Mitral valve prolapse
Mitral valve prolapse (MVP) is the most common heart problem.
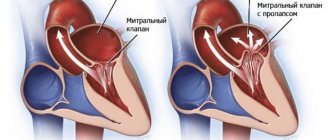
According to statistics, every fifth person has this defect. Most of them (30–40%) do not even suspect the presence of pathology, but in some cases it causes complications. Literally from Latin “prolapse” is translated as “loss”. Essentially, this is the sagging of one or both valve leaflets into the atrium cavity. It can occur at any age, but mitral valve prolapse is most often diagnosed in children.
Causes and degrees of mitral valve prolapse
Pathology can be primary and secondary. In the first case, the cause is connective tissue dysplasia. It causes a change in the structure and length of the chords by which the valve flaps are attached to the muscles, or contributes to the appearance of additional chords.
Secondary prolapse accompanies or complicates other pathologies. Possible reasons:
- congenital heart defects;
- endocrine disorders;
- rheumatic diseases;
- connective tissue diseases;
- genetic syndromes.
Risk factors are valvular-ventricular disproportion, infective endocarditis, insufficient blood supply to the papillary muscles, hypertrophic cardiomyopathy, inflammatory damage to the valvular structures of the heart, myocarditis, hypertrophy of the ventricular wall, pericarditis, coronary heart disease, chest trauma, etc.
The pathology is divided into 3 degrees depending on how much the valve leaflets protrude:
- 3–5 mm – I degree;
- 6–9 mm – II degree;
- ≥ 10 mm – III degree.
The course of the disease is usually benign. In most patients, the disorder does not progress throughout their lives. There are known cases of a decrease in the severity of pathology with age. Complications are rare, but they are possible.
Etiology of the disease
The main cause of the disease is dysgenesis of connective tissue, which is part of many organs and, in particular, the valve apparatus.
Underdevelopment of connective tissue can be caused for various reasons. These could be infections, intoxications and occupational hazards that affected the body of a pregnant woman and the fetus. There is no clear answer to what causes the disease.
The acquired form of the pathological disease occurs after an inflammatory disease, in particular infective endocarditis, rheumatism.
Signs of mitral valve prolapse
Clinical manifestations depend on the degree of connective tissue dysplasia. The main symptom is heart rhythm disturbances - acceleration, tremors, freezing, interruptions. During physical activity, stress, and drinking coffee, extrasystole, a feeling of lack of air, shortness of breath, and tachycardia often occur. Some patients experience shortness of breath even with little activity.
Other possible signs:
- chest pain;
- dyspnea;
- hyperventilation syndrome;
- vegetative crisis;
- increased sweating;
- anxiety;
- increased fatigue;
- headache;
- dizziness;
- feeling of a lump in the throat;
- decreased performance;
- irritability;
- mood swings;
- depression;
- presyncope and fainting;
- slight increase in body temperature.
Acquired prolapse occurs:
- rheumatic origin,
- due to calcification of the base in the posterior leaflet of the mitral valve,
- various dysfunctions and properties of the papillary muscle,
- chronic valvulitis, especially with CTD,
- due to infective endocarditis,
- when the integrity of the valve chords is violated,
- against the background of subaortic or aortic stenosis.
Symptoms The clinical picture of mitral valve prolapse is very different and is not an indicator for making a diagnosis, but can only give rise to speculation.
Patients may complain of:
- Pain in the heart area, often dull, but sometimes sharp and always passing quickly.
- Palpitations. Usually not associated with physical activity. Sometimes there are very pronounced ones, up to 200 beats per minute.
- Sometimes paroxysmal arrhythmia may develop, which patients feel as “failures in the heart.”
- Nervous system disorders are very often observed: severe migraine-like pain, anxiety, irritability, fainting, autonomic crises, mood swings, depression, panic attacks, and so on.
- The most common complaints about physical weakness: fatigue, shortness of breath, joint hypermobility, poorly developed muscles, poor posture, winged shoulder blades, scoliosis, myopia, flat feet, and so on.
