Aortic regurgitation refers to a heart defect in which damage to the aortic valve prevents the semilunar valves from closing completely. This causes a characteristic circulatory disorder. When the heart contracts, blood is ejected from the left ventricle and then flows through the aorta into other vessels. In the absence of pathology in this area, the aortic valve flaps are completely connected, and this prevents blood from returning back. Blood moves through the aorta, completing its circulation. But if a pathology such as aortic valve insufficiency develops, normal blood flow is disrupted, the aortic valves do not completely close the aortic opening and part of the blood returns back to the left ventricle. Blood from the left atrium also arrives at the same time. There is much more blood in the left ventricle than it should be, it becomes overfilled, it rises, it needs to cope with a large volume of blood, making great efforts to maintain blood flow. Over time, as a result of this increased load, the muscle that pushes blood out becomes thicker. In addition, against the background of aortic insufficiency, the heart itself does not receive sufficient nutrition due to impaired coronary blood flow. This further aggravates the heart condition. Aortic valve insufficiency can be an isolated defect, or it can occur in various forms with other heart defects.
Symptoms
Given the large compensatory capabilities of the myocardium, the disease can be asymptomatic for a long time. And even when doing physical exercise, a person may not immediately feel any symptoms. Further progression of coronary and cerebral disorders lead to the appearance of the first symptoms in the form of dizziness, weakness, fatigue, increased heart rate and increased heart rate. Aortic insufficiency is manifested by tachycardia, felt at rest, symptoms intensify after physical exertion. There is pallor. Shortness of breath and angina attacks develop, which are poorly relieved by nitroglycerin.
A person with aortic valve insufficiency has external characteristic manifestations. He can see the pulsation of the cervical vessels “carotid dance” and he shakes his head in time with the pulse. When measuring blood pressure, increased systolic pressure is detected, but diastolic pressure always decreases, sometimes down to zero. Blood pressure always changes. The pulse is fast, high, large. An intensified elevating apical impulse is detected. The heart expands to the left.
When listening, there is a weakening of the first tone at the apex, and a weakening of the second tone above the aorta (with severe destruction of the valve leaflets - until it completely disappears). A soft blowing diastolic murmur appears in the third intercostal space on the left and above the aorta. It can be heard more clearly if the patient exhales completely and holds his breath. Changes in blood flow that occur against the background of this defect cause a large expansion of the left ventricle, leading to mitral valve insufficiency. This will be manifested by the appearance of a systolic murmur. It is heard at the apex of the heart. Less common is Flint's diastolic murmur. Sometimes with this defect you can hear two noises on the femoral artery.
Complications
Complications of aortic insufficiency develop as its severity increases. At the beginning, normal syncope (fainting) may appear due to insufficient blood supply to the brain. Conduction disorders in the form of blocks of the left bundle branch and atrioventricular conduction of impulses can also often occur in patients with aortic insufficiency.
Coronary insufficiency can accompany aortic insufficiency, but more often in combination with aortic valve stenosis. The patient develops attacks of angina (pain in the heart of a pressing, squeezing nature) and even myocardial infarction.
Heart failure is the most common complication of already severe aortic regurgitation. The patient complains of shortness of breath during physical exertion, asthma attacks, and swelling of the lower extremities.
Sudden death often develops as a result of life-threatening arrhythmias - paroxysmal ventricular tachycardia, ventricular fibrillation. In this case, the person does not even have time to call an ambulance - the arrhythmia develops so quickly.
Diagnostics
First of all, the doctor can think about the presence of aortic valve insufficiency based on the results of the examination of the patient. Because the manifestations of this pathology have their own characteristics, revealed externally and by listening. As mentioned above, at a certain stage in the development of the disease, the patient’s characteristic appearance appears and heart murmurs appear. The diagnosis is confirmed after special research methods. Echocardiography can detect signs of this defect in the form of reverse blood flow, increased work of the muscular wall of the left ventricle in systole, and fluttering of the mitral valve as blood fills the left ventricle. A phonocardiogram clearly reveals changes in tones and noises that identify this defect. ECG and x-ray of the heart may not detect changes for a long time. They are detected already in the later stages, when left ventricular hypertrophy develops.
