General information
Aortic valve insufficiency is one of the types of heart defects acquired during life, namely the aortic valve, accompanied by hemodynamic disturbances. The pathology causes a reverse flow of blood from the aortic cavity into the left ventricular chamber during relaxation of the heart muscle (in diastole). Most often, failure is provoked by acute rheumatic fever or infective endocarditis .
In some cases, the pathology may be due to congenital anomalies, which are most often combined with damage to other valves and Marfan syndrome .
What types of valves are there?
Three types of elements can be used to replace an unhealthy valve:
- Biological. They suggest recreating a new valve from the patient’s own tissues. Such a valve will last about 10-15 years, after which the operation will need to be repeated. This is due to the gradual wear and tear of the element and its inevitable degenerative changes. With this approach, anticoagulants need to be taken only for the first six months after surgery.
- Mechanical. Such a valve is manufactured in a laboratory and requires constant use of anticoagulants (for the entire life of the patient). Such prostheses are installed mainly in patients who have not reached old age.
- Donor. This option is used only in extreme cases, as there is a risk of rejection of donor tissue by the patient's body. The outcome of such an operation is difficult to predict, and the possibility of complications cannot be excluded. In order for the valve to take root, doctors need to carry out therapy that suppresses the recipient’s immunity so that the immune system does not begin to fight the foreign element. As with the installation of an artificial valve, the patient is advised to take lifelong anticoagulants to exclude the possibility of thrombus formation.
- Available: doctor’s appointment from 1500 rubles
- Convenient: open daily from 8:00 to 21:00
- Quickly: we will carry out all the diagnostics at the first appointment
- Complete: has all the necessary equipment
Pathogenesis
The mechanism of development of this type of heart defect is based on an inflammatory-sclerotic process that affects the leaflets of the aortic valve and causes them to shrink and incompletely close. As it spreads, the aorta may also undergo pathological changes, which leads to stretching of the mouth and retraction of the valves, and the boundaries of the left ventricle also significantly expand. In addition, the addition of septic lesions and the formation of defects is possible.
Pathogenesis in aortic insufficiency
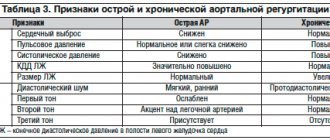
With aortic insufficiency, hemodynamic disturbance occurs: diastole occurs when the semilunar valves are not closed, which entails a reverse flow of blood from the aortic space into the left ventricle throughout the entire period of relaxation of the heart muscle. This causes its stretching (compensatory tonogenic dilatation) and hypertrophy , and diastolic pressure decreases. If blood stagnation occurs in the pulmonary circulation, then the pressure in the pulmonary arteries increases and, as a result, the development of right ventricular hypertrophy and pulmonary hypertension . Hyperfunction and hypertrophy of the right ventricle leads to the gradual development of right ventricular failure, but death may occur earlier with significant hemodynamic disturbances and left ventricular failure.
The amount of blood thrown back depends, to a large extent, on the size of the resulting pharynx in the aortic valve. Systole is accompanied by a large ejection of blood into the aorta, which leads to expansion of its initial sections.
Aortic valve disease contributes to ischemia of the muscle tissue of the left ventricle, as it experiences a greater load and an increased need for oxygen in conditions of less than the required amount of circulating blood in the coronary vessels and coronary insufficiency.
Fluctuations in blood pressure are caused by an increase in systolic blood pressure due to a significant increase in stroke volume in the left ventricle, while diastolic blood pressure is reduced due to rapid regurgitation of the blood, and as a result, numerous characteristic “peripheral” symptoms occur.
tachycardia begins to occur , causing shortening of diastole and some limitation of the reverse flow of blood from the aorta.
Risk factors
The risk of aortic regurgitation is greater if you are affected by any of the following:
- Damage to the aortic valve.
Inflammation associated with certain conditions, such as endocarditis or rheumatism, can damage your aortic valve. - High blood pressure (hypertension).
