- home
- Articles
- Schedule of illnesses
- Can you join the army if you have a heart defect?
»
»
»
Updated: November 27, 2021
Free hotline for conscripts and their parents
8
Young people of pre-conscription age often hear stories from their friends that one of them had to serve in the army with congenital or acquired heart disease. Such situations do happen in practice. Therefore, the answer to the question of whether someone with a heart defect will be accepted into the army in 2022 is ambiguous and may depend on various circumstances.
Conditions for exemption from the army with congenital heart disease
Heart defects, both congenital and acquired, are not a separate diagnosis in themselves. This is a group of diseases of the cardiovascular system. These include multiple pathologies that can occur in different ways.
The decision on whether a conscript will serve in the ranks of the Russian armed forces is made by the military conscription commission based on the following indicators:
- the presence or absence of heart failure in a young person;
- the degree of regurgitation - the reverse outflow of blood as it moves through the heart;
- indicator of heart valve function;
- the state of health and well-being of the young man at the time of passing the military conscription commission.
All of these factors together have a direct impact on the results of the medical examination, on the basis of which the conscript is sent to the army, released from service or removed from military registration.
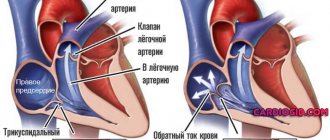
Regurgitation on the tricuspid valve
Tricuspid regurgitation
- This is the leakage of blood in the opposite direction through the tricuspid valve each time the right ventricle contracts. The tricuspid valve is located in the opening between the right atrium and the right ventricle.
The tricuspid valve opens, allowing blood from the right atrium to enter the right ventricle, and closes when the right ventricle contracts, pushing blood into the lungs. If the tricuspid valve does not close completely, some blood leaks back into the right atrium - called regurgitation.
Tricuspid valve insufficiency can be primary or secondary (the most common).
Causes
Symptoms
Diagnostics
Diagnosis is based on history, physical examination, and examination results. To clarify the diagnosis, the doctor may prescribe the following types of examination:
- electrocardiography (ECG);
- X-ray examination of the chest organs;
- echocardiography;
- magnetic resonance imaging (MRI) of the heart;
- cardiac catheterization.
Obtaining category “B” or “D” according to the UPU
The basis for exemption from conscription for young people with congenital heart disease is their assignment of fitness category “B” or “D”. You can receive one of these categories if the conscript’s circulatory system defect is included in the list of diagnoses in the corresponding article of the Schedule of Diseases for which service in the Armed Forces of the Russian Federation is prohibited.
The reasons why a young man cannot fulfill his military duty and be involved in military training may lie in the presence of the following pathologies:
- isolated aortic heart disease and heart failure of functional class II–IV, which is determined through medical research by specialists in the field of cardiology;
- congenital heart disease with heart failure II, stage II regurgitation and valve insufficiency (aortic, mitral and tricuspid).
All of the listed pathologies are the basis for assigning a conscript the fitness category “D”. The young man is completely exempt from the army, receives a military ID and is removed from the military register.
Category “B” can be assigned to a young person with impaired development of the interatrial septum or congenital heart valve defects.
Conscripts with fitness category “B” are not called up for military service in peacetime, but at the same time they are not removed from the military register, but are enlisted in the reserves. In the event of general mobilization, these individuals may be assigned to certain types of troops with certain restrictions.
Need help getting out of the army?
Call us at 8 (800) 550-25-66 or leave a request and we will answer any questions about the army and obtaining a military ID.
Request a call
Problems a recruit may encounter
It happens that even with a non-conscription diagnosis, a young man is given a draft eligibility category. This can happen for various reasons, but let's look at the most common one.
After passing the military medical commission, specialists write a referral for an additional examination to the conscript, he will need to undergo it. As soon as he receives all the results of tests and studies, the doctor responsible for conducting the additional examination is obliged to confirm the presence of a diagnosis, or indicate its absence. At this stage, the most common problem may arise - the specialist indicates an incorrect formulation of the diagnosis.
In this case, even if the conscript has a non-conscription illness, he may be sent to serve. It is necessary to carefully check the wording indicated by the specialist in the extract. To obtain an exemption, it is very important that this wording is exactly the same as provided in the Schedule of Illness document. If you make a mistake, you may not hope to receive a military ID due to health reasons. The maximum that you can be given is a deferment from the army in case of regurgitation.
Who is recruited into the army with a heart defect?
Congenital heart disease is a pathology that is always perceived by people as a danger to human life. But there are exceptions to all rules. Sometimes heart disease is not a reason for exemption from conscription. In such cases, young people are recruited into troops that do not require much physical exertion.
For example, they can be called up for service if they have a bicuspid aortic valve, provided there are no violations of its functions, if the disease is compensated and there are no signs of regurgitation.
Sometimes young people are mistaken, classifying such a disease as open oval window among heart defects. Despite the fact that there is constant debate between cardiologists about this diagnosis, today it is usually classified not as a congenital defect, but as a minor anomaly in the development of the heart.
This disease has certain characteristics - it is not always confirmed during additional examination. Often young people who have lived with this diagnosis since childhood, after undergoing diagnosis, learn that they are fit to serve in the army. This is because during blood drainage there is a risk of misdiagnosis.
But even if the disease is confirmed, the conscript can be enlisted in the Russian army, because in the absence of blood outflow, the young man is considered fit for service.
Is he fit to have this diagnosis?
Suitable for the diagnosis: Fragmentary, marginal sealing of the aortic valve leaflets. Aortic - valvular regurgitation of the 1st degree. Mitral - valvular regurgitation of the 1st degree. Tricuspid - valvular regurgitation of the 1st degree. Pulmonary valve regurgitation grade 1. False chord of the left ventricle Bradycardia.