Diagnostics The most important thing is to differentiate mitral valve prolapse from insufficiency of this valve, as well as from dysfunction of the myocardial valvular apparatus and from various minor anomalies of heart development. In this regard, listening to noise alone is not enough. The ECG is not always indicative, and sometimes there are no changes at all. X-ray of the heart will also give practically nothing, since the myocardium does not enlarge or sometimes has a slight bulging of the pulmonary arch (pulmonary artery arch) due to inferior connective tissue, but is not a definitive indicator of the presence of mitral valve prolapse. The most informative and revealing is EchoCG, according to which the final diagnosis is made.
Treatment Usually, mitral valve prolapse does not require any treatment. This is especially true for the “silent” form of prolapse. In some cases, symptomatic assistance is prescribed to improve the patient’s psycho-emotional and vegetative status. In case of auscultatory mitral valve prolapse in the absence of any noticeable disturbances and a satisfactory response to physical activity, adults are recommended to switch to light work, and children are advised not to participate in sports games associated with sudden movements. In general, moderate physical labor and exemption from physical education at school are not required. In the presence of mitral regurgitation of any degree and severe disturbances, as well as in the presence of clear arrhythmia, strict limitation in physical activity and the appointment of exercise therapy with an individual approach are necessary. If there are episodes of loss of consciousness or a family history of death from coronary insufficiency, non-selective magnesium preparations or cardioselective beta-blockers are prescribed. In case of significant mitral valve prolapse with severe persistent insufficiency, surgical valve correction, prosthetics or implantation may be prescribed.
Prognosis In general, the prognosis is favorable. Many patients live happily into old age and die for completely different reasons. And sometimes, with age, mitral valve prolapse decreases significantly and sometimes disappears altogether. The course of prolapse is usually benign, long-term and favorable. Mitral valve dysfunction progresses very slowly and a stable condition usually lasts throughout life.
consultation with a cardiologist
Diagnostics
The main diagnostic method is conventional auscultation of the heart (listening). When prolapse occurs, the doctor hears specific noises and clicks.
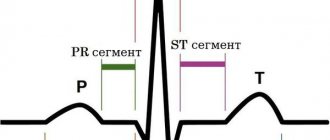
An ECG is not advisable because it does not show any abnormalities. The key test is echocardiography. If necessary, angiocardiography, left-sided ventriculography, and radionuclide testing are additionally performed.
Differential diagnosis is carried out with aneurysm of the interatrial septum, mitral valve insufficiency, acquired heart defects.
How to treat mitral valve prolapse?
Many patients do not require specific therapy. For mitral valve prolapse, medications are required for patients who experience heart palpitations and heart pain.
For moderate cases of the disease, sedative herbal remedies based on St. John's wort, valerian, hawthorn, valerian, and motherwort are prescribed.
In recent years, magnesium preparations have been increasingly used. Studies have established a beneficial effect on patients with MVP of the drug Magnerot, used for 6 months at a dose of 1000 mg three times a day.
For frequent extrasystoles and prolongation of the QT interval, the use of beta-blockers (Anaprilin or Sotalol) is indicated.
Severe mitral regurgitation requires surgical treatment.
Magazine "Child's Health" 2(5) 2007
Mitral valve prolapse (MVP), which is based on structural and functional disorders of the mitral valve of the heart, leading to bending of the valve leaflets into the cavity of the left atrium at the time of left ventricular systole, occupies a leading place in the structure of childhood diseases.
In recent years, the incidence of MVP has increased, therefore, despite the fact that the most characteristic auscultatory manifestation of the MVP phenomenon is the presence of systolic clicks (clicks) in combination with systolic murmur, with the widespread introduction of ultrasound research methods into practice, it became clear that even the absence of any - complaints, clinical symptoms and auscultatory changes do not exclude the possibility of its existence [1, 2].
At the present stage, the etiopathogenetic heterogeneity of the MVP phenomenon has been convincingly proven, manifested by clinical polymorphism and represented by such most recognized factors as, firstly, congenital microanomalies of the architecture of the valves, chords and atrioventricular ring, which over time, due to repeated microtraumas against the background of hemodynamic influences, become more pronounced, accompanied by excess production of collagen, predominantly type 3, in the valve stroma, and, secondly, the theory of a primary defect in the development of the connective tissue apparatus of the mitral valve, which is combined with an increase in the number of stigmas of disembryogenesis [2, 7, 14]. The clinical manifestations of MVP are influenced by: the degree of valve prolapse, the background against which MVP is detected, the nature of electrocardiographic abnormalities, and the presence of complications [8–10, 13].
