Mitral valve insufficiency - classification and causes
Mitral valve insufficiency is caused by a violation of the closure function as a result of deformation of the valves, often of a fibrous nature, as well as subvalvular structures and disruption of the integrity of various elements of the valve or dilatation of the fibrous ring, which ultimately leads to the return of part of the blood volume during systole from left ventricle to left atrium. This leads to a decrease in minute blood circulation and the development of pulmonary hypertension. Isolated mitral valve insufficiency is a very rare occurrence, occurring in approximately only 2% of patients. Mostly, failure is combined with mitral valve stenosis and/or aortic heart defects.
Classification and reasons
A distinction is made between functional deficiency (also called relative) or organic.
Functional mitral valve insufficiency can develop as a result of:
- Mitralization (expansion of the volume of the cavity of the left ventricle) as a result of myocardial diseases, which lead to the formation of hemodynamic overload of this part of the heart muscle.
- Acceleration of blood flow as a result of vegetative dystonia and a change in tone in the papillary muscles.
Functional mitral valve insufficiency is not a heart defect. However, hemodynamic disturbances fully correspond to the nature of organic failure. Organic mitral valve insufficiency occurs as a result of anatomical damage to the tendons of the valve filaments or the valve itself. According to the nature of the process, acute and chronic mitral insufficiency are distinguished.
General information
Acquired heart defects include defects of the mitral, aortic and tricuspid valves. rheumatism was considered a factor in the development of heart valve defects , and in recent years - infective endocarditis and degenerative changes in the valves.
The most common defects are the aortic valve (they account for 43%) and the mitral valve. The mitral valve is located between the left atrium and the left ventricle, separating them. Blood enters the left ventricle through the mitral valve from the left atrium. From the left ventricle it enters the aorta - this is the systemic circulation. The condition of the valve determines the amount of blood that will enter the large circle to supply the entire body. Mitral defects disrupt hemodynamics and affect cardiac function. They are manifested by stenosis (narrowing) or insufficiency of the mitral valve. The narrowing of the mitral orifice makes it difficult for blood to flow from the atrium into the ventricle. Mitral insufficiency is characterized by a violation of the closing function of the valve (it does not close completely), which causes the return (regurgitation) of part of the blood from the ventricle during its contraction into the left atrium.
The mitral valve apparatus consists of two leaflets, the mitral ring, papillary muscles and chordae (tendon). The valve opens towards the ventricles, and its eversion into the left atrium is prevented by tendons attached to the papillary muscles. Complete closure and brief symmetrical overlap of both leaflets prevent backflow of blood into the atrium. With mitral insufficiency due to changes in the valves or subvalvular apparatus (chordae, papillary muscles), normal hemodynamics are disrupted.
Hemodynamic disturbances inside the heart lead to a decrease in minute volume of blood circulation and at the same time an increase in pressure in the pulmonary artery ( pulmonary hypertension ). Over time, the disease progresses and patients develop heart failure , which is first eliminated conservatively, and subsequently many require surgical correction of the defect. It is important to determine the degree of progression and timely referral of patients to a cardiac surgeon to resolve the issue of surgical treatment. Patients with asymptomatic forms of defects are especially wary, since their prognosis is often unfavorable.
How to recognize prolapse?
Since in the first and second degrees the disease can occur without symptoms, you need to contact a good cardiologist in Rostov (Western) to diagnose it. A doctor can determine congenital prolapse by a number of external signs, including: above average height and elongated limbs, as well as hypermobile joints.
When visiting a cardiologist, the patient can list the following complaints, after which the doctor will prescribe an ultrasound scan:
- Frequent dizziness and faintness;
- The appearance of shortness of breath;
- Arrhythmia and interruptions in cardiac function;
- Fatigue and panic attacks;
- Chest pain.
In this case, the cardiologist will write a referral and tell you how much an ultrasound will cost to make a diagnosis. You will also need to do an x-ray and an ECG. Daily monitoring of cardiac activity and bicycle ergometry are prescribed.
The reason for clarifying the cost of ultrasound will also be noises that the doctor may detect at the appointment. To establish their cause, you will also need to do ultrasound diagnostics.