ANSWERS TO QUESTION (1)
The presence of aortic valve regurgitation makes you unfit for at least point “c” of Article 80 of the Schedule of Diseases:
isolated congenital heart defects in the absence of chronic heart failure;
Aortic regurgitation of any degree is aortic valve insufficiency as explained below (page 92):
A violation of intracardiac hemodynamics should be considered constant regurgitation of grade I or more. Prevalvular (minimal) regurgitation refers to grade I regurgitation. If grade I regurgitation is detected on the aortic valve, it should be regarded (regardless of other indicators) as aortic valve insufficiency.
And aortic valve insufficiency is an isolated congenital heart defect, as is clear from point “a”:
isolated congenital heart defects (aortic stenosis, pulmonary artery stenosis, left atrioventricular orifice stenosis, aortic valve insufficiency, (mitral) valve, prolapsed aortic valve leaflets, bicuspid aortic valve , myxomatosis, aneurysm of the interatrial septum, interventricular septum or sinus of Valsalva, fenestration of the valve leaflets with blood regurgitation, patent ductus arteriosus, ventricular or atrial septal defect, etc.)
Source
Acquired heart disease and military service
During life, the human body is exposed to many factors that can lead to various defects in the structure of the heart valves. As a result, disturbances in blood flow within the organs of the cardiovascular system often occur. These pathologies are called acquired heart defects (HADs). PPS are often the cause of other serious problems, such as arrhythmias and tachycardia.
There are several types of PPP:
- stenosis, in which there is difficulty in blood flow;
- heart failure, in which the functionality of the valve decreases and, as a result, it becomes impossible to prevent blood flow in the opposite direction.
If one of these pathologies occurs, as well as if insufficiency is observed in only one valve, the acquired heart defect is called simple. In the presence of both disorders or damage to several valves - combined.
The following diseases can lead to the occurrence of these disorders:
- rheumatism;
- infective endocarditis;
- autoimmune diseases;
- neoplasms; heart attack, etc.
Category “D” is assigned to young people if they have the following pathologies:
- insufficiency of III-IV functional class;
- isolated stenosis in the left atrioventricular orifice;
- cardiomyopathy and obstruction in the outflow tract in the left ventricle;
- consequences of surgery on heart valves.
Category “B” is assigned if there is:
- primary prolapse in the valve, myocardial cardiosclerosis with persistent deviation of heart rhythm;
- consequences of operations aimed at treating heart disease.
Read more about whether you will be allowed to serve with prolapse.
When diagnosing isolated PPS, category “D” or “B” can be assigned based on parameters of heart failure. In other cases, there is a high probability that the conscript will receive category “B-4” with subsequent conscription into the army.
Aortic regurgitation (aortic valve insufficiency)
Aortic regurgitation
is the backflow of blood through the aortic valve into the left ventricle when the left ventricle relaxes during each cardiac cycle. The aortic valve opens when the left ventricle contracts and pushes blood into the aorta. If the aortic valve leaflets do not close completely, backflow of blood from the aorta into the left ventricle occurs.
To compensate for the load on the heart, the muscular walls of the ventricles thicken (hypertrophy) and the chambers of the ventricles increase in size (dilate). Eventually, despite this compensation, the heart loses its ability to meet the body's blood needs, leading to heart failure with fluid accumulation in the lungs.
Aortic valve regurgitation can develop suddenly (acute) or gradually (chronic).
Causes
Acute aortic regurgitation
- Valve infection (infective endocarditis)
- Rupture of the aortic lining (aortic dissection)
Chronic aortic regurgitation
- Spontaneous weakening of the valve or ascending aorta (congenital defect)
- Rheumatic fever
Symptoms
- Heart murmurs
- Dyspnea
- Chest pain
- Heartbeat
Mild aortic regurgitation causes no symptoms other than a characteristic heart murmur that can be heard with a stethoscope whenever the left ventricle relaxes. Symptoms in people with severe regurgitation may occur as heart failure develops.
Heart failure causes shortness of breath on exertion. The patient's breathing is difficult when lying down, especially at night. Changing to a sitting position allows accumulated fluid to drain from the top of the lungs, which helps restore normal breathing. Some patients with aortic regurgitation experience chest pain due to insufficient blood supply to the heart muscle (angina), especially at night.
The pulse, sometimes called a racing pulse, becomes momentarily strong and then quickly disappears as blood leaks back through the aortic valve into the heart, causing blood pressure to drop sharply.
Diagnostics
The diagnosis is based on the results of a medical examination (namely, a jumping pulse and characteristic heart murmurs) and is confirmed through examination. For this purpose, the doctor may prescribe:
- echocardiography;
- computed tomography (CT);
- magnetic resonance imaging (MRI);
- X-ray examination of the chest organs;
- electrocardiography (ECG);
- coronary angiography (before surgical treatment).
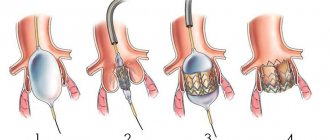
Treatment
Drug treatment is not particularly effective in slowing the progression of heart failure. Treatment depends on the cause and symptoms of the disease, the severity of the disease, as well as the presence of comorbidities and drug therapy received for the comorbidity. Taking this into account, the doctor may prescribe:
- medications;
- heart valve replacement.
Source
Diagnostics
To confirm the presence of a congenital or acquired heart defect, it is necessary to submit to the military conscription commission all documents indicating the presence of the disease. Pathology can be confirmed by the results of the following medical tests: echocardiography, electrocardiography, stress tests, radiography, cardiac catheterization and MRI.
Ivan Golubkin
Legal specialist and manager. Experience in the legal field - more than 10 years, in the field of assistance to conscripts - more than 3 years. Writes useful articles for conscripts.