daily monitoring allows us to identify transient rhythm disturbances and indirectly assess the degree of insufficiency of myocardial blood supply during physical activity.
Based on the results of echocardiography, the diagnosis of cardiomyopathy can be confirmed in the presence of hypertrophy, a decrease in the contractility index of the left ventricle - ejection fraction and expansion of the heart chambers with an increase in end-systolic and/or end-diastolic dimensions and/or volumes of the left ventricle [11, 18]. The earliest manifestation of myocardial dysfunction is diastolic dysfunction of one or both ventricles [11, 23, 24]. However, a number of authors note the fact that a normal echocardiographic picture today does not exclude the diagnosis of cardiomyopathy [19, 25].
In a biochemical blood test, some patients may experience an increase in the MB fraction of creatine phosphokinase, α-hydroxybutyrate dehydrogenase, aspartic transaminase, troponin I or T. In autoimmune processes, antibodies to the myocardium can be detected.
Endomyocardial biopsy is considered the gold standard for diagnosing cardiomyopathy [11–13, 23]. But, according to the majority of foreign and Russian researchers, it does not provide a complete guarantee of an accurate diagnosis, since there is a high probability of histological examination of unchanged areas, incorrect timing of the study, or difficulties in interpreting the resulting picture. According to the recommendations of leading cardiologists, this method cannot be considered absolutely necessary for diagnosing cardiomyopathies, especially in pediatric practice.
The results of modern high-tech methods: magnetic resonance imaging with paramagnetic contrast agents, myocardial tomoscintigraphy, positron emission tomography - can be useful in doubtful situations.
Thus, cardiomyopathy in most patients is secondary in nature; different forms have similar symptoms. The diagnosis can be made based on the clinical picture, ECG results, echocardiography and laboratory data. . Bibliography
1. Gaziano JM. Global burden of cardiovascular disease. Braunwald E, Zipes P, Libby P, eds. Heart Disease: A Textbook of Cardiovascular Medicine. Philadelphia, 2005: 1–19. 2. Basso C, Calabrese F, Corrado D, Thiene G. Postmortem diagnosis in sudden cardiac death victims: macroscopic, microscopic and molecular findings. Cardivasc. Res. 2001. 50: 290–300. 3. Dancea A, Cote D, Rohlicek C et al. Heart pathology in unexpected sudden death in young children. Issues of modern pediatrics. 2002. 1. 6: 15–20. 4. Doolan A, Langlois N, Semsarian C. Causes of sudden cardiac death in young Australians. Med. J. Aust. 2004. 180: 110–112. 5. Larsson E, Wesslen L, Lindquist O et al. Sudden unexpected cardiac death among young Swedish orienteers-morphological changes in heart and other organs. APMIS. 1999. 107 (3): 325–336. 6. Matturi L, Ottaviani G, Kamos SG, Rossi L. Sudden infant death syndrome (SIDS); a study of cardiac conduction system. Cardiovascular Pathology. 2000. 9 (3): 137–145. 7. Mutafyan O.A. Cardiomyopathies in children and adolescents. O.A. Mutafyan. St. Petersburg: Dialect, 2003. 8. Maksimov V.A., Finogeev Yu.P., Balyabin A.A. Infectious lesions of the myocardium. Abstracts of reports of the scientific conference of the III Congress of the Italian-Russian Society for Infectious Diseases “Infectious diseases: new in diagnosis and therapy.” St. Petersburg, 1998. 60. 9. Gravanis MB, Sternby NH Incidence of myocarditis. A 10-year autopsy study from Maimo, Sweden. Arch. Pathol. Lab. Med. 1991. 115: 805–812. 10. Hauck AJ, Kearney DL, Edwards WD. Evaluation of postmortem endomyocardial biopsy specimens from 28 patients with lymphocytic myocarditis: implications for the role of sampling error. Mayo Clinic Proc. 1989. 63: 1235–1245. 11. Deryugin M.V., Boytsov S.A. Chronic myocarditis. St. Petersburg: [ELBI-SPb], 2005. 288. 12. D'Ambrosio A, Patti G, Manzoli A et al. The fate of acute myocarditis between spontaneous improvement and evolution to dilated cardiomyopathy: a review. Heart. 