Pathogenesis
With rheumatism, all layers of the heart are involved in the process - the endocardium with valves, the myocardium, the vascular system and the pericardium. The rheumatic process causes deformation of the valve, soldering of them along the commissures, shortening of the tendon chords - all this limits the mobility of the valves. Degenerative valve changes occur in Marfan and Ehlers-Danlos . These include thickening and stretching of the valve due to collagen breakdown. At the same time, the resulting fibrous tissue causes thickening of the valves - they become dense, and shortening causes a limitation in the mobility of the valves. With this pathology, defects of the leaflets are formed along the edges, the edges are twisted, wrinkled and the leaflets are shortened, not closing during systole. Changes in the subvalvular apparatus also play a role—cicatricial shortening of the chordae and sclerosis of the papillary muscles. Subsequently, calcium is deposited in the valves, which sharply limits mobility. All these changes cause changes in intracardiac hemodynamics.
Mitral valve disease in the form of mitral insufficiency has the following hemodynamic features:
- The valves do not close completely, causing blood to return to the left atrium. The return of blood overloads the left atrium.
- The crowded left atrium begins to enlarge, and the left ventricle hypertrophies.
- The wave of regurgitation increases over time, and valvular insufficiency increases. Pulmonary hypertension develops - this is due to the fact that overload of the left atrium creates stagnation in the pulmonary circulation.
- In some cases, pulmonary edema . The contractility of the left ventricle decreases and its pumping function is weakened. Chronic heart failure develops .
The amount of backflow of blood into the atrium determines the severity of mitral regurgitation. Over time, volume overload of the left ventricle develops and the total stroke volume of the left ventricle can increase 3 times. Outflow into the aorta is normal until left ventricular failure develops. Enlargement of the left sections stretches the valve ring and contributes to the progression of insufficiency. The additional volume of blood in the atrium stretches its walls, they lose tone and at the same time the pressure in the atrium cavity and in the pulmonary veins increases (venous pulmonary hypertension develops).
Classification
The following types of mitral insufficiency are distinguished:
- organic (primary, degenerative), which develops when the valves are initially damaged;
- functional (relative, secondary), which occurs in diseases of the left ventricle.
The most common cause of chronic organic failure is valve prolapse , which has a wide range of manifestations. In young people, myxomatous degeneration is detected, in which redundancy of the valves and chords develops (in Barlow syndrome ). fibroelastic insufficiency develops , leading to rupture of the chordae. of ischemia and heart failure appear early : decreased exercise tolerance, shortness of breath.
Depending on the volume of regurgitation, several degrees of mitral regurgitation are distinguished:
- I degree. Mitral regurgitation 1st degree, what is it? This is the initial degree of deficiency. Mitral valve insufficiency of the 1st degree is characterized by mild regurgitation. Its volume is less than 30 ml, and the area of the return flow hole is less than 0.20 cm2. Reverse blood flow occurs only at the valve.
- II degree. Mitral regurgitation of the 2nd degree is characterized by moderate regurgitation and reverse blood flow in the middle of the atrium. With this degree, the atrium is moderately dilated. At grade 2, the volume of regurgitation is 30-59 ml, the area of the regurgitation opening is 0.20-0.39 cm2.
- III degree. Mitral valve insufficiency of the 3rd degree is characterized by a regurgitation volume of more than 60 ml, and the area of the return flow hole is more than 0.40 cm2. At grade 3, the atrium is significantly expanded, and the jet reaches its posterior wall. This is a severe degree of deficiency.
By stages:
- Compensation stage.
- Stage of decompensation.
In the compensatory stage, increased preload and normal afterload facilitate left ventricular ejection, so effective stroke volume is observed. The compensatory phase continues for many years.
Prolonged volume overload ultimately leads to disruption of the contractile function of the left stomach and the stage of decompensation occurs.
Types and features of mitral prostheses
Cardiac surgeons use three types of prostheses:
- Mechanical ones, which were initially made in the shape of a ball, and a little later - in the form of hinges. Blood clots often form on them, and installation may be complicated by embolism. The patient has to constantly take antiplatelet drugs. The most modern are products that are processed with a biologically intact titanium alloy.
- Biological. They are created from pericardium or other natural tissues. They do not have the ability to form blood clots.
- Allografts are taken from a corpse and cryopreserved before being implanted into a suitable donor.
Case study: advanced mitral regurgitation
I would like to give an example of a clinical case in which the lack of timely treatment led to such a diagnosis - mitral regurgitation of the 3rd degree. A patient was admitted to the hospital with complaints of severe shortness of breath at rest, worsening with physical activity, cough with sputum, which sometimes contains streaks of blood, weakness, and swelling.
