Quail rhythm, 1 auscultation point
Svetlana Shcherbakova
Cardiologist
Higher education:
Cardiologist
Kabardino-Balkarian State University named after. HM. Berbekova, Faculty of Medicine (KBSU) Level of education – Specialist 1994-2000
Additional education:
“Cardiology”
State Educational Institution “Institute for Advanced Training of Physicians” of the Ministry of Health and Social Development of Chuvashia
Contacts
Physical examination, of which auscultation (listening to the heartbeat) is a part, has been and remains an important part of the diagnosis. When the heart is healthy, both parts work in sync, and its beating sound is crisp and clear. Some pathologies cause changes in healthy heart sounds due to the splitting of sounds. The three-part melodies of the heart have names - the rhythm of a quail and a gallop.
Heart sounds are normal
The heart, like any other organ, creates certain sounds when working. This is due to the fact that blood is constantly moving in the heart, passing through the valves, and the valve flaps open and close, emitting sound vibrations.
In addition, at the moment of stretching of the heart muscle of the atria and ventricles, vibration is created, which is layered with the sounds of slamming valve flaps.
Previously, it was believed that the first sound is formed when the atrioventricular valves close at the moment when blood flows from the atria into the ventricles, and then when the valves of the aorta and pulmonary trunk open, when blood flows from the ventricles into the aorta and into the pulmonary trunk. That is, the first sound characterizes the filling of the ventricles with blood and its expulsion further into large arteries.
However, since 2004 (E.
Braunwald) ideas about the nature of the origin of the first tone have changed somewhat - now it is generally accepted that such a sound is created not by the slamming of a valve, but by the impact of blood on the walls of the ventricle, when the blood first quickly fills the ventricles and then abruptly stops its movement. The first sound is systolic, as it indicates systole (contraction) of the ventricles. The second sound is diastolic, as it is caused by diastole (relaxation) of the ventricles.
The second sound is formed a few hundredths of a second after the first and is formed by sounds that are created by the closure of the valves of the aorta and pulmonary trunk, as well as the oscillatory movements of the walls of these arteries.
distribution of heart sounds in the cardiac cycle
– there – ta – there – ta – there – ta – I tone – II tone – I tone – II tone – I tone – II tone
Heart sounds and heart murmurs should not be confused. Between the two tones there are silent pauses, during which the blood flows directly, which normally occurs silently through the chambers of the heart.
However, with heart defects or other pathologies of the heart valves, the blood stream has difficulty expelling from the heart chambers corresponding to the defect, so sound phenomena called murmurs occur.
Noises can be heard in pauses between tones, or can be layered on top of them.
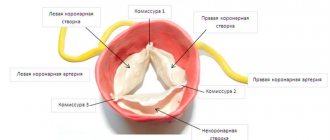
From the splitting of the second tone described above, which are usually heard only at the base of the heart, mainly at the pulmonary artery, one should distinguish a sound melody that only externally resembles the splitting of the second tone and is usually detected at the apex of the heart with mitral stenosis - the so-called quail rhythm or sound opening of the mitral valve - the so-called mitral click.
The rhythm of the quail, as V.P. Obraztsov called it, consists of a pronounced three-part melody of the heart, heard with mitral stenosis at the apex of the heart. In this case, the third, additional tone, auscultated shortly after the second, is thus heard in the initial part of diastole - protodiastole. This three-part rhythm resembles the sound made by a quail.
The reason for the quail rhythm, which can be heard not only directly by the ear, but also clearly through a phonendoscope, is the sound caused by the opening of a rigid, sclerotic bicuspid valve with mitral stenosis. This sound usually merges at the time of its occurrence with the third normal tone, which, layered on top of it, enhances this sound phenomenon.
The opening tone (sound) of the mitral valve, also called the opening click, is caused by tension when the rigid valve moves at the beginning of diastole from a convex position towards the atrium to a convex position towards the ventricle with good mobility of the mitral valve. The opening click is abrupt, hard, perceived as a loud echo behind the second tone. Sometimes the op is even more sonorous than the second tone.
With a sharp degree of stenosis, the opening click may be absent. Less commonly, it is also detected when mitral stenosis is combined with aortic valve insufficiency, with severe mitral valve insufficiency, and with a significant increase in pressure in the pulmonary vessels.
