Mitral valve prolapse - normal or pathological?
P
The term mitral valve prolapse (MVP) refers to
the sagging of one or both mitral valve leaflets into the cavity of the left atrium during systole
. This phenomenon was described relatively recently - only in the second half of the 60s, when the echocardiography method appeared. Then it was noticed that in individuals with a mid-systolic click and systolic murmur at the first point of auscultation during echocardiography, the mitral valve leaflet(s) sags into the cavity of the left atrium during systole.
Currently, a distinction is made between primary (idiopathic) and secondary MVP. Causes of secondary MVP
are rheumatism, chest trauma, acute myocardial infarction and some other diseases. In all these cases, the mitral valve chords are separated, as a result of which the leaflet begins to sag into the atrium cavity. In patients with rheumatism, due to inflammatory changes affecting not only the valves, but also the chords attached to them, separation of small chords of the 2nd and 3rd order is most often noted. According to modern views, in order to convincingly confirm the rheumatic etiology of MVP, it is necessary to show that the patient did not have this phenomenon before the onset of rheumatism and arose during the course of the disease. However, in clinical practice this is very difficult to do. At the same time, in patients with mitral valve insufficiency referred for cardiac surgery, even without a clear indication of a history of rheumatism, in approximately half of the cases, morphological examination of the mitral valve leaflets reveals inflammatory changes in both the leaflets themselves and the chordae.
Chest trauma
is the cause of acute chordal separation and the development of severe mitral insufficiency with the clinical picture of acute left ventricular failure.
This is often the cause of death in such patients. Acute posterior myocardial infarction
affecting the posterior papillary muscle also leads to chordal avulsion and the development of posterior mitral valve prolapse.
The population frequency of MVP, according to different authors (from 1.8 to 38%), varies significantly depending on the diagnostic criteria used, but most authors believe that it is 10–15%. At the same time, secondary MVP accounts for no more than 5% of all cases. The prevalence of MVP varies significantly with age - after 40 years, the number of people with this phenomenon decreases sharply and in the age population over 50 years old it is only 1–3%. Therefore, MVP is a pathology of people of young working age
.
In people with MVP, according to the results of many researchers, an increased incidence of serious complications has been established:
sudden death, life-threatening arrhythmias, bacterial endocarditis, stroke, severe mitral valve regurgitation. Their frequency is low - up to 5%, however, given that these patients are of working, military and childbearing age, the problem of identifying a subgroup of patients with an increased risk of complications among the huge number of people with MVP becomes extremely urgent.
Idiopathic (primary) MVP
Currently, it is the most common pathology of the valvular apparatus of the heart. According to the vast majority of authors, the basis for the pathogenesis of idiopathic MVP is genetically determined disorders of various components of connective tissue, which leads to “weakness” of the connective tissue of the mitral valve leaflets and, therefore, their prolapse into the atrium cavity under blood pressure during systole. Since connective tissue dysplasia is considered the central pathogenetic link in the development of MVP, these patients should have signs of connective tissue damage from other systems, not just the heart. Indeed, many authors have described a complex of changes in the connective tissue of different organ systems in individuals with MVP. According to our data, these patients are significantly more likely to have an asthenic type of constitution, increased skin extensibility (more than 3 cm above the outer ends of the clavicles), funnel chest deformity, scoliosis, flat feet (longitudinal and transverse), myopia, increased joint hypermobility (3 or more joints), varicose veins (including varicoceles in men), positive signs of the thumb (the ability to extend the distal phalanx of the thumb beyond the ulnar edge of the palm) and wrist (the first and fifth fingers cross when grasping the wrist of the opposite hand ). Since these signs are revealed during a general examination, they are called phenotypic signs of connective tissue dysplasia. At the same time, in persons with MVP, at least 3 of the listed signs are simultaneously detected (usually 5–6 or even more). Therefore, to identify MVP, we recommend sending individuals with the simultaneous presence of 3 or more phenotypic signs of connective tissue dysplasia for echocardiography.
We conducted a morphological study of skin biopsies in individuals with MVP using light-optical examination (histological and histochemical methods). A complex of morphological signs of skin pathology has been identified - degeneration of the epidermis, thinning and smoothness of the papillary layer, destruction and disorganization of collagen and elastic fibers, changes in the biosynthetic activity of fibroblasts and pathology of the microvasculature and some others. At the same time, no similar changes were found in skin biopsies of individuals in the control group (without MVP). The identified signs indicate the presence of connective tissue dysplasia of the skin in persons with MVP, and, consequently, the generalization of the process of “weakness” of the connective tissue.