Causes and risk factors
Aortic valve insufficiency develops due to loose closure of the valves during the relaxation phase of the ventricles, which can develop for a number of reasons:
- idiopathic (unknown cause) dilation of the aorta;
- congenital defects of the aortic valve (usually bicuspid aortic valve);
- sclerosis of the valves (due to atherosclerosis);
- rheumatism;
- infective endocarditis;
- arterial hypertension;
- myxomatous degeneration (disorder of connective tissue development);
- dissection of the ascending aorta;
- Marfan syndrome;
- aortic valve injuries;
- ankylosing spondylitis;
- syphilitic aortitis;
- rheumatoid arthritis.
Most of these causes lead to chronic aortic insufficiency, which can be asymptomatic for a long time. Others, in particular infective endocarditis, aortic dissection, and trauma are often accompanied by a sudden development of severe aortic insufficiency. This leads to serious hemodynamic disturbances. As a result, much less blood reaches vital organs: the brain, kidneys, liver, heart.
Treatment of aortic valve insufficiency
There are two types of treatment for this pathology. Aortic insufficiency is eliminated if treated with surgery, which radically solves the problem. In this case, an artificial valve is implanted. But the positive outcome of such an operation depends on the severity of the changes that have occurred in the myocardium.
Aortic valve insufficiency is treated conservatively; treatment is aimed at reducing the symptoms of this disease, which can be eliminated temporarily. At the same time, the time of onset of heart failure is delayed. The conservative method is aimed at maintaining the functioning of the heart and improving the condition of other organs. In order to prevent cerebral circulatory failure, as well as coronary circulatory failure, it is necessary to maintain a sufficient heart rate. This becomes possible with the use of cardiac glycosides (korglykon, strophanthin and others).
Vitamins, cocarboxylase, and riboxin are also used to maintain nutrition of the heart muscle. If complications occur, their treatment is prescribed.
Forecast
The prognosis for aortic insufficiency is better, the lower the degree of regurgitation and the earlier treatment is started. Preventive examination by a general practitioner, cardiologist, full antibiotic therapy in case of infective endocarditis and rheumatic fever - all this helps to improve the prognosis. It is very important to listen to yourself, your body, so as not to miss the first symptoms (lethargy, decreased performance, fainting, shortness of breath during physical activity).
Usually, with severe clinical heart failure, the prognosis worsens, since irreversible changes occur in the structure of the heart.
Pathogenesis
The mechanism of development of this type of heart defect is based on an inflammatory-sclerotic process that affects the leaflets of the aortic valve and causes them to shrink and incompletely close. As it spreads, the aorta may also undergo pathological changes, which leads to stretching of the mouth and retraction of the valves, and the boundaries of the left ventricle also significantly expand. In addition, the addition of septic lesions and the formation of defects is possible.
Pathogenesis in aortic insufficiency
With aortic insufficiency, hemodynamic disturbance occurs: diastole occurs when the semilunar valves are not closed, which entails a reverse flow of blood from the aortic space into the left ventricle throughout the entire period of relaxation of the heart muscle. This causes its stretching (compensatory tonogenic dilatation) and hypertrophy , and diastolic pressure decreases. If blood stagnation occurs in the pulmonary circulation, then the pressure in the pulmonary arteries increases and, as a result, the development of right ventricular hypertrophy and pulmonary hypertension . Hyperfunction and hypertrophy of the right ventricle leads to the gradual development of right ventricular failure, but death may occur earlier with significant hemodynamic disturbances and left ventricular failure.
The amount of blood thrown back depends, to a large extent, on the size of the resulting pharynx in the aortic valve. Systole is accompanied by a large ejection of blood into the aorta, which leads to expansion of its initial sections.
Aortic valve disease contributes to ischemia of the muscle tissue of the left ventricle, as it experiences a greater load and an increased need for oxygen in conditions of less than the required amount of circulating blood in the coronary vessels and coronary insufficiency.
Fluctuations in blood pressure are caused by an increase in systolic blood pressure due to a significant increase in stroke volume in the left ventricle, while diastolic blood pressure is reduced due to rapid regurgitation of the blood, and as a result, numerous characteristic “peripheral” symptoms occur.
tachycardia begins to occur , causing shortening of diastole and some limitation of the reverse flow of blood from the aorta.