He considers himself unhealthy for many years, often suffered from sore throats, and had joint problems. The deterioration occurred after suffering from acute respiratory viral infection. When listening to the lungs, fine bubbling rales are detected, a weakening of the apical impulse, a click of the opening of the mitral valve, and systolic murmur are observed. The liver is enlarged, the lower edge is determined 5 cm below the hypochondrium. EchoCG shows thickening of the valve leaflets, calcification, dilatation of the left atrium, grade III mitral valve regurgitation.
The patient is scheduled for prosthetic surgery, after which he can be saved. Get treatment on time!
Causes
Organic (primary) mitral valve insufficiency is associated with anatomical damage to the valve or the tendons that hold it. The reasons are:
- valve prolapse is a syndrome that stands on the border between normal and pathological (bending of the valves into the atrium, associated with the “weakness” of the connective tissue of the valves, so they prolapse, occurs mostly in women);
- degeneration of valve leaflets ( calcific disease , myxomatous degeneration of valve leaflets );
- rheumatic heart disease;
- infective endocarditis;
- congenital defects of the valves (splitting of the valves);
- connective tissue diseases ( scleroderma , rheumatoid arthritis , systemic lupus erythematosus );
- violation of the integrity of the mitral valve.
Rheumatic disease accounts for 14% of valve defects. The main causative agent of rheumatism is β-hemolytic streptococcus A. The main manifestation of rheumatism is carditis and valve damage ( valvulitis , the mitral valve is predominantly affected, less often the aortic valve).
Cardiac surgery, injection drug addiction, hemodialysis and long-term venous catheterization play an important role in infective endocarditis. The causative agents of this disease are Staphylococcus aureus and Enterococcus spp. due to the prevalence of diseases of the abdominal cavity and pelvic organs. In infective endocarditis, the mitral valve is most often affected.
Among non-inflammatory mitral regurgitation, dysplasia . For a long time it is asymptomatic, but as the degenerative process progresses, the weakened chords rupture and acute mitral regurgitation .
In connective tissue diseases, in particular rheumatoid arthritis , rheumatoid nodules appear in the myocardium, pericardium and endocardium at the base of the mitral and aortic valves. Subsequently, sclerosis , which causes the formation of valve insufficiency. There are also often inflammatory changes in the valves ( valvulitis ). It proceeds favorably, without causing significant deformation of the valves. But in some patients, valvulitis occurs with deformation of the valves and mitral insufficiency develops, which often requires surgical correction. Thus, rheumatoid valve damage serves as a background against which significant changes in the structure of the valves develop.
Functional tricuspid valve insufficiency is not a heart defect, but the hemodynamic disturbances with it are the same as with organic valve insufficiency. The causes of functional mitral valve insufficiency are:
- expansion of the left ventricular cavity in myocardial diseases ( hypertrophic cardiomyopathy , coronary artery disease);
- subvalvular pathology (dysfunction of papillary muscles, rupture of chordae tendineae due to infarction or valve prolapse );
- acceleration of blood flow during vegetative dystonia.
3.What to do if heart valve repair cannot be done?
In cases of aortic or pulmonary valve disease, heart surgery to replace the valve is usually performed.
During surgery, the abnormal heart valve is removed and a new valve is transplanted in its place. It could be:
- Mechanical heart valve.
The valve is made entirely of mechanical parts and materials that are well tolerated by the body. Most often this is a valve made of two carbon flaps in a ring, covered with polyester fabric. The advantage of mechanical valves is their durability and they last for many years without problems. But there are also disadvantages. Because the materials used to make the valve are artificial, you must continue to take anticoagulants (blood thinners) to prevent clots from forming in the valve after valve replacement. Clots can increase the risk of stroke. Another feature is the quiet ticking sound that is sometimes heard when the valve blades open and close. - A biological valve (bioprosthetic valve)
is made from human or animal tissue. Pig or cow tissue can be used for a bioprosthesis. Tissue valves may also have some artificial parts that help position it or create a frame. The advantage of a biological valve is that you will not need to take anticoagulants after valve replacement. But such valves are less durable and usually require replacement of the valve after about 10 years. However, recent studies have shown that some biological valves remain effective for at least 17 years. - Allograft valve.