The difference between the sound of the opening mitral valve and the bifurcation of the second tone comes down to the following: 1) the place where it is heard is the region of the cardiac apex, and not the base of the heart (as with splitting or bifurcation of the second sound); 2) the rhythm of the quail is characterized by constancy (the splitting of the second tone can appear and disappear, intensify and weaken); 3) with the quail rhythm, although a short, but still pronounced gap is noted between the second and the third tone that follows it in protodiastole, the splitting of the second tone is often replaced by subsequent splitting, and the gap between the parts of the second tone cannot be clearly discerned. The quail rhythm with mitral stenosis is so characteristic of it that based on this phenomenon alone one can assume a narrowing of the left venous opening.
Interesting medical articles:
Source: https://klinika-krovi.ru/bolezni-serdca/ritm-perepela.html
Changes in heart sounds in pathology
Previously: heart sounds.
A change in heart sounds can primarily be expressed in a weakening or strengthening of the sonority of one or both of them, in a change in timbre, duration, in their splitting or bifurcation, in some cases - in the appearance of additional tones. In this case, determining the place of best listening to pathological sound phenomena is of diagnostic importance. Strengthening of the second tone in the 2nd intercostal space on the left
speaks of its emphasis on the pulmonary artery (determined by comparing its volume and timbre on the pulmonary artery and aorta).
This indicates an increase in pressure in the pulmonary circulation, which can be observed in diseases of the heart, as well as the respiratory system (mitral defects, emphysema, pneumosclerosis, chronic pneumonia). The intensification of the second tone in the second intercostal space on the right
indicates its emphasis on the aorta, which is observed with an increase in blood pressure in the systemic circulation (arterial hypertension), as well as in the case of hardening of the wall and valve of the aorta in atherosclerosis and a number of other diseases.
Strengthening the first sound at the apex of the heart
most often occurs with narrowing of the left atrioventricular orifice (mitral stenosis), tachycardia. This is due to the fact that with this defect, during diastole, less blood flows into the left ventricle than normal, and it contracts more quickly (transition from a relaxed to a tense state). In addition, with mitral stenosis, the timbre of the first tone changes due to vibrations of the sclerotic cusps of the mitral valve. It takes on a crackling tone, reminiscent of the sound of a flag flapping in the wind. This sound at the apex of the heart with mitral stenosis is called “popping”.
Weakening of the first sound at the apex of the heart
can be observed during inflammatory processes of its muscles (myocarditis), cardiosclerosis (scar changes in the heart muscle), and damage to the valve apparatus (bicuspid and tricuspid, as well as aortic).
Weakening of the second sound on the aorta
possible with aortic defects (aortic valve insufficiency or stenosis of its mouth).
Weakening of the second tone on the pulmonary artery
occurs when the valve is insufficient or its opening is narrowed (stenosis).
If during auscultation of the heart, instead of one of the tones, two short ones are heard, following each other after a short period of time, then this indicates a split tone
.
If the difference in the time of occurrence of these components is insignificant and the impression of splitting is not created, we are talking about tone splitting
. Thus, there is no fundamental qualitative difference between bifurcation and splitting of tones. There is only some quantitative difference: splitting is the initial phase, and bifurcation is a more pronounced degree of disruption of the unity of tones.
Bifurcation and splitting of tones can be physiological and pathological. For example, the bifurcation of the first tone may depend on the non-simultaneous closure of the bicuspid and tricuspid valves as a result of changes in pressure in the chest during different phases of breathing. But more often, a split in the first tone indicates pathological changes in the heart. It occurs, as a rule, when one of the legs of the atrioventricular bundle (bundle of His) is blocked, which leads to non-simultaneous contraction of the right and left ventricles of the heart. This can occur with significant blockade of the atrioventricular (atrioventricular) node, with sclerosis of the initial part of the aorta.
In case of severe heart damage, a three-part rhythm can be heard. It is caused by weakening of the myocardium (inflammation, degenerative changes, toxic lesions) of the left ventricle and occurs as a result of rapid stretching of its walls under the pressure of blood flowing from the atrium. This creates the melody of a three-part rhythm (first, second and additional third tones), reminiscent of the clatter of a galloping horse - the “ gallop rhythm.”
" It is also figuratively called the “cry of the heart for help,” since it is a sign of severe heart damage. The rhythm of the gallop is best heard directly by the ear (along with the sound, a slight impulse is perceived, transmitted from the heart to the chest in the diastole phase) in the area of the apex of the heart or the third-fourth intercostal space on the left. It can be heard especially clearly when the patient is lying on his left side. But this creates inconvenience for direct listening with the ear. In such cases, a phonendoscope is used.