Currently, the attention of clinicians is attracted by anomalies in the development of the choral apparatus of the heart, which occur in children in an average of 38% of cases [1]. The frequency of MVP, which is also a developmental anomaly, in children ranges from 3–5% at the age of up to 1 year, increasing by 14 years to 22–31% and depends on the diagnostic method [7]. Considering the prevalence of MVP among the pediatric population, pediatricians and cardiologists need to lean toward greater clinical vigilance and prevention of possible complications [1].
The purpose of this study was to study the effectiveness of complex therapy for clinical manifestations of MVP based on the results of prospective observation of children in the cardiology department of Children's Clinical Hospital No. 5 in Zaporozhye.
Material and methods
703 children (280 boys and 423 girls) from 3 to 18 years old were under observation. There were 108 (15.36%) children aged 3 to 7 years; from 8 to 12 years - 243 (34.57%); from 13 to 18 years old - 352 (50.1%) children.
All children underwent a comprehensive clinical examination, taking into account complaints, anamnestic data, results of physical examination methods, general clinical laboratory and instrumental (electrocardiography, echocardiography with Doppler ultrasound) research methods using standard methods. To diagnose concomitant somatic pathology, the children were examined by an otolaryngologist, neurologist, ophthalmologist, orthopedic surgeon, endocrinologist, dentist, and the girls were examined by a gynecologist. The nature of cardiac disorders was assessed according to ICD-10 recommendations.
The results obtained were processed using traditional statistical methods using Excel [4, 12].
Depending on the clinical manifestations, all observed children were divided into 3 groups: MVP with rhythm disturbance and electrocardiographic symptoms (short P-Q syndrome, WPW syndrome, long QT syndrome), MVP as a manifestation of connective tissue dysplasia, and MVP with clinical signs of dysfunction of the autonomic nervous system .
The patients underwent echocardiographic examination in M- and B-modes and Doppler ultrasound in constant wave and pulse modes using an Aloka SSD-630 device. The generally accepted criteria for identifying PMC were used [1, 2, 7]. Also, two-dimensional echocardiography made it possible to detect morphological microanomalies in the structure of the valve apparatus that underlie the occurrence of mitral valve prolapse in the form of ectopic attachments or impaired distribution of tendon filaments, changes in the configuration and position of the papillary muscles, elongation of tendon filaments, and redundancy (enlargement) of the valve leaflets. Transmitral blood flow and mitral valve function were quantitatively assessed using Doppler ultrasound. Mitral valve regurgitation was diagnosed by the presence of turbulent systolic flow under the mitral valve leaflets in the left atrium. The following gradations of regurgitation magnitude were adopted:
— 1st degree (+) — systolic regurgitation in the area under the mitral valve;
— 2nd degree (++) — systolic regurgitation extends to 1/3 of the cavity of the left atrium;
— 3rd degree (+++) — spread of systolic regurgitation to 1/2 of the cavity of the left atrium;
— 4th degree (++++) — spread of regurgitation to more than 1/2 of the cavity of the left atrium [1, 7].
Results and discussion
Over the past five years, according to our observations, the number of children with MVP has increased in dynamics from 18.5% in 2002 to 29% in 2006, which is explained by both the expansion of the capabilities of ultrasound diagnosis of MVP (EchoCG) and the increase in the prevalence of connective dysplasia syndrome tissues with manifestations of dysfunction of the autonomic nervous system in children.
As a result of the study, it was established that in adolescents MVP is diagnosed significantly more often than in other age groups, with a predominance in girls in a ratio of 2: 1. In other groups of children studied, this pathology occurs equally often in both boys and girls.
All children, regardless of the severity of MVP, presented almost the same type of complaints, the variability of which varied depending on the degree of autonomic disorders. There was pain and heaviness in the heart area, a feeling of lack of air, and frequent deep sighs. A number of children experienced paroxysmal conditions, which manifested themselves as an atypical attack of suffocation, mainly after physical exertion and psycho-emotional stress. These conditions in children with severe MVP (as a rule, these are vagotonic children) were regarded as vegetative crises. Often, such children had syncope during follow-up.