Acquired heart defects (AHD)
Heart valve defects
Valvular heart disease is characterized by damage or defect of one of the four heart valves: mitral, aortic, tricuspid or pulmonary.
The mitral and tricuspid valves control the flow of blood between the atria and ventricles (the upper and lower chambers of the heart). The pulmonary valve controls the flow of blood from the heart to the lungs, and the aortic valve regulates the blood flow between the heart and the aorta, and therefore the blood vessels to the rest of the body. With normal heart valve function, blood flows with the proper force in the right direction at the right time.
With a heart defect, the function of the valve is impaired; it can become too narrow (stenosis), which is why it does not open completely, or expand and cannot close completely (insufficiency). A narrowed valve prevents blood from flowing out of the chamber of the heart, while when it fails, the blood flows back into the chamber from which it previously came out. Impaired valve function leads to enlargement and thickening of the heart muscle, reducing its elasticity and efficiency.
The most common defects are the mitral and aortic valves.
The severity of heart disease varies. In mild cases there may be no symptoms, but in advanced cases the defect can lead to congestive heart failure and other complications. Treatment depends on the extent of the disease.
Causes of heart valve defects
There are many reasons. Some of them are present at birth (congenital), while others can be acquired later in life:
- aging of valves: heart valve tissue can degrade with age due to atherosclerosis, lose elasticity and become hard;
- rheumatism;
- bacterial endocarditis;
- high blood pressure;
- myocardial infarction;
- heart tumors
- systemic diseases (rheumatoid arthritis, systemic lupus erythematosus, syphilis);
- radiation therapy used to treat cancer.
Symptoms that may appear due to heart valve disease
Symptoms of heart disease can occur suddenly, depending on how quickly the disease progresses. When the disease progresses slowly, your heart may adjust and you may not notice the onset of any symptoms. It is important to understand that the severity of symptoms is not equivalent to severe heart valve disease and, conversely, symptoms may be completely absent in cases of severe heart valve disease.
Symptoms of heart disease include:
- Shortness of breath during exercise, fatigue
- Swelling of the extremities, rapid weight gain due to fluid accumulation
- Palpitations or irregular heartbeat
- Chest pain
- Dizziness or fainting
- Fever (if the valve is infected)
To identify and treat heart valve diseases, correct and timely diagnosis is important.
Diagnosis of defects
Valvular heart disease can be detected by listening to characteristic sounds known as heart murmurs.
To fully diagnose the defect, you need to undergo one or more of the following studies:
- An electrocardiogram (ECG) shows the heart's electrical activity, regularity of heartbeats, thickening (hypertrophy), and damage to the heart muscle from coronary artery disease.
- A chest x-ray shows enlargement of the heart chambers due to dysfunction of the heart valves.
- Echocardiogram (EchoCG) is the gold standard in modern diagnostics. In an echocardiogram, sound waves bouncing off the heart are recorded and converted into images. The scans can reveal abnormal size, shape, and movement of the heart and valve dysfunction.
- Coronary angiography, which involves inserting a catheter into the heart to assess the condition of the vessels supplying the heart.
Mitral valve defects
There are three types of mitral valve dysfunction:
- Mitral valve prolapse is when both valve leaflets are enlarged and bulging, preventing them from closing evenly.
- Insufficiency is when the valve leaflets do not close tightly, causing blood to leak back into the left atrium of the heart. Deficiency can occur suddenly (acute) or, more often, gradually over time (chronic). Acute mitral valve regurgitation is often caused by damage to the heart, such as a heart attack or infective endocarditis.
There are many reasons why chronic mitral valve insufficiency can develop. Symptoms include fatigue, shortness of breath on exertion and while lying down, and irregular heartbeat.
- Stenosis—the mitral valve leaflets thicken, become rigid, and may even fuse together. Because of this, the valve opening narrows. Among adult patients, stenosis is more common in women, and the main cause is rheumatism. Symptoms include shortness of breath on exertion, swelling of the lower extremities, and cardiac arrhythmias. In some patients, clots (thrombi) form in the left atrium. These clots can travel through blood vessels and damage the brain, spleen, or kidneys.