This is an aortic or pulmonary valve obtained from a human donor. It is considered an ideal option for transplantation, especially when the patient has aortic disease or infection. When a valve is transplanted from a donor, the complete anatomy of the heart is preserved. But this valve replacement option is not always available.
About our clinic Chistye Prudy metro station Medintercom page!
Symptoms
The main manifestations of mitral valve insufficiency are:
- dyspnea;
- rhythm disturbances;
- swelling;
- heart failure , which develops earlier or later.
In some patients the defect does not appear for a long time. With mitral insufficiency, shortness of breath is less pronounced than with mitral stenosis and appears later. Circulatory failure also develops late, and hemoptysis occurs rarely.
Clinical symptoms depend on the volume of blood return from the ventricle to the atrium, on the contractile function of the myocardium and the severity of pulmonary hypertension . With the development of significant circulatory failure, treatment becomes ineffective, since irreversible changes develop in the internal organs. First of all, the heart suffers due to chronic overload. In acute mitral valve regurgitation, rapid overload of the left ventricle occurs, which increases preload on the left ventricle. This is accompanied by symptoms of left ventricular failure - pulmonary edema and decreased blood pressure .
When auscultating the heart, the doctor notes:
- weakening of the first tone;
- systolic murmur at the apex of the heart;
- splitting of the second tone.
Systolic murmur at the apex radiates into the axilla. It occurs when a backward wave passes into the left atrium through an opening between poorly closed valves.
Treatment methods
Treatment of mitral valve insufficiency at the compensation stage consists of constant monitoring of the patient, reducing physical activity and using medications to prevent the progression of the disease. If complications arise and there is no way to solve the problem surgically, symptomatic therapy is used:
- cardiac glycosides;
- diuretics;
- beta blockers;
- calcium antagonists;
- ACE inhibitors;
- anticoagulants and antiplatelet agents.
No drugs can cure the disease. Conservative methods only help to temporarily delay deterioration and improve the quality of life. The only way to fix the problem is to perform an operation.
Surgical interventions: indications and techniques
The indication for surgical treatment is a gross violation of the structure of the valves, leading to a pronounced deviation of hemodynamics. Valve restoration or replacement is required in the following cases:
- history of endocarditis;
- first manifestations of heart failure (shortness of breath, swelling);
- rhythm disturbances;
- frequent severe pain in the chest, signs of congestion in the pulmonary system.
You cannot operate in the following cases:
- onset of an acute disease or exacerbation of a chronic one;
- stroke or heart attack;
- heat;
- extreme degree of heart failure.
The main types of interventions are complete replacement or valve repair. The second option is carried out in the following ways:
- annuloplasty using soft or hard rings;
- valve resection;
- replacement of chords with artificial materials;
- edge-to-edge technique.
Tests and diagnostics
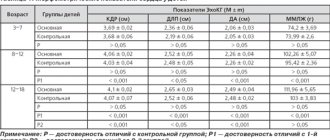
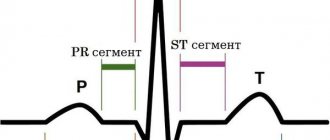
ECG . With a minor or moderately severe defect, the ECG does not change, but with severe pathology, hypertrophy of the left atrium is noted. With the development of pulmonary hypertension, hypertrophy of the right ventricle and right atrium appears. Atrial fibrillation occurs with prolonged mitral regurgitation and left atrium enlargement.
Transthoracic and transesophageal (transesophageal) echocardiography . With 3D echocardiography, the LV ejection function is determined - this is the most important indicator for the doctor. This study also evaluates the severity of the defect and the possibility of performing valve-sparing surgery. Transesophageal echocardiography is performed for prosthetic dysfunction, suspected blood clots , or infective endocarditis . Also, transesophageal echocardiography may be needed before surgical treatment to more accurately determine valve damage.
Magnetic resonance imaging . Allows you to determine cardiac function and the volume of reverse flow. CT scan. Determines the severity of valve calcification.
Chest X-ray . Diagnoses calcification of the valve and its structures. An X-ray examination reveals an enlarged heart; it has no waist due to an enlargement of the left atrium. The atrium can reach gigantic sizes. Enlargement of the left ventricle predominates over the right. X-ray reveals venous congestion in the lungs.