Changes in the electrocardiogram (ECG) in the form of extrasystole, long QT syndrome, WPW syndrome were noted in 24% of children with MVP, MVP in combination with other manifestations of connective tissue dysplasia (joint hypermobility, myopia, high “Gothic” palate, low position of the ears, flat feet, asthenic constitution, etc.) were observed in 12% of patients, 64% of children were diagnosed with severe autonomic disorders.
According to the echocardiographic study, depending on the severity of MVP, MVP of the 1st degree was significantly more common and was recorded in 609 children examined (86.6%), MVP of the 2nd degree was detected less often - in 81 children (11.5%), 3rd degree - in 10 people (1.5%), 4th degree - in 3 children (0.4%).
The examined patients had predominantly holosystolic and late systolic variants of prolapse (98%). In 9 patients, Doppler ultrasound examination revealed 1st degree mitral regurgitation, despite the presence of MVP greater than 7 mm.
Morphometric parameters of the heart in the examined children are presented in Table. 1. The echocardiographic examination revealed in children of all age groups, in comparison with controls, only a tendency towards an increase in the size and mass of the left ventricular myocardium. The data obtained do not contradict the literature data [1] that in children with mitral valve prolapse and metabolic disorders of the myocardium, the end-diastolic volume of the left ventricle increases by an average of 20%.
Indicators of pumping and contractile function of the myocardium in the examined children are presented in Table. 2. The analysis showed that in children with MVP in all age groups, the indicators that characterized the pumping ability (EF and %ΔD) and contractility of the left ventricular myocardium (n.Sk.ser. and Sk.ts.) also tended to decrease in comparison with control groups, which is associated with the development of metabolic disorders in the myocardium.
Indicators of the systolic amplitude of movement of the posterior wall of the left ventricle and the interventricular septum, which indirectly characterize the state of the pumping function of the left ventricle, were reduced in children with MVP in all 3 age groups compared to the controls. Changes in the kinetics of the heart muscle, which turned out to be a violation of the movement of the interventricular septum and the posterior wall of the left ventricle, were mainly recorded in the form of hypokinesia of the posterior wall of the left ventricle and the interventricular septum.
Thus, in children with MVP, there are structural prerequisites for the formation of hemodynamic disorders, which are important in the diagnosis and development of diseases of the cardiovascular system in this group of patients and are characterized so far only by a tendency to increase the end-diastolic size and mass of the left ventricle with a decrease in indicators its contractility and contractility.
Taking into account the peculiarities of the clinical manifestations of MVP, we maximally individualized the treatment and management tactics of children, taking into account age, gender, heredity, the presence and nature of dysfunction of the autonomic nervous system, as well as the degree of prolapse of the mitral valve leaflets. Depending on the severity and nature of clinical manifestations, appropriate drug therapy was prescribed. Children with dysfunction of the autonomic nervous system underwent correction of autonomic disorders.
The main aspects of the recommended therapy included the normalization of the daily routine with alternating physical and mental activity. Without exception, everyone was prescribed therapeutic exercises and a visit to the pool. The department widely used physiotherapeutic treatment methods, in particular galvanization using the reflex-segmental technique. In the last 2 years, the department has introduced the administration of drugs immediately before galvanization (thiotriazoline was administered intramuscularly 2 hours before), which ensured a direct effect of the drug on the heart muscle during metabolic changes. In complex therapy, electrophoresis of medicinal substances on the upper cervical spine was widely used: for vagotonic dysfunctions - with calcium, for sympathicotonic dysfunctions - with bromine. The darsonvalization method was used very widely and successfully.
Almost all children were prescribed herbal remedies that have a sedative effect. Children with vagotonic tendencies were prescribed herbal adaptogens: tincture of ginseng, eleutherococcus.