Aortic valve defects
Aortic valve regurgitation occurs when the valve leaflets do not close and blood flows back into the left ventricle of the heart. A patient may have significant aortic regurgitation for many years without developing significant symptoms. Signs of the disease include palpitations, shortness of breath on exertion or while lying down (there may be sudden severe shortness of breath in the middle of the night), chest pain.
Aortic valve stenosis affects men more often than women. This is a condition where the valves thicken, become stiff and fuse together, narrowing the valve and preventing the normal flow of blood from the heart to the aorta and the rest of the body. Aortic valve stenosis usually does not cause symptoms until the valve opening has narrowed to about one-third of normal size. Symptoms include shortness of breath on exertion, chest pain, and fainting.
Tricuspid valve insufficiency
This is a heart defect characterized by incomplete closure of the tricuspid valve leaflets and the reverse flow of blood from the right ventricle into the right atrium.
Damage to the tricuspid valve, like other heart valves, can be caused by rheumatism, myxomatosis, infective endocarditis, or chest trauma.
Tricuspid valve insufficiency may also not be associated with damage to the valve itself, but may arise as a result of a long course of mitral and aortic defects, in the absence or improper treatment of them.
Treatment of heart valve defects
Treatment for heart valve disease will depend on the type and severity of the condition and may include medication or surgery.
If the heart defect is significant and medications do not help, surgery is performed to repair or replace the heart valve. Currently, heart valve surgery strives to perform valve-sparing operations. Thanks to improvements in reconstructive surgery techniques, it is possible to restore the valve even with infective endocarditis. In other cases, the valve is replaced with an artificial prosthesis.
Artificial heart valves
Artificial heart valves have improved significantly since their invention, and cardiac surgeons now have prostheses that can perform the function of their own valve as closely as possible.
Depending on the composition, artificial heart valves can be mechanical or biological. Mechanical valves are made entirely of synthetic materials, their advantages are strength, durability and wear resistance. The disadvantage is the need for lifelong use of anticoagulants (blood thinners) to prevent the formation of blood clots.
Artificial heart prostheses
Biological valves are made from animal heart tissue and treated with special solutions that increase wear resistance and prevent immune rejection after implantation. The advantages of biological prostheses are that there is no need for lifelong use of anticoagulants. Disadvantage: rapid wear, limited age of the patient. Biological prostheses are recommended for patients over 70 years of age; their service life is about 10-15 years.
Heart surgery
In most cases, the surgeon makes an incision in the middle of the sternum to reach the heart, uses a heart-lung machine to circulate blood throughout the body during surgery, stops and opens the heart to reach the diseased valve, then repairs or replaces the valve.
Heart valve surgery is also performed through a small incision on the right side of the chest using video support.
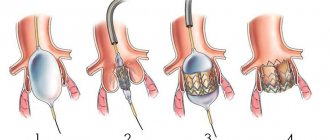
Patients with aortic stenosis can undergo aortic valve replacement with a biological prosthesis through the femoral artery or the apex of the heart - without cutting the sternum and stopping the heart. This operation is performed on older patients at high risk of standard open heart surgery. In this case, only biological prostheses are implanted.
After heart surgery
The World Health Organization (WHO) has defined health as not only the absence of disease and illness, but also the presence of physical, mental and social well-being. The goal of heart surgery is not only to prolong life, but also to improve functional mobility and quality of life.
Open heart surgery is a major procedure and requires time to fully recover. It depends on the age and general health of the person, as well as the complexity of the operation.
If you seek surgical help in a timely manner, it is possible to avoid postoperative complications and go through a short recovery path in almost 100% of cases.
During the first two weeks the patient feels tired and weak, the general condition gradually recovers over the next month. During this period, you need to limit heavy physical activity and give up sports. You need to leave the house at least 2 times a day for a short walk and try to increase your load a little every day. The sternum will heal completely within two months, after which it will be possible to return to normal household activities.
For many patients, returning home after heart surgery is a great relief, but for some it can be quite frightening. Follow the recommendations of your doctor, take prescribed medications on time, the duration and quality of your life depends on this.