Clinical picture
The clinical picture of MVP is very diverse and can be divided into 4 major syndromes
– vegetative dystonia, vascular disorders, hemorrhagic and psychopathological.
Autonomic dystonia syndrome
(VDS) includes pain in the left half of the chest (stabbing, aching, not associated with physical activity, lasting either a few seconds for stabbing pains or hours for aching pains), hyperventilation syndrome (the central symptom is a feeling of lack of air, the desire to take a deep, full breath), disturbances in the autonomic regulation of heart activity (complaints of palpitations, a feeling of a rare heartbeat, a feeling of uneven beating, “fading” of the heart), disturbances in thermoregulation (a feeling of “chilling”, long-lasting low-grade fever after infections), disorders with side of the gastrointestinal tract (irritable bowel syndrome, functional gastric dyspepsia, etc.), psychogenic dysuria (frequent or, on the contrary, rare urination in response to psycho-emotional stress), increased sweating. Naturally, in such a situation, all possible organic causes that could cause similar symptoms should be excluded.
Vascular dysfunction syndrome
includes syncope - vasovagal (fainting in stuffy rooms, during prolonged standing, etc.), orthostatic, as well as pre-syncope in the same conditions, migraines, crawling sensation in the legs, distal extremities cold to the touch, morning and night headaches (based on venous congestion), dizziness, idiopathic pastosity or swelling. Currently, the hypothesis about the arrhythmogenic nature of syncope in MVP has not been confirmed, and they are considered vasovagal (i.e., a violation of the autonomic regulation of vascular tone).
Hemorrhagic syndrome
combines complaints of easy bruising, frequent nosebleeds and bleeding from the gums, heavy and/or prolonged menstruation in women. The pathogenesis of these changes is complex and includes a violation of collagen-induced platelet aggregation (due to collagen pathology in these patients) and/or thrombocytopathies, as well as vascular pathology such as vasculitis. In persons with MVP and hemorrhagic syndrome, thrombocytosis and increased ADP-platelet aggregation are often detected, which are regarded as reactive changes in the hemostatic system such as hypercoagulation, as a compensatory reaction of this system to chronic hemorrhagic syndrome.
Syndrome of psychopathological disorders
includes neurasthenia, anxiety-phobic disorders, mood disorders (most often in the form of mood instability). An interesting fact is that the severity of clinical symptoms directly correlates with the number of phenotypic signs of “weakness” of connective tissue from other organ systems and with the severity of morphological changes in the skin (see above).
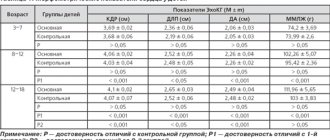
ECG changes in MVP are most often detected by Holter monitoring. Significantly more often in these patients, negative T waves in leads V1,2, episodes of paroxysmal supraventricular tachycardia, sinus node dysfunction, prolongation of the QT interval, supraventricular and ventricular extrasystoles in the amount of more than 240 per day, horizontal depression of the ST segment (lasting more than 30 minutes per day) were noted ). Since ST segment depression occurs in individuals with pain in the left half of the chest other than angina, taking into account the young age of these patients, the absence of dyslipidemia and other risk factors for coronary heart disease, these changes are not interpreted as ischemic. They are based on uneven blood supply to the myocardium and/or sympathicotonia. Extrasystoles, especially ventricular ones, were detected to a greater extent in patients lying down. At the same time, during a test with physical activity, the extrasystoles disappeared, which indicates their functional nature and the role of hyperparasympathicotonia in their genesis. In a special study, we noted a predominance of parasympathetic tone and/or a decrease in sympathetic influences in individuals with MVP and extrasystole.
When conducting a test with maximum physical activity, we established high or very high physical performance of patients with MVP, which did not differ from that of the control group. However, these individuals showed disturbances in the hemodynamic support of physical activity in the form of lower threshold values of heart rate (HR), systolic blood pressure (BP), double product and their lower increase per threshold load, which directly correlated with the severity of SVD and phenotypic severity connective tissue dysplasia.
Typically in clinical practice, MVP is associated with the presence of arterial hypotension. According to our data, the frequency of arterial hypotension did not differ significantly in individuals with or without MVP, however, the frequency of arterial hypertension (WHO grade 1 - OHCA) was significantly higher than in the control group. We identified arterial hypertension in approximately 1/3 of the examined young (18–40) persons with MVP, while in the control group (without MVP) it was only in 5%.