There are protodiastolic, mesodiastolic and presystolic gallop rhythms (depending on the diastole phase, during which the pathological third sound appears).
gallop rhythm
an auscultatory finding of three (triple r.) or four (quadruple r.) heart sounds;
the extra sounds occur in diastole and are related either to atrial contraction (S), to early rapid filling of a ventricle (S), or to concurrence of both events (summation gallop) . Translation: The gallop rhythm
is heard as a three-part or four-part rhythm. Additional sounds appear in diastole and are caused either by atrial contraction, or early rapid filling of the ventricle, or a combination of both mechanisms (summation gallop).
Much more common are bifurcation and splitting of the second tone, caused by non-simultaneous closure of the pulmonary artery and aortic valves due to increased pressure in the pulmonary or systemic circulation. Bifurcation and splitting of the second tone can also be physiological and pathological.
Physiological splitting of the second tone is heard exclusively at the base of the heart during inhalation and exhalation or during physical activity. At the end of a deep inhalation, when the chest expands due to a decrease in pressure in it, the blood is somewhat retained in the dilated vessels of the small circle and therefore flows in smaller quantities into the left atrium, and from there into the left ventricle. The latter, due to less blood filling, ends systole earlier than the right one, and the closure of the aortic valve precedes the closure of the pulmonary valve. During exhalation, the opposite conditions are created. In the case of increased pressure in the chest, blood, as if squeezed out of the vessels of the pulmonary circle, enters in large quantities into the left part of the heart, and the systole of the left ventricle, and therefore the beginning of its diastole, occurs later than the right.
At the same time, a split second tone may be a sign of serious pathological changes in the heart and its valves. Thus, a bifurcation of the second sound at the base of the heart (second intercostal space on the left) is heard with mitral stenosis. This is due to the fact that the hypertrophied and blood-filled right ventricle ends systole later than the left. Therefore, the aortic component of the second sound occurs earlier than the pulmonary one. Bifurcation or splitting of the second sound in bicuspid valve insufficiency is associated with greater blood filling of the left ventricle than normal, which leads to prolongation of its systole, and the diastole of the left ventricle begins later than the right. Because of this, the aortic valve closes later than the pulmonary valve.
One should distinguish from the true splitting of the second tone its sound melody, which only superficially resembles splitting. An example is the additional tone that occurs during the opening of the bicuspid (mitral) valve with mitral stenosis. It has a high-pitched clicking tone and is perceived as a loud echo following the second tone. The additional tone, together with the clapping first and second, form a peculiar melody, reminiscent of the cry of a quail. Hence the name of this sound phenomenon, heard with mitral stenosis at the apex of the heart - “ quail rhythm”
" Its distribution area is extensive - from the apex of the heart up and into the axillary fossa.
Sometimes, when listening to the heart, against the background of rare and dull tones, a lonely, very loud tone appears, the so-called “gun tone” Strazhesko
. It is caused by the simultaneous contraction of the atria and ventricles, which is observed with complete atrioventricular block, i.e. when impulses from the atria do not reach the ventricles and they each contract in their own rhythm (the atria contract more often), but in some cycle their contractions coincide.
Next: heart murmurs.
In English:
All heart sounds (English):
Gallop rhythm and quail rhythm: signs of pathological tones, causes, diagnosis, treatment
© Sazykina Oksana Yurievna, cardiologist, especially for SosudInfo.ru (about the authors)
From time immemorial, a doctor, when examining a sick person, relies only on his hands and ears, because imaging diagnostic methods appeared relatively recently.
And to this day, one of the most important medical procedures is auscultation, or listening with a special tube to the sounds created by the work of the heart. Such sounds can be normal or pathological, for example, the gallop rhythm and the quail rhythm.
In order to find out why such rhythms occur and what diseases they may be caused by, you should understand the formation of normal heart sounds.
Pathological split rhythms
Such rhythms are considered to be sound phenomena that are formed due to pathology of the heart muscle itself or valve structures.
When listening to a heart with a similar pathology, a three-part rhythm is determined, in which the second sound seems bifurcated (split). But in fact, the split sound is nothing more than an additional tone.
What exactly causes the pathological tone depends on the type of rhythm. Split rhythms include the gallop rhythm and the quail rhythm.