High blood pressure makes the heart work harder, increasing stress on the aortic valve, which can make it less elastic and prone to leaking. - Congenital defect of the aortic valve.
If you were born with a unicuspid or bicuspid aortic valve, your chances of aortic regurgitation increase. - Disease.
Certain conditions, including Marfan syndrome, ankylosing spondylitis and syphilis, can cause dilatation of the aortic root (where the aorta attaches to the ventricle), resulting in a leaky aortic valve.
Classification
Isolated damage to the aortic valve is quite rare - in approximately 5-9% of all diagnosed heart defects. In most cases, the pathology develops against the background of the development of stenosis of the aortic mouth and damage to other heart valves.
Aortic insufficiency can be absolute and relative, characterized by severe atherosclerosis of the aorta and the presence of dilatation of the aortic mouth in the case of hypertension .
Depending on the length of the stream during regurgitation of blood flow and the amount of regurgitated blood, various degrees of the defect are distinguished.
Aortic valve insufficiency 1st degree
For the 1st degree of aortic insufficiency, the reverse blood flow reaches 5 mm - a jet under the aortic valve leaflets, while the amount of blood thrown back is approximately 15%.
Aortic insufficiency grade 2
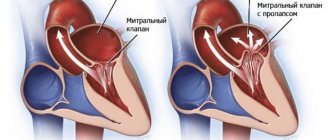
In patients with grade 2 aortic insufficiency, regurgitated blood is diagnosed to reach the mitral valve at approximately a distance of 5-10 mm, and the amount of ejected blood increases to 30%.
Aortic valve insufficiency grades 3 and 4
The most severe forms of development of the pathology, because more than half of the volume of pumped blood returns to the ventricle in a flow that reaches directly to the apex of the heart chamber, while the distance can exceed 10 mm.
Treatments and drugs
Treatment for aortic valve insufficiency depends on how severe the symptoms of the disease are and how the damaged valve affects the functioning of the heart.
Observation
Individuals with mild aortic valve regurgitation do not require treatment. However, even if you do not have signs and symptoms of aortic valve insufficiency, it is worth seeing your doctor regularly. Regular monitoring by a doctor will help to identify the progression of the disease and recommend the correct treatment.
Medicines
Medicines cannot eliminate aortic valve insufficiency. However, there are a number of drugs that help reduce the symptoms of the disease. Control your blood pressure and your weight.
Surgery
As aortic regurgitation progresses, valve replacement surgery may be required. The heart is usually good at fighting problems caused by a leaky aortic valve, the problem is that if the valve is not fixed or replaced in due time, the strength of your heart can decrease so much that it permanently weakens. You can avoid this by having surgery at the appropriate time.
Overall cardiac function and the amount of regurgitation helps determine when surgery is necessary. Surgical procedures include:
- Aortic valve plastic surgery.
Aortic valve repair is performed to preserve the valve and improve its function. Sometimes surgeons can modify the original valve (valvuloplasty) to eliminate the backflow of blood. You will not need long-term drug therapy to prevent blood clots (anticoagulant therapy) after valvuloplasty. - Valve replacement surgery.
In many cases, the aortic valve must be replaced to correct aortic valve regurgitation. Your surgeon removes your aortic valve and replaces it with a mechanical valve or a biologic valve. Mechanical valves, made of metal, are durable, but they carry the risk of blood clots forming on or near the valve. If you have a mechanical aortic valve, you will need to take anticoagulant medications such as warfarin (Coumadin) for life to prevent blood clots. Biological valves, made from pig, cow or human cadaveric donor tissue, often need to be replaced. Sometimes another type of biological valve can be used, which is your own pulmonary artery valve (autograft).