2001. 85: 499–504. 13. Calabrese F, Rigo E, Milanesi O et al. Molecular diagnosis of myocarditis and dilated cardiomyopathy in children: clinicopathologic features and prognostic implications. Diagn. Mol. Pathol. 2002. 11. 212–221. 14. Mason JW et al. Myocarditis. Willerson JT, Wellens HJJ, Cohn JN, Holmes DR. Cardiovascular Medicine, 3rd edition Springer. 2007. 1: 1313–1347. 15. Burian J, Buser P, Eriksson U. Myocarditis: the immunologist's view on pathogenesis and treatment. Swiss Med. Wkly., 2005, 135 (25–26): 359–364. 16. Kovalenko V.M., Ilyash M.G., Bazika O.I. Myocarditis: current aspects of pathogenesis and diagnosis. Ukr. rheumatol. zhur., 2001, 1: 56–61. 17. Karatolios K, Pankuweit S, Kisselbach C, Maisch B. Inflammatory cardiomyopathy. Hellenic. J. Cardiol. 2006. 47 (2): 54–65. 18. Boytsov S.A., Deryugin M.V. Non-rheumatic myocarditis. Guide to cardiology: textbook. manual in 3 volumes, ed. G.I. Storozhakova, A.A. Gorbachenkova. M., 2008. 2: 116–145. 19. Park MK, Troxler RG. Pediatric cardiology for practitioners. 4th ed. St. Louis, Mosby: 2002: 289–290. 20. Wang ZX, Xu L, Wang YL et al. Mentality and behavior of children suffering from viral myocarditis. Zhonghua Er Ke Za Zhi (Chinese journal of pediatrics). 2006. 44: 122–125. 21. Basargina E.N. Cardiomyopathies. Selected lectures on pediatrics. Ed. Baranova A.A., Shilyaeva R.R., Kasanova B.S. M., 2005: 201–208. 22. Belozerov Yu.M. Pediatric cardiology. M., 2004. 597. 23. Tobias JD, Deshpande JK, Johns JA, Nichols DG. Inflammatory heart disease. Nichols DG, Ungerleider RM et al, Critical Heart Disease in Infant and Children. 2nd ed., Philadelphia, PA: Mosby. 2006: 899–925. 24. Ruzhentsova T.A., Gorelov A.V. The significance of acute respiratory viral infections in the development of chronic heart pathology in children. Epidemiology and infectious diseases. 2012, 3: 42-46. 25. Rybakova M.K., Alekhin M.N., Mitkov V.V. Practical guide to ultrasound diagnostics. Echocardiography. M., 2008. 544.
Restrictive cardiomyopathy
This species is quite rare in medical practice and has therefore been little studied. In this case, the walls of the myocardium become too rigid, do not stretch and lose the ability to enter the relaxation stage. In this case, there is no thickening of the myocardial walls or enlargement of the ventricle, as with other types of cardiac cardiomyopathy.
The elasticity of the heart muscles decreases. The body begins to retain excess fluid. As a result, oxygen, along with the blood, flows worse and in insufficient quantities into the left ventricle. Pathology leads to disruption of general blood circulation and poor blood supply to various organs.
It occurs in young people and children, often in combination with other diseases caused by metabolic disorders. Diagnosis is difficult, since the pathology manifests itself already at the stage when heart failure develops with its typical symptoms. It is for this reason that treatment does not always begin on time, so the prognosis in some cases may not be too optimistic.
For diagnosis, the most valuable information is obtained during cardiac ultrasound (echocardiography). Laboratory tests may reveal eosinophils (white cells) and deposits of amyloid (a complex of protein and carbohydrate) in the internal organs.
Arrhythmogenic cardiomyopathy
This cardiomyopathy is also called right ventricular - due to the specific location of the pathological changes. It develops mainly against the background of bradycardia, tachycardia or other types of chronic arrhythmia. The disease is quite rare, its frequency is 1:5000 of all cases of cardiac cardiomyopathy, and the causes are not completely clear to medicine.
The pathology is that the myocardium of the right ventricle is gradually replaced by fat or connective tissue. In rare cases, the left ventricle may also be partially affected, while the interventricular septum remains healthy.