The mechanism of gallop rhythm formation
The pathological three-membered heart rhythm, which occurs with severe damage to the heart muscle and is almost always accompanied by tachycardia, is called the gallop rhythm, since its sound qualities resemble the fast running of a horse.
It can be proto-diastolic (“after” diastole, immediately after the second sound) and presystolic (“before” systole, after a longer period of time after the second sound, immediately before the first sound).
But in any case, the gallop rhythm is characterized by the presence of pathological III and pathological IV tones, caused by either severe heart failure with loss of muscle tone in the left ventricle, or hypertrophy of the left ventricle, respectively.
https://www.youtube.com/watch?v=a6n7l_9DXF8\u0026list=PL6FBf4FJC4Fw4OzBpCRLhWjcaq5XyFcPj
A protodiastolic gallop rhythm is more common when the left ventricle is overloaded with volume, such as in dilated cardiomyopathy, when the left ventricular cavity is significantly enlarged and dilated.
The presystolic subtype of gallop rhythm is more common in hypertrophic cardiomyopathy, when pressure overload of the left ventricle occurs.
Both subtypes of the gallop rhythm are often referred to as the “heart's cry for help,” or the heart's cry for digitalis (a group of heart medications called cardiac glycosides, derived from the foxglove plant and used in the treatment of heart failure).
The melody of the heart during the gallop rhythm can be described literally as:
– ta – ta – ta – ta – ta – ta – ta – I tone – II tone – III+IV tone – I tone – II tone – III+IV tone – I tone
The mechanism of quail rhythm formation
In addition to the gallop rhythm, the quail rhythm also has three parts. This rhythm is due to the apparent bifurcation of the second tone. In fact, the second sound does not bifurcate, it is simply accompanied by a sound called a “mitral click.”
The occurrence of such an additional tone is due to the presence of adhesions and commissures between the leaflets of the mitral valve, therefore, when the valve opens, a characteristic clicking sound occurs. The quail rhythm is most clearly heard at the point of projection of the mitral valve (in the fifth intercostal space under the nipple).
The additional tone begins in diastole and can be heard immediately after the second tone. It is otherwise called TOMK, or the mitral valve opening tone.
quail rhythm on FKG
Along with the additional tone, when the mitral valve ring narrows, the first two tones also become more intense. Thus, the first sound is enhanced due to the fact that the left ventricle vibrates more strongly due to less blood flow into it than normal.
That is, the muscle creates a stronger sound. The second tone is enhanced by the sound of the pulmonary artery valves opening.
This is due to the fact that with mitral stenosis, the blood does not completely enter the ventricle; accordingly, in the left atrium the volume of blood is greater than normal, and in the pulmonary veins that bring blood to the left atrium, pressure increases - pulmonary hypertension is formed.
In conditions of pulmonary hypertension, the valves of the pulmonary trunk, on the contrary, carrying blood from the right ventricle into the arteries of the lungs, slam shut louder than usual - the second tone intensifies.
Letter designation of the heart melody with the rhythm of a quail:
– sleep – by – ra – sleep – by – ra – I tone – II tone – additional. tone – I tone – II tone – additional. tone
What diseases cause abnormal heart rhythms?
Based on the above, during auscultation of the heart, the doctor may suspect the presence of one or another heart pathology in the patient.
1. Gallop rhythm , as a rule, can be determined by:
- acute myocardial infarction,
- acute myocarditis (inflammation of the heart muscle),
- hypertrophy of the left ventricle (with arterial hypertension, stenosis of the aortic mouth of rheumatic or atherosclerotic origin),
- dilated cardiomyopathy (with coronary heart disease),
- acute left ventricular failure,
- chronic left ventricular failure due to post-infarction or post-myocardial origin.
2. The quail rhythm is caused by stenosis of the left atrioventricular orifice (mitral stenosis). This pathology is an acquired heart defect that develops as a result of acute rheumatic fever, scarlet fever, tonsillitis or chronic tonsillitis.
What further examination is necessary?
If during the examination the doctor was able to listen to the rhythm of a gallop or the rhythm of a quail, he should refer the patient for further examination. First of all, an ECG and chest x-ray are necessary. Any of the listed diseases can be detected by performing these methods (heart attack - on an ECG, hypertrophy or dilatation of the heart - on an x-ray, etc.).