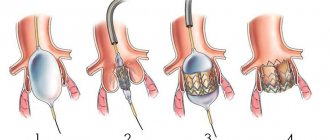
Aortic valve
Traditionally, aortic valve replacement surgery is performed on an open-heart procedure. A less invasive approach is transcatheter aortic valve implantation—installation of a new valve using a catheter through the femoral artery in your leg (transfemoral) or the left ventricle of your heart (transapical). Currently, this procedure is generally limited to those individuals who have aortic valve stenosis or aortic valve regurgitation, and carries a high risk of surgical complications. In the future, transcatheter aortic valve implantation may be an option for the treatment of aortic regurgitation.
Aortic valve insufficiency can be corrected with surgery and you will usually be back to your normal life within a few months. The prognosis after surgery is good.
Causes
Relative (functional) aortic insufficiency occurs with hypertensive disease with pronounced dilatation of the aortic mouth or with the development of aortic trismus of various origins. However, most often the pathological changes are organic and are caused by deformations and defects of the aortic valve leaflets: wrinkling, perforation, etc.
The most common causes of aortic insufficiency are:
- systemic connective tissue diseases;
- rheumatic fever;
- endocarditis of infectious origin, causing perforation of infected leaflets;
- atherosclerosis against the background of dissecting aortic aneurysm also leads to damage to the valve leaflets;
- arterial hypertension;
- aortitis;
- valve damage resulting from tertiary syphilis ;
- Marfan syndrome , which initiates myxomatous degenerative damage to both the aortic valve leaflets and the aorta;
- chest injuries, especially when valve flaps are torn off.
Important! Rheumatic endocarditis causes heart disease in 70% of cases and is combined with stenosis and disturbances in the structure of the mitral valve, the development of its insufficiency and mitralization of aortic valve disease. Pathogenesis causes thickening, deformation and shrinkage of the semilunar valve structures, initiating disturbances in closure and hemodynamics in diastole.
Acquired vices
The causes of acquired defects are severe chronic diseases, so they often develop in adulthood. The greatest connection has been established with:
- rheumatism;
- septic conditions (endocarditis);
- previous pneumonia;
- syphilis;
- atherosclerosis.
The nature of pathological changes is different:
- With rheumatic lesions, the valves are soldered at the base and wrinkled.
- Endocarditis deforms the valves, starting from the free edge. Here, warty growths are formed due to the proliferation of colonies of streptococci, staphylococci, and chlamydia. Fibrin is deposited on them and the leaflets fuse together, losing the ability to completely close.
- With atherosclerosis, the lesion passes from the aortic wall, the valves thicken, fibrosis develops, and calcium salts are deposited.
- Syphilitic changes also spread to the valves of the aorta, but are accompanied by the death of elastic fibers and expansion of the fibrous ring. The valves become dense and inactive.
The causes of the inflammatory process can be autoimmune diseases (lupus erythematosus), chest injuries.
In older people, atherosclerosis of the aortic arch leads to expansion of the root, stretching and sclerosis of the valves.
Symptoms
With relatively powerful compensatory abilities of the body, formed aortic insufficiency for many years (10-15) may not cause subjective clinical manifestations. The exception is acute heart disease caused by destruction of the valve leaflets by infective endocarditis, which can develop in just a few hours, and sometimes even minutes.
First, patients begin to feel palpitations (caused by compensatory sinus tachycardia ) and strong pulsation in the neck, head and heart due to high cardiac output and high pulse pressure in the arterial system. At the same time, there is an increased tendency to faint, which occurs due to cerebral circulatory insufficiency during a diastolic drop in blood pressure in the arteries of the brain. At the stage of decompensation, complaints indicating left ventricular failure begin to appear. Patients may experience shortness of breath , especially at the beginning of physical exercise, and then at rest, as well as attacks of breathlessness and increased fatigue . Signs of further right ventricular failure include pain in the right hypochondrium, indigestion, swelling of the lower extremities and worsening diuresis .