This type of pathology is also often familial in nature, can be inherited by close relatives and manifests itself already in adolescence. There is a classification of arrhythmogenic cardiomyopathy:
- disease in its pure form;
- Naxos disease, accompanied by malignant ventricular arrhythmia;
- Venetian form with involvement of the left ventricle and manifestation in childhood;
- Pokkuri disease with ECG changes;
- benign right ventricular extrasystoles;
- Uhl's anomaly with a complete absence of muscle fibers in the myocardium;
- biventricular dysplasia affecting both ventricles;
- dysplasia with complications in the form of myocarditis.
Most patients, if treatment is started in a timely manner, will undergo lifelong monitoring by a cardiologist with drug therapy.
Secondary cardiomyopathies of the heart
This group includes pathologies whose causes lie in physical and chemical disorders in the body that provoke changes in the heart muscle.
- Alcoholic cardiomyopathy is a consequence of the effect on the myocardium of ethanol, which forms the basis of alcoholic beverages. As a result, adipose tissue appears in the myocardium.
- Thyrotoxic is caused by dysfunction of the endocrine system, lack of treatment for thyrotoxicosis. One of the common manifestations is dyshormonal cardiomyopathy during puberty or during hormonal therapy.
- Toxic is another type of secondary cardiomyopathy associated with the effects of various toxic substances on the heart tissue: lithium, cobalt, etc. They cause inflammation and microinfarctions.
- Stress is accompanied by a decrease in myocardial contractions and weakness due to emotional, mental influences, and shocks.
- Diabetic appears when diagnosed with diabetes mellitus and leads to biochemical changes in the myocardium and the accumulation of various polysaccharides.
The prognosis for each type of secondary cardiomyopathy depends on the success of treatment not only of the pathology itself, but also of the diseases that caused it: diabetes mellitus, thyrotoxicosis, alcohol addiction, etc. These are extremely difficult cases, but with a professional approach, the patient’s life expectancy can be maximized.
Treatment
Due to the lack of specific therapy, treatment of cardiomyopathy is aimed at preventing complications incompatible with life. If the disease is in a stable phase, all measures are prescribed and carried out on an outpatient basis. Must be under the supervision of a cardiologist. The indication for periodic planned hospitalization is the presence of severe heart failure, for emergency - the development of intractable paroxysms of arrhythmias, as well as thromboembolism and pulmonary edema.
Drug treatment. For various manifestations of cardiomyopathy, it is advisable to prescribe:
- diuretics, which reduce pulmonary and systemic venous congestion;
- cardiac glycosides, which help combat disorders of contractility and pumping function of the myocardium;
- antiarrhythmic drugs that help regulate heart rhythm;
- anticoagulants and antiplatelet agents to prevent the occurrence of thromboembolic complications of cardiomyopathy.
Surgery. Indicated in extremely severe cases. Among the methods practiced today are septal myotomy (resection of an enlarged portion of the interventricular septum) and mitral valve replacement, as well as whole heart transplantation.
In addition, experts emphasize the need to reduce physical activity and adhere to a diet, an important condition of which is limiting the consumption of animal fats and salt. It is strongly recommended to eliminate bad habits and exposure to negative external factors. Compliance with these recommendations will significantly reduce the load on the myocardium and slow down the progression of heart failure.
Complications
- The main ones are heart failure and arrhythmias in their obvious clinical manifestations.
- When the walls of the ventricle expand, the heart valves stop working normally.
- Due to the large accumulation of fluid in the tissues and internal organs (lungs), edema appears.
- Embolism (formation of blood clots and blood clots) is an extremely dangerous complication that leads to heart attack and stroke.
- Sudden cardiac arrest is the most complex consequence of cardiomyopathy, which, in the absence of timely resuscitation, is fatal.
In order for the forecast to be as optimistic as possible, monitor your lifestyle and diet. And to avoid negative consequences, visit a qualified cardiologist as often as possible and undergo diagnostics using modern equipment.
Consequences and complications
For all types of cardiomyopathy, a characteristic complication is progressive heart failure. In addition, arterial and pulmonary thromboembolism, cardiac conduction disturbances, and severe forms of arrhythmia may develop. There is a high risk of sudden cardiac death. If the patient has bad habits, such as smoking and drinking alcohol, the prognosis worsens significantly. Life expectancy may also be affected by the presence of thromboembolism and tachycardia, especially if cardiomyopathy is untreated. Today, alleviating the course of the disease for such patients is becoming possible thanks to modern early diagnostic technologies.