To clarify the nature of pathological tones in the heart, phonocardiography (PCG) is used - a study in which the sounds of tones are amplified using a microphone and then converted into a graphic image using a writing device. FCG is interpreted by a specialist and helps to reliably determine what causes pathological sound phenomena. FCG is often performed in children with suspected heart disease.
However, a complete clinical diagnosis can be established only after performing imaging diagnostic methods - ultrasound (echocardioscopy) or CT (MRI, MSCT) of the heart. These methods make it possible to accurately determine the type of defect, the presence of cardiomyopathy or post-inflammatory scar, as well as the localization of pathological changes.
Do pathological rhythms need to be treated?
Therapy in the presence of pathological rhythms in a patient is necessary only after a thorough examination and establishment of an accurate diagnosis. The type of medical institution where treatment will be carried out depends on the underlying disease.
For example, hypertension, leading to left ventricular hypertrophy, can be dynamically observed in a clinic, and more severe pathologies (heart attack, myocarditis, severe heart failure) must be treated in a hospital setting.
Mitral stenosis, when diagnosed for the first time, also requires further examination and selection of therapy in a hospital, where the need for surgical correction of the defect will be determined.
https://www.youtube.com/watch?v=r38tHeDKMWY\u0026list=PL6FBf4FJC4Fw4OzBpCRLhWjcaq5XyFcPj
In conclusion, it should be noted that listening to pathological rhythms is the highest skill of a doctor, which comes with experience and requires constant practice. Therefore, a physician specializing in internal medicine or cardiology should pay special attention to chest auscultation when examining a patient.
© 2012-2020 sosudinfo.ru
Sources
Source: https://sosudinfo.ru/serdce/ritm-galopa-i-perepela/
Mitral valve prolapse - symptoms and treatment
Diagnosis criteria
Mitral valve prolapse is most often diagnosed using non-invasive examination methods - the doctor takes into account the patient’s complaints and heredity. But the final diagnosis is made using transthoracic echocardiography.
Instrumental diagnostic methods
During auscultation (listening to the heart) with a stethoscope, the doctor may hear a characteristic systolic click and/or late systolic murmur over the apex of the heart. With the patient standing, the systolic click and murmur appear at the beginning of systole (contraction). With the patient lying or squatting, these sound phenomena are reduced.
The electrocardiogram can detect nonspecific changes in the ST segment and T wave in leads III and aVF. In the presence of mitral valve prolapse, the ECG can diagnose the phenomenon of pre-excitation (“short PQ syndrome”), supraventricular (atrial) tachycardia, and ventricular extrasystole.
chest x-ray Cardiac enlargement may be diagnosed in some patients with a very small anteroposterior chest size.
Transthoracic echocardiography ( Echo-CG) . It is carried out using an ultrasound sensor placed by a doctor on certain points of the chest. It is the most important routine examination in the diagnosis of mitral valve prolapse. Distinctive and important echocardiographic signs of this pathology include deflection of the posterior or both leaflets of the mitral valve into the cavity of the left atrium in mid-systole, in late systole or throughout systole. Deflection (sagging) of the mitral valve in mid-systole is more common, which corresponds to the data obtained by auscultation and angiography.
There are other echocardiographic signs, they are nonspecific, but highly sensitive:
- dilatation (expansion) of the mitral ring;
- increased range of motion of the mitral valve, diastolic contact of the leaflets with the interventricular septum;
- an increase in the range of diastolic divergence of the leaflets and the speed of opening of the anterior valve leaflet;
- systolic displacement of the anterior and posterior leaflets of the mitral valve (more than 3 mm) into the left atrium below the closure of the mitral line;
- thickening of the mitral valve leaflets;
- signs of disruption of the internal structure of the valve tissue (myxomatous valve degeneration);
- reverse blood flow;
- signs of increased pressure in the pulmonary artery.
Transthoracic echocardiography is recommended every 6 to 12 months in all asymptomatic patients with moderate to severe mitral regurgitation. This is necessary to assess the ejection fraction (pumping function of the heart, normally it should be at least 55%) and end-systolic size.
Transesophageal echocardiography. This is an ultrasound test in which a probe is inserted into the esophagus. Indicated only in the absence of contraindications in the following cases:
- Echo-CG does not assess the severity and mechanism of mitral regurgitation and/or the state of left ventricular function;
- The patient is about to undergo valve surgery; during the examination, the question of the nature of the surgical intervention is decided.