Bacteriological examination of blood in rheumatism and infective endocarditis . However, there is a low level of isolation of significant pathogens, which is associated with antibiotic therapy.
Diet
Diet 10th table
- Efficacy: therapeutic effect after 1 month
- Timing: constantly
- Cost of products: 1700-1850 rubles. in Week
Basic principles of dietary nutrition for patients with chronic heart failure:
- Limiting salt intake to 2g per day (in case of severe edema, it is completely excluded).
- Limiting fluid intake (0.8-1 liter).
- Frequent meals (5-6 times).
- Introducing foods that have a diuretic effect into the diet.
The more severe the heart failure, the more salt in the diet is limited. For CHF I, salty foods are excluded and no more than 3 g of additional salt can be consumed. For CHF II FC and higher, salty foods are excluded and salt is not used when preparing food (added salt is excluded).
Limiting fluid intake is recommended only in severe CHF. A weight gain of 2 kg in 1-2 days indicates fluid retention.
The diet should consist of easily digestible, high-calorie foods, high in protein and vitamins. The diet contains lean meat, vegetable and milk soups, lean fish, protein omelettes, vegetable side dishes, fruits, berries, juices (grape juice, which causes bloating, is excluded). Also limited are foods that cause bloating: beans, peas, beans, radishes.
Not recommended:
- Rich meat broths.
- Strong tea, coffee.
- Pork and animal fats.
- Smoked products.
- Canned food.
- Alcohol.
Prevention
The following will help reduce the risk of heart defects:
- Timely treatment of streptococcal infections.
- Sanitation of infectious foci.
- In case of a rheumatic attack, bicillin prophylaxis is carried out .
- Moderate hardening and a healthy lifestyle.
- To prevent infective endocarditis during dental procedures, antibacterial drugs are prescribed.
- Prescription of antibacterial drugs for invasive manipulations on the respiratory tract, gastrointestinal and urinary tracts.
Prognosis for mitral valve insufficiency
With grade 1 mitral insufficiency, the prognosis is favorable. Such patients do not need drug and surgical treatment, but they need to be monitored over time and measures are taken only if necessary. Untimely treatment for grades 2-3 leads to disability of patients. If the overload of the heart continues for a long time, they develop heart failure as a result of myocardial damage. Patients quickly become disabled - they cannot even get out of bed without shortness of breath, swelling increases and cannot be treated, and the valves of the right half of the heart are affected. Without treatment, death inevitably occurs.
In the natural course of events, only 30% survive for 5 years with myocardial ischemia , 80% survive in the absence of ischemia, and 60% survive for 10 years. An unfavorable prognosis is a decrease in left ventricular output of less than 50%, an increase in pressure in the pulmonary artery and an increase in the left atrium of more than 4.0 cm. In this case, patients do not respond to drug treatment. Timely correction of the defect cures patients. Mortality for this pathology decreased significantly after valve replacement, which indicates the effectiveness of surgical treatment. However, if atrial fibrillation occurs before surgery, survival after surgery is reduced.
List of sources
- Nesukai E.G. Mitral regurgitation/Heart failure. - 2010. - No. 3, pp. 84-91.
- Knyshov G.V., Bendet Ya.A. Acquired heart defects. /Kyiv: Institute of Cardiovascular Surgery, 1997. – 280 p.
- Kovalenko V.N., Nesukai E.G. Non-coronary heart diseases. Practical guide / K.: MORION, 2001. – 480 p.
- Shikhverdiev N.N., Marchenko S.P. Fundamentals of reconstructive surgery of heart valves / St. Petersburg: Deaton, 2007. – 270 p.
- Mitral regurgitation. Clinical recommendations. 2021. - 30 p.
- Danilov A.I., Kozlov R.S., Kozlov S.N., Dekhnich A.V. Practice of managing patients with infective endocarditis in the Russian Federation // Antibiotics and chemotherapy. 2017; 62 (1–2): 7–11.
1.What happens during normal surgery?
If surgery is required to treat heart valve disease, it can be performed traditionally, minimally invasively, or minimally invasive balloon valvuloplasty.
Traditional surgery to treat heart valve disease is performed under general anesthesia. The surgeon makes an incision in the center of the chest, thereby allowing direct access to the heart (in this case, actually open heart surgery is performed). The surgeon then operates on the abnormal valve, eliminating its defects, or replaces the heart valve.
A must read! Help with treatment and hospitalization!