The functioning of the autonomic nervous system in MVP is of great clinical importance, since until recently it was believed that sympathetic influences predominated in these patients, so b-blockers were the drugs of choice for treatment. However, at present, the point of view on this aspect has changed significantly: among these people there are people with both a predominance of sympathetic tone and a predominance of the tone of the parasympathetic part of the autonomic nervous system. Moreover, the latter even predominate. According to our data, an increase in the tone of one or another link is more correlated with clinical symptoms. Thus, sympathicotonia was noted in the presence of migraine, arterial hypertension, pain in the left half of the chest, paroxysmal supraventricular tachycardia, vagotonia - in syncope, extrasystole.
The presence of SVD and the type of autonomic regulation in individuals with MVP is directly related to the fourth syndrome of the clinical picture - psychopathological disorders. In the presence of these disorders, the frequency of detection and severity of VDS increases, as well as the frequency of detection of hypersympathicotonia. According to many authors, it is the psychopathological disorders in these individuals that are primary, and the symptoms of SVD are secondary, arising in response to these psychopathological features. The results of treatment of persons with MVP also indirectly support this theory. Thus, the use of b-blockers, although it makes it possible to eliminate objective signs of hypersympathicotonia (for example, heart rate significantly decreases), but all other complaints persist. On the other hand, treatment of persons with MVP with anti-anxiety drugs led not only to the correction of psychopathological disorders, a significant improvement in the well-being of patients, but also to the disappearance of hypersympathicotonia (heart rate and blood pressure levels decreased, supraventricular extrasystoles and paroxysms of supraventricular tachycardia decreased or disappeared).
Diagnostics
The main method for diagnosing MVP is still echocardiography
. Currently, it is believed that it is necessary to use only B-mode, otherwise a large number of false positive results can be obtained. In our country, it is customary to divide MVP into 3 degrees depending on the depth of prolapse (1st – up to 5 mm below the valve ring, 2nd – 6–10 mm and 3rd – more than 10 mm), although many domestic authors have established that that MVP up to 1 cm in depth is prognostically favorable. At the same time, persons with 1st and 2nd degrees of prolapse practically do not differ from each other in clinical symptoms and frequency of complications. In other countries, it is customary to divide MVP into organic (in the presence of myxomatous degeneration) and functional (in the absence of EchoCG criteria for myxomatous degeneration). In our opinion, this division is more optimal, since the likelihood of developing complications depends on the presence of myxomatous degeneration (regardless of the depth of MVP).
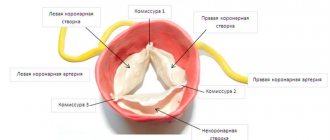
Under myxomatous degeneration
understand the complex of morphological changes in the cusps of the mitral valve, corresponding to the “weakness” of the connective tissue (see above for the description of morphological changes in the skin) and described by morphologists as a result of studying materials obtained during cardiac surgery (in persons with MVP and severe, hemodynamically significant, mitral regurgitation) . In the early 90s, Japanese authors created echocardiographic criteria for myxomatous degeneration - their sensitivity and specificity are about 75%. These include leaflet thickening greater than 4 mm and decreased echogenicity. Identifying individuals with myxomatous leaflet degeneration is very important, since all complications of MVP (sudden death, severe mitral valve regurgitation requiring surgical treatment, bacterial endocarditis and strokes) in 95–100% of cases are noted only in the presence of myxomatous leaflet degeneration. According to some authors, such patients need antibiotic prophylaxis for bacterial endocarditis (for example, during tooth extraction). MVP with myxomatous degeneration is also considered one of the causes of stroke in young people without generally accepted risk factors for stroke (primarily arterial hypertension). We studied the frequency of ischemic strokes and transient ischemic attacks in patients under the age of 40 years using archival data from 4 clinical hospitals in Moscow over a 5-year period. The proportion of these conditions in persons under 40 years of age averaged 1.4%. Among the causes of strokes in young people, hypertension should be noted - 20% of cases, however, 2/3 of young people did not have any generally accepted risk factors for the development of ischemic brain damage. Some of these patients (who consented to participate in the study) underwent echocardiography, and in 93% of cases, MVP with myxomatous degeneration of prolapsed leaflets was detected. Myxomatously altered mitral valve leaflets can be the basis for the formation of micro- and macrothrombi, since the loss of the endothelial layer with the appearance of small ulcerations due to increased mechanical stress is accompanied by the deposition of fibrin and platelets on them. Consequently, strokes in these patients are of thromboembolic origin, and therefore, for persons with MVP and myxomatous degeneration, a number of authors recommend daily intake of small doses of acetylsalicylic acid. Another reason for the development of acute cerebrovascular accidents during MVP is bacterial endocarditis and bacterial emboli.