A type of prolapse is the so-called valve . It is usually detected by rupture of the chordae or avulsion of the papillary muscle (more common in acute myocardial infarction). With echocardiography in B-mode, the freely moving papillary muscle and the “dangling” mitral valve leaflet are clearly visible. The valve makes irregular, voluntary movements during diastole (the period of relaxation of the heart muscle) and “falls” into the cavity of the left atrium during ventricular systole. In M-mode, characteristic echocardiographic signs of such a valve are the presence of:
- additional echo signals from the mitral valve leaflet in the cavity of the left atrium during the period of ventricular contraction;
- diastolic vibration of the anterior valve leaflet or paradoxical movement of the posterior mitral leaflet in systole and diastole.
Radionuclide equilibrium ventriculography is performed to assess ejection fraction and assess the severity of heart failure. The method is based on the intravenous administration of a radionuclide with its fixation on red blood cells and subsequent quantitative assessment of the contractility of the heart.
Differential diagnosis
The strategy and tactics of patient management depend on the origin of the prolapse - congenital or acquired, therefore differential diagnosis is carried out only between these types of mitral valve prolapse.
Gallop rhythm. Quail rhythm
The main tones during auscultation of the heart are the I and II sounds. In addition, under certain conditions, additional 3rd and 4th heart sounds and the mitral valve opening sound (MOV) may appear.
The first sound is recorded at the beginning of systole, it approximately coincides with the S wave of the ECG. The second sound is recorded at the beginning of diastole, it approximately coincides with the end of the T wave of the ECG. The third tone is a very quiet sound phenomenon - it is 200 times weaker than the second tone and is heard as a dull “echo” of the second tone. The third tone is low-frequency, appears in the first third of diastole, i.e. in protodiastole - 0.12 - 0.19″ after the second sound. The IV heart sound is recorded at the end of diastole (presystole) and coincides with the P wave of the ECG. TOMK is a high-frequency sound that appears with mitral valve stenosis. Heard almost immediately after the second tone.
III heart sound
The third tone was described in the 19th century by P. Pothen (1866) and has since been considered an important sign of ventricular damage. The National Directorate of Programs for Therapy and Cardiology (USA) has designated the third heart sound as the most important additional heart sound in terms of its diagnostic value .
III low-frequency tone - from 10 to 70 Hz (40-50 Hz), it occurs during passive filling of the ventricles with blood (in protodiastole). At this time, the ventricles are filled with blood by 80% (!) .
Figuratively, we can say that when the AV valves open, the blood falls (“flops”) into the ventricles and then the third heart sound is heard - from the vibration of the ventricular muscles. In this case, a hydraulic shock occurs against the wall of the ventricles of a portion of blood.
The third sound is called the sound of diastolic filling of the ventricles , as well as ventricular or protodiastolic .
However, in healthy people, tone III is very quiet. This is due to the fact that with good diastolic tone, the shock of a portion of blood from the atrium is absorbed by the normally relaxing ventricular myocardium (A.V. Strutynsky, 2004).
The question of whether the third tone is physiological or pathological is decided by the doctor, taking into account the specific circumstances under which this tone is heard.
IV heart sound
The IV tone is a low-frequency quiet sound that occurs at the end of diastole - before the I tone (in presystole).
It is called “ atrial tone ,” emphasizing the connection of the IV tone with atrial contraction (evidence of the role of atrial systole in the occurrence of the IV tone is the fact of its disappearance when atrial fibrillation occurs).
The IV sound is also called late diastolic or presystolic additional tone (as mentioned above, the III sound is called ventricular or protodiastolic).
The relatively loud IV tone in combination with the I and II sounds causes a three-beat rhythm called the atrial or presystolic gallop.
Gallop rhythm
The gallop rhythm of the heart is the threefold rhythm of the heart at a high heart rate. It got its name from its resemblance to the sound of a galloping horse. The famous French clinician Henri Huchard said: “There is no gallop without tachycardia.”
The reason for the appearance of the gallop rhythm is changes in the properties of the ventricular myocardium.
Pierre Potin (Potin Pierre Charles Edouard, 1825 -1903), a French therapist, explained the gallop rhythm by vibration of the walls of the left ventricle when it lost tone . As is known, in protodiastole the flow of blood from the atria into the ventricles begins.
Normally, it occurs silently (not perceived by the ear), since the ventricular muscle, which has tone, straightens gradually and absorbs the shock of a portion of blood coming from the atrium.