Drugs that improve the metabolism of the central nervous system have proven themselves well. To improve microcirculation, cinnarizine was prescribed for 2–3 weeks. If changes in the rheoencephalogram of children were recorded in the form of difficulty in venous outflow, accompanied by frequent exacerbations of respiratory neurosis, bellataminal was prescribed for 2–3 weeks.
All children were required to be prescribed courses of cardiometabolites for the prevention and treatment of metabolic changes (riboxin, ATP, etc.). Antihomotoxic drugs were also used in the complex treatment of patients with MVP.
When MVP was combined with sinus tachycardia, extrasystole, long QT syndrome, and syncope, beta-blockers were prescribed: atenolol, metoprolol or propranolol in an individually selected dose (1–2 mg/kg) for 2–4 months, followed by gradual withdrawal. Beta-blockers were also recommended for children with severe mitral regurgitation and prolapse of the mitral valve leaflets of the 3rd degree. Children with persistent rhythm disturbances without prolongation of the QT interval on the ECG were prescribed antiarrhythmic drugs (cordarone). Also, in children with MVP, brain metabolites (piracetam), vascular drugs (cinnarizine), membrane stabilizers (Aevit), and antisclerotic agents (lidase) were used for heart rhythm disturbances.
Since many clinical manifestations of MVP can progress, all of our patients with this pathology were hospitalized in the cardiology department two to three times a year. A control echocardiographic study with Doppler ultrasound 6 months after complex treatment revealed clear positive dynamics in the course of the disease in 594 (84.5%) children. Among them, in 48 (8.1%) children, MVP was no longer registered, in 71 (11.9%) children, the degree of prolapse decreased, in 59 (9.9%) patients, cardiac arrhythmias disappeared and electrocardiographic study indicators normalized, in 6 (1%) patients no longer had mitral regurgitation.
Considering the existing possibility of complications from the cardiovascular system in the form of the formation of mitral valve insufficiency, secondary bacterial endocarditis, all patients with mitral valve prolapse were subsequently under medical supervision of a local pediatrician and cardio-rheumatologist, and children with an auscultatory form of MVP accompanied by regurgitation were required to undergo Antibacterial prophylaxis was carried out during dental procedures and surgical interventions.
The results of a comprehensive examination of children with MVP showed that in the occurrence of leaflet prolapse in these children, several factors were simultaneously important, the main ones being: inferiority of the connective tissue structures of the valve, minor anomalies of the valve apparatus, dysfunction of the autonomic nervous system, contributing to hemodynamic dysregulation. Timely diagnosis of MVP and a high probability of developing possible complications make it possible to recommend effective therapy, clinical observation and adequate physical activity for this group of children.
conclusions
1. Recently, there has been an increase in the number of children with MVP, especially teenage girls.
2. In the structure of all identified MVP in children, MVP of the 1st degree was significantly more common (86.6%), and less often - of the 2nd degree (11.5%), 3rd degree (1.5%), 4 th degree (0.4%).
3. Cardiac connective tissue dysplasia syndrome, represented by mitral valve prolapse, determines the presence of structural prerequisites for the formation of hemodynamic disorders in children.
4. As a result of the complex treatment, positive dynamics were observed in 84.5% of children with MVP, among whom MVP was no longer registered in 8.1%, the degree of leaflet prolapse decreased in 11.9% of those examined, heart rhythm disturbances completely disappeared in 9, 9%, and mitral regurgitation in 1% of children.
5. The prevalence of mitral valve prolapse among children dictates the need for effective therapeutic measures and clinical observation of this group of patients in order to prevent the progression of MVP and the occurrence of complications.
Frequently asked questions about mitral valve prolapse
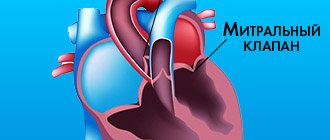
What is the mitral valve?
This is a bicuspid valve that connects the left ventricle of the heart to the left atrium. It has an oval shape and consists of connective tissue cusps, which during systole prevent the reverse flow (regurgitation) of blood into the left atrium.
What is the danger of mitral valve prolapse?
Serious complications include severe arrhythmia and bacterial endocarditis.
Can mitral valve prolapse be cured?
It is impossible to cure MVP with drug therapy. A necessary condition is a change in lifestyle, eliminating stress and excessive stress.