Treatment
The treatment of these patients is practically undeveloped. In recent years, an increasing number of studies have been devoted to studying the effectiveness of oral magnesium supplements.
. This is due to the fact that magnesium ions are necessary for laying collagen fibers into a quaternary structure, therefore magnesium deficiency in tissues causes the random arrangement of collagen fibers - the main morphological sign of connective tissue dysplasia. It is also known that the biosynthesis of all matrix components in connective tissue, as well as the maintenance of their structural stability, is a function of fibroblasts. From this point of view, it seems important that we and other authors detected a decrease in the RNA content in the cytoplasm of dermal fibroblasts, which indicates a decrease in the biosynthetic activity of the latter. Considering the information about the role of magnesium deficiency in dysfunction of fibroblasts, it can be assumed that the described changes in the biosynthetic function of fibroblasts and disruption of the structure of the extracellular matrix are associated with magnesium deficiency in patients with MVP.
A number of researchers have reported tissue magnesium deficiency in individuals with MVP. We have established a significant decrease in the level of magnesium in the hair in 3/4 of patients with MVP (on average 60 or less mcg/g, with the norm being 70–180 mcg/g).
We treated 43 patients with MVP aged 18 to 36 years with Magnerot
, containing 500 mg of magnesium orotate (32.5 mg of elemental magnesium) at a dose of 3000 mg/day (196.8 mg of elemental magnesium), for 3 doses.
After using Magnerot in patients with MVP, a significant decrease in the frequency of all symptoms of SVD was revealed
. Thus, the frequency of disorders of autonomic regulation of heart rhythm decreased from 74.4 to 13.9%, thermoregulation disorders - from 55.8 to 18.6%, pain in the left half of the chest - from 95.3 to 13.9%, disorders gastrointestinal tract – from 69.8 to 27.9%. Before treatment, mild VDS was diagnosed in 11.6%, moderate in 37.2%, severe in 51.2% of cases, i.e. Patients with severe and moderate-severe severity of autonomic dystonia syndrome predominated. After treatment, a significant decrease in the severity of SVD was noted: there were people (7%) with a complete absence of these disorders, the number of patients with a mild degree of SVD increased 5 times, while a severe degree of SVD was not found in any patient.
, the frequency and severity of vascular disorders also significantly decreased in patients with MVP
morning headache from 72.1 to 23.3%, syncope from 27.9 to 4.6%, presyncope from 62.8 to 13.9%, migraine from 27.9 to 7%, vascular disorders in the extremities from 88.4 to 44.2%, dizziness from 74.4 to 44.2%. If before treatment mild, moderate and severe degrees were diagnosed in 30.2, 55.9 and 13.9% of people, respectively, then after treatment in 16.3% of cases there were no vascular disorders, the number of patients with mild increased by 2.5 times. degree of vascular disorders, but a severe degree was not detected in any of the subjects examined after treatment with Magnerot.
has also been established :
heavy and/or prolonged menstruation in women from 20.9 to 2.3%, nosebleeds - from 30.2 to 13.9%, bleeding gums disappeared. The number of people without hemorrhagic disorders increased from 7 to 51.2%, with an average degree of hemorrhagic syndrome - decreased from 27.9 to 2.3%, and a severe degree was not identified.
Finally, after treatment in patients with MVP, the frequency of neurasthenia significantly decreased
(from 65.1 to 16.3%) and mood disorders (from 46.5 to 13.9%), although the frequency of anxiety-phobic disorders did not change.
The severity of the clinical picture as a whole after treatment also significantly decreased. Therefore, it is not surprising that a highly significant increase in the quality of life of these patients
. This concept refers to the patient’s subjective opinion about the level of his well-being in physical, psychological and social terms. Before treatment, on a self-assessment scale of general well-being, persons with MVP rated it worse than the control group (persons without MVP) - by about 30%. After treatment, patients with MVP noted a significant improvement in quality of life on this scale – by an average of 40%. At the same time, the assessment of the quality of life on the scales “work”, “social life” and “personal life” before treatment in people with MVP also differed from the control: in the presence of MVP, patients assessed their impairments on these three scales as initial or moderate - approximately to the same extent, while healthy people noted the absence of violations. After treatment, patients with MVP showed a highly significant improvement in quality of life – by 40–50% compared to the baseline.