If the muscle has lost its tone and “hangs like a bag,” then the blood, falling to the bottom of the ventricle, causes an additional beat, heard as an additional sound - a pathological III heart sound.
The gallop rhythm can be of two types: protodiastolic and presystolic:
Protodiastolic gallop rhythm (the so-called ventricular gallop rhythm) - it is based on a pathological III tone , which has higher frequency components than normal; an additional tone is heard after II then at the apex of the heart. George Taylor (South Carolina, USA, 2004) gives the following brief description of the third tone and protodiastolic gallop: “a large flabby ventricle (volume overload).”
III tone 90/min (protodiastolic gallop)
Presystolic gallop rhythm (atrial gallop) - it is based on a pathological IV tone - this rhythm is better recorded with a long PQ ECG interval; The appearance of a pathological IV tone depends on the value of the end-diastolic pressure in the ventricle, the rigidity of the left ventricle, its poor “straightening”, and poor relaxability.
IV tone 90/min (presystolic gallop)
It is very important that it can be “palpated”, i.e. feel this diastolic tone with your hand. The rhythm of the gallop indicates heart failure - this is the “cry of the heart for help”, they used to say that this is the “cry of the heart for digitalis”.
The gallop rhythm is a cry from the heart for help!
Summation gallop
Summation (or mesodiastolic) gallop is a three-term ventricular rhythm, when, as a result of a sharp shortening of the slow filling phase against the background of tachycardia, pathological III and IV sounds merge into one additional fairly loud tone.
The main conditions for the occurrence of a summation gallop are:
- a decrease in the contractility of the ventricular myocardium in patients with heart failure and acute myocardial damage, leading, on the one hand, to a decrease in its diastolic tone and rate of relaxation (“flabby ventricle, the ventricle “hangs like a bag”) - this gives the third pathological heart sound;
- an increase, of course, in diastolic pressure in the ventricle - this gives the IV pathological heart sound;
A characteristic combination for such patients is the presence of hypertension and heart failure.
Summation gallop can also occur with AV block of the first degree, when an extended PQ interval leads to a displacement of the IV sound closer to the beginning of diastole, where it merges with the III sound.
The summation gallop tone has a higher frequency, is louder and longer lasting than the III and IV tones separately.
The dual nature of the summation gallop can be revealed by slowing down the rhythm, for example, during massage of the carotid sinus. In this case, a four-part gallop rhythm with the third and fourth heart sounds heard separately.
III and IV sounds 60/min
Total
So, the protodiastolic (ventricular) gallop is associated with an audible III sound. An additional tone is heard after the second tone. It is perceived both by the ear and by palpation. Gallop is usually observed with tachycardia. Many clinicians believe that the ventricular gallop rhythm is the most reliable sign of heart failure, determined physically.
IV tone and presystolic gallop are “a hard, unyielding ventricle (pressure overload).”
The protodiastolic gallop rhythm is more unfavorable prognostically.
It should be noted once again that gallop refers to any three-term diastolic heart rhythm, the speed of which is so high that it imitates the running of a horse.
The term "gallop rhythm" implies a high heart rate (often combined with dulling of the 1st and 2nd sounds) and a typical melody. The rhythm of the gallop is a more threatening sign than the simple presence of the third tone .
As mentioned above, the third heart sound may be “close to physiological”, and also be a reflection of the relative volume overload of the left ventricle and not form a gallop rhythm. On the contrary, the gallop rhythm with the third tone is almost always pathological.
As the observations of V.P. Obraztsov and M.M. Gubergrits, now confirmed by many Soviet clinicians and foreign therapists, have shown, that even in healthy people the heart melody heard by direct auscultation is three-membered (the so-called
normal third tone) and that with a relatively minor pathology, as well as under physiological circumstances, splitting and bifurcation of the first tone (? V.O.) can be observed (over 10% according to V.P.
Obraztsov), it is clear that between the rhythm of the gallop and the normal melody of the heart there are gradual transitions, and not a sharp inseparable line .”
The importance of gallop rhythm was interestingly defined by George Taylor (2004):
“Traditionally, a lot of attention is paid to heart murmurs, but they, while helping to make a correct diagnosis, cannot tell us as much about the severity of the disease. It’s the gallops and the apical impulse that do this: they tell us about the size of the ventricle, its function and diastolic compliance.”