Clinical manifestations of aortic insufficiency usually include the following symptoms:
- dizziness and tendency to sudden fainting;
- pain in the heart area , which are angina-like in nature, having physical exertion or emotional stress as the root cause, they are difficult to relieve with nitroglycerin and usually occur at rest and at night:
- visually visible pulsation of the carotid arteries, subclavian, radial and temporal veins, which is also called the “carotid dance”;
- Musset's symptom , manifested by shaking the head back and forth in time with the pulse;
- quite rare Landolfi symptom , manifested by pulsation of the pupils with systolic constriction and diastolic dilation;
- manifestations of Quincke's symptom - “pseudocapillary pulse” with variable redness and blanching of the nail bed at the base of the root in case of intense pressure on the apex or changes in the color intensity of spots on the forehead during skin friction, which is associated with pulsation of small-caliber arterioles that are not normally capable of pulsation ;
- symptoms similar to cardiac asthma and caused by stagnation of blood in the pulmonary circulation;
- stagnation in the systemic circulation causes swelling of the neck and swelling of the legs;
- high and racing pulse;
- pulsating sensations in the area of the right hypochondrium, located in the projection of the liver;
- pseudocapillary pulse or Quincke's sign .
The role of valves in the formation of aortic stenosis
With repeated rheumatic attacks, the aortic valves shrink, and the free edges become so welded together that they narrow the outlet. The fibrous ring becomes sclerotic, further increasing the stenosis.
Symptoms depend on the degree of narrowing of the opening. A critical stenosis is considered to be a diameter of 10 mm2 or less. Depending on the area of the free aortic opening, it is customary to distinguish between the following forms:
- light - more than 1.5 cm2;
- moderate - from 1 to 1.5 cm2;
- severe - less than 1 cm2.
Patients complain about:
- pain similar to angina attacks is caused by insufficient blood flow into the coronary arteries;
- dizziness and fainting due to brain hypoxia.
Signs of heart failure appear in the event of decompensation.
During the examination, the doctor notes:
- pale skin;
- palpation is determined by a shift to the left and down the apex impulse, “trembling” at the base of the heart on exhalation, like a “cat’s purr”;
- hypotension;
- tendency to bradycardia;
- typical sounds on auscultation.
Tests and diagnostics
During physical examination, patients reveal a significant difference between systolic and diastolic pressure readings (with systolic being higher than normal and diastolic being lower). On palpation, the apical impulse is felt more dome-shaped, strong and shifted to the left and somewhat downward in conditions of an enlarged chamber of the left ventricle. Thanks to auscultation, a weakening of the first sound at the apex of the heart and a weakening of the second sound above the aorta can be heard.
In some cases, this heart defect is characterized by the detection of two sounds on the femoral artery - the Traube sound and the double Vinogradov-Durozier murmur .
Instrumental examination methods allow us to identify such signs of aortic insufficiency as:
- left ventricular hypertrophy and , left ventricular overload and relative coronary insufficiency, which are displayed on the ECG as a decrease in the ST segment and identification of a negative T wave in the first and second standard and left precordial leads, as well as possible blockade in the left bundle branch;
- thanks to echocardiography, fluttering is detected in the anterior leaflet of the mitral valve in diastole due to the impacts of the jet of reverse blood flow from the aorta;
- X-ray shows the aortic configuration of the heart - with an enlarged left ventricle or a specific “boot” shape;
- during Doppler studies, reverse blood flow into the heart chamber and diastolic reverse flows in the cavity of the abdominal aorta are detected;
- high-frequency diastolic murmurs, a decrease in amplitude towards the end of diastole and the amplitude of the second sound in patients are displayed on phonocardiography above the aorta.
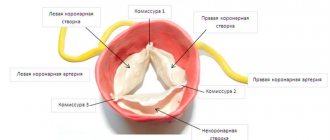
How does the aortic valve work?
The tricuspid structure of the aortic valve is distinguished from the bicuspid mitral valve by the absence of papillary muscles and tendon chords. Therefore, it opens and closes only under the influence of the difference in pressure in the cavity of the left ventricle and the aorta.