According to Holter ECG monitoring after Magnerot therapy, compared with the baseline level, a significant decrease in the average heart rate (by 7.2%), the number of tachycardia episodes (by 44.4%), the duration of the QT interval and the number of ventricular extrasystoles (by 40%) was established. The positive effect of Magnerot in the treatment of ventricular extrasystole seems especially important.
in this category of patients.
According to 24-hour blood pressure monitoring, a significant decrease in average systolic and diastolic blood pressure and hypertensive load to normal values was revealed. These results confirm the previously established fact that there is an inverse relationship between the level of magnesium in tissues and the level of blood pressure, as well as the fact that magnesium deficiency is one of the pathogenetic links in the development of arterial hypertension.
After treatment, a decrease in the depth of mitral valve prolapse and a significant decrease in the number of patients with hypersympathicotonia were revealed, while the number of people with equal tone of both parts of the autonomic nervous system increased. Similar information is contained in the works of other authors devoted to the treatment of persons with MVP with oral magnesium preparations.
Finally, according to a morphological study of skin biopsies, after treatment with Magnerot, the severity of morphological changes decreased by 2 times.
Thus, after a 6-month course of therapy with Magnerot in patients with idiopathic MVP, a significant improvement in objective and subjective symptoms was found with a complete or almost complete reduction in the manifestations of the disease in more than half of the patients.
During treatment, there was a decrease in the severity of vegetative dystonia syndrome, vascular, hemorrhagic and psychopathological disorders, heart rhythm disturbances, blood pressure levels, as well as an improvement in the quality of life of patients. In addition, during treatment, the severity of morphological markers of connective tissue dysplasia according to skin biopsy data significantly decreased. Literature:
1. Martynov A.I., Stepura O.B., Ostroumova O.D. et al. Mitral valve prolapse. Part I. Phenotypic features and clinical manifestations. // Cardiology. – 1998, No. 1 – P.72–80.
2. Martynov A.I., Stepura O.B., Ostroumova O.D. et al. Mitral valve prolapse. Part II. Rhythm disturbances and psychological status. // Cardiology. – 1998, No. 2 – P.74–81.
3. Stepura O.B., Ostroumova O.D. et al. The role of magnesium in the pathogenesis and development of clinical symptoms in individuals with idiopathic mitral valve prolapse. // Russian Journal of Cardiology – 1998, No. 3 – P.45–47.
4. Stepura O.B., Melnik O.O., Shekhter A.B. et al. Results of the use of magnesium salt of orotic acid “Magnerot” in the treatment of patients with idiopathic mitral valve prolapse. // Russian medical news – 1999 – No. 2 – P.12–16.
Symptoms
The most typical complaint is shortness of breath, which occurs with moderate and severe chronic mitral regurgitation and the clinic of acute left ventricular failure with acute mitral regurgitation. The presence of atrial fibrillation before surgery is an independent predictor of reduced long-term survival after mitral valve surgery for chronic mitral regurgitation.
Differential diagnosis
A differential diagnosis is carried out with acquired heart defects , based primarily on auscultatory data (especially in the presence of systolic murmur, which indicates mitral regurgitation).
Differential diagnosis of idiopathic MVP and myocarditis . Auscultation: with myocarditis, the noise that appears gradually progresses in intensity and area over several days, and then regresses in the same sequence. At the same time, there is a change in the boundaries of the heart to the left, followed by a return to the previous level. With myocarditis, no systolic “click” is heard. The diagnosis is confirmed by a decrease in the ejection fraction and a slight expansion of the left ventricular chamber during an echocardiographic study, as well as the dynamics of biochemical changes in the blood.
The above diseases, as well as cardiomyopathy, coronary heart disease, arterial hypertension , are accompanied by secondary prolapse of the mitral valve leaflets. This is mainly due to weakening or rupture of the chordal filaments or changes in the function of the papillary muscles. The main point in diagnosis, especially if it is impossible to perform echocardiography, is the presence of a constant rough noise, the intensity of which corresponds to the degree of mitral regurgitation and does not depend on stress tests, which are informative for primary MVP.
Also, a differential diagnosis is made with aneurysm of the interatrial septum , which, as a rule, is located in the area of the oval window and is associated with failure of connective tissue elements. It is a congenital developmental anomaly or occurs with hereditary connective tissue dysplasia, after spontaneous closure of an atrial septal defect. Aneurysmal protrusion is usually small, is not accompanied by hemodynamic disturbances and does not require surgical intervention. Suspicion of an aneurysm may arise if there are clicks in the heart, similar to those with MVP. A combination of aneurysm and prolapse is also possible. In order to clarify the nature of sound changes in the heart, echocardiography is performed. Confirmation of an aneurysm is the presence of protrusion of the interatrial septum towards the right atrium in the area of the oval window. Children with this defect are predisposed to the development of supraventricular tachyarrhythmias and sick sinus syndrome.
general information
Short description
Clinic automation: fast and inexpensive!
300 clinics from 4 countries connected
Clinic automation: fast and inexpensive!
I'm interested! Contact me
Clinical picture
Symptoms, course
In women, clinical symptoms are more common. Among them are nausea and “lump in the throat”, increased sweating, vegetative crises, asthenovegetative syndrome, periods of low-grade fever, syncopal states. Vegetative crises can appear spontaneously or situationally, are repeated at least three times within three weeks, and are not associated with significant physical stress or a life-threatening situation. Basically, crises are not accompanied by a bright emotional and vegetative arrangement.
Characteristic auscultatory signs of MVP
— isolated clicks (clicks); - combination of clicks with late systolic murmur; — isolated late systolic murmurs (LSS); - holosystolic murmurs.
It is necessary to distinguish between MVP clicks and ejection clicks, which occur in early systole and can be aortic or pulmonary. Aortic ejection clicks are heard, as with MVP, at the apex and do not change their intensity depending on the phase of breathing. Pulmonary ejection clicks are heard in the area of the projection of the pulmonary valve. Their intensity changes with breathing; they are better heard during exhalation.
Most often, MVP is manifested by a combination of systolic clicks with late systolic murmur , which is caused by turbulent blood flow resulting from bulging of the valves and vibration of tense tendon threads. Often, the combination of systolic clicks and late murmur is more clearly detected in an upright position after exercise.
Late systolic murmur is best heard in the left lateral decubitus position. It intensifies during the Valsalva maneuver and changes its character with deep breathing: as you exhale, the noise intensifies and sometimes takes on a musical tone.
In some cases, when systolic clicks are combined with a late murmur in an upright position, a holosystolic murmur .
In approximately 15% of cases, an isolated late systolic murmur . It is heard at the apex and carried into the axillary region. The noise continues until the second tone, has a rough, “scraping” character, and is better determined when lying on the left side. Isolated late systolic murmur is not a pathognomonic sign of MVP. It can occur with obstructive lesions of the left ventricle.
Late systolic murmurs should be distinguished from mid-systolic ejection murmurs, which also occur in isolation from the first sound after the opening of the semilunar valves and have a maximum sound in mid-systole.
Midsystolic ejection murmurs are observed with:
Diagnostics
Echocardiographic criteria for myxomatous mitral valve:
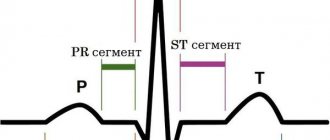
The main electrocardiographic (ECG) abnormalities in MVP: changes in the final part of the ventricular complex, disturbances in heart rhythm and conduction.
On a standard ECG, changes in the repolarization process are recorded in various leads. Typical options: 1. Isolated inversion of T waves in the limb leads; II, III, avF without ST segment displacement (inversion is more often associated with the location of the heart (vertical “drip” heart, located midway in the chest like a “suspended” heart). 2. Inversion of T waves in the limb leads and left chest leads (mainly in V5-V6) in combination with a slight ST shift below the isoline. Such inversion indicates the presence of hidden myocardial instability, the frequency increases by 2 times when recording a standard ECG in the orthostatic position. 3. Inversion of T waves in combination with ST segment elevation, which is caused by the syndrome of early ventricular repolarization (an electrocardiographic phenomenon consisting of pseudocoronary ST elevation above the isoline). The syndrome is based on congenital individual characteristics of electrophysiological processes in the myocardium, leading to early repolarization of its subepicardial layers. Occurs in the population with a frequency of 1.5% to 4.9%; in boys 3 times more often than in girls.
Radiography. In the absence of mitral regurgitation, expansion of the shadow of the heart and its individual chambers is not observed. Small heart sizes in 60% are combined with bulging of the pulmonary artery arch. Detectable bulging of the pulmonary artery arch confirms the inferiority of connective tissue in the structure of the vascular wall of the pulmonary artery, and borderline pulmonary hypertension and “physiological” pulmonary regurgitation are often determined.