During opening, elastin fibers from the ventricle press the valves against the walls of the aorta, opening the hole for blood flow. At the same time, the aortic root (the initial part) contracts and pulls them towards itself. If the pressure in the ventricular cavity exceeds the pressure in the aorta, then blood flows into the vessel.
The valves close with swirling currents in the area of the sinuses. They move the valve away from the walls of the aorta towards the center. Elastic flaps close tightly. The closing sound is heard with a stethoscope.
Diet for aortic valve insufficiency (aortic insufficiency)
Diet for cleansing blood vessels for diseases of the cardiovascular system
- Efficacy: therapeutic effect after 3 months
- Timing: constantly
- Cost of products: 1700-1800 rubles. in Week
Treatment of aortic insufficiency occurs under conditions of limited physical activity, which should be taken into account in nutrition. In addition, if you have heart problems, you should avoid:
- fried, smoked and fatty;
- too peppery and salty;
- refined sugar - in candies, ice cream, cakes, etc.
You also need to limit salt consumption - no more than 5 g and saturate your diet with healthy vegetables, dried fruits, herbs, berries, seafood and offal.
Postoperative period
The recovery period is the most important stage, which has its own characteristics. For the first time after replacing the valve, physical activity and strong psychological experiences are prohibited. Caution must be exercised for at least three years after the intervention. Professional athletes can return to full training only after six years. Taking anticoagulants prescribed by a doctor is a must. It is also very important to regularly check the condition of the body and monitor for possible concomitant pathologies.
In fact, the valve itself will not affect the patient's future health in any way. If irreversible changes have occurred, the patient needs constant monitoring by a cardiologist.
How do adaptive mechanisms work?
As a result of incomplete closure of the semilunar valves, the returned blood forces the left ventricle to work harder and push out more blood. It expands and lengthens. After some time, muscle hypertrophy occurs. It is quite enough to compensate for the defect for many years.
In patients with rheumatism, repeated attacks lead to decompensation due to myocardial overload. Heart failure develops.
It is worth noting the peculiarity of the development of the decompensatory mechanism in syphilis: after inflammation, cicatricial deformation occurs at the base of the aorta. This is where the coronary vessels arise. Therefore, their mouth narrows and becomes deformed. Disturbance of the blood supply to the myocardium predominates.
Diagnostic examination methods
If any signs indicating problems with the heart appear, an examination by a cardiologist is immediately required. In addition to collecting anamnesis, the doctor prescribes the necessary types of hardware diagnostics.
The very first method that will reveal the presence of congenital heart disease in the form of a bicuspid aortic valve is echocardiography (a type of ultrasound (you can watch it on video), which allows you to identify not only the presence of an anomaly, but also the degree of regurgitation).
In addition, diagnostics may include:
- radiography;
- electrocardiogram;
- Doppler study;
- cardiac catheterization.
Diagnosis confirmation methods
Diagnosis is usually not difficult. The age of the patient helps in determining the cause.
- Typically, children and young people are characterized by rheumatic lesions or the consequences of infective endocarditis.
- In middle age, manifestations of syphilis are more typical.
- In older people, atherosclerosis is the main disease.
ECG signs reveal significant hypertrophy of the left ventricle, in later stages - both ventricles and the left atrium.
Phonocardiography allows you to synchronously record noise; the diagram shows the point of maximum noise of the aorta
The x-ray shows expanded contours of the cardiac shadow, displacement of the apex outward and downward, and expansion of the ascending portion of the aortic arch.
Echocardiography and ultrasound make it possible to record the increase in the volume of the left ventricle, mitral valve flutter, and the magnitude of regurgitation.
The introduction of a catheter into the cavity of the heart allows you to accurately measure the amount of cardiac output and the volume of returned blood.
Laboratory tests play a role in determining the cause of aortic regurgitation.