Transcatheter aortic valve replacement (TAVI) is a minimally invasive surgical procedure that replaces a heart valve.
The most common pathology of the valve apparatus is aortic stenosis . The disease is treated only with surgical methods.
According to statistics, classical surgery using artificial circulation for 11-15% of patients in the older age group with concomitant diseases is associated with a high risk of hospital mortality. For this reason, 33% of patients with aortic stenosis are denied classical surgery involving aortic valve replacement.
An alternative surgical method is the TAVI procedure. Implantation of a bioprosthetic aortic valve is carried out on a beating heart. A special catheter is inserted through the femoral artery to deliver and implant a replacement aortic valve.
Symptoms of aortic stenosis
Patients with aortic stenosis exhibit the following general clinical signs:
- headache;
- increase or decrease in blood pressure;
- bradycardia (heart rate less than 60 beats per minute);
- pale skin.
When examining a patient, the doctor additionally discovers:
- “trembling” of the chest, resulting from the passage of blood through the narrowed opening of the valve;
- wheezing in the lungs;
- When listening, it detects faint sounds of valve flaps closing, accompanied by additional noise.
Depending on the degree of narrowing of the aortic mouth, other symptoms may appear:
- dyspnea;
- increased fatigue during physical activity;
- dizziness;
- fainting;
- attacks of suffocation;
- swelling of the lower extremities;
- ascites;
- pain in the right hypochondrium that occurs against the background of an enlarged liver due to blood stagnation.
The fifth degree of aortic stenosis is accompanied by severe shortness of breath, edema of the whole body and acrocyanosis.
Implantation of a bioprosthetic aortic valve through TAVI is indicated for patients with degree 2 or 3 aortic stenosis.
Contraindications for surgery
Heart valve replacement surgery is contraindicated for the following diseases and conditions:
- Acute myocardial infarction,
- Acute cerebrovascular accidents (stroke),
- Acute infectious diseases, fever,
- Exacerbations and worsening of chronic diseases (diabetes mellitus, bronchial asthma),
- Extremely severe heart failure with an ejection fraction of less than 20% with mitral stenosis, in which case the attending physician should decide whether a heart transplant is necessary.
Diagnosis of aortic stenosis before TAVI
The following diagnostic measures can help determine aortic stenosis in a patient:
- electrocardiogram (arrhythmia, blockades are determined);
- exercise electrocardiogram;
- radiography (the expansion of the aortic section located above the stenotic area is visualized, an enlargement of the left ventricle of the heart is detected, and calcification of the orifice is determined);
- echocardiography (an increase in size and thickening of the walls of the aortic valve is visualized, left ventricular hypertrophy is established);
- Doppler echocardiography;
- catheterization of cardiac chambers;
- coronary angiography.
Preparing for surgery
Once a diagnosis of heart disease or infective endocarditis has been made, the decision regarding the need to replace the affected valve should be made as soon as possible. After this, the patient undergoes the required minimum of clinical studies and is referred by the attending physician to the cardiac surgery center. Typically, surgery can be performed within a few months of diagnosis. If a patient submits an application to the regional health department for a quota (budgetary allocations from the federal budget to provide high-tech assistance to the population), then a response to the quota can be received within 20 days.
For admission to the cardiac surgery department, the following documents and examinations are required:
- Passport, insurance policy, SNILS,
- Referral from the treating cardiologist or therapist,
- Extract from the previous place of hospitalization (department of cardiology, therapy) with the examination methods performed,
- If the patient has not been hospitalized, it is necessary to perform on an outpatient basis general clinical blood and urine tests, a biochemical blood test, determination of blood group and blood coagulation ability, ultrasound of the heart, ECG, 24-hour monitoring of ECG and blood pressure, chest x-ray, exercise tests (treadmill test, bicycle ergometry),
- You may need to consult an ENT doctor, gynecologist, urologist and dentist to exclude foci of chronic infection.
TAVI procedure
When diagnosing aortic stenosis, doctors prescribe conservative treatment, which includes taking the following medications:
- diuretics that remove excess fluid from the body, reducing the load on the heart;
- dopaminergic agents that activate muscle contractions;
- vasodilating drugs that relieve heart pain;
- antibacterial drugs prescribed for the prevention of endocarditis.
However, the most effective and gentle way to treat aortic stenosis is the TAVI procedure.
Compared to the standard open-heart valve replacement procedure, which requires a sternotomy (opening up the chest), the TAVI procedure can be performed through small punctures in the chest without the need to break the integrity of the chest bones. The surgeon, taking into account the individual characteristics of the patient, determines which approach will be most acceptable and safe for the client:
- transfemoral (catheter is inserted through the femoral artery);
- transapical (the catheter is inserted through a large artery in the chest or the apex of the left ventricle, accessed through a small incision in the chest).
Using a catheter, the disassembled replacement valve is delivered to the installation site, the new valve expands, pushes the leaves of the old valve apart and subsequently takes on the functions of regulating blood flow.
4. Lifespan of heart valves
Today, two types of heart valve implants are used in heart surgery: artificial and biological.
The first ones are durable, but their installation is associated with lifelong use of a number of drugs to eliminate the risk of blood clots. Biological valves are closest to living tissues, but wear out faster. Cardiologists are constantly working to develop and introduce into medical practice new types of valves that combine the best properties of both types - durability and maximum acceptability for the body. The service life of artificial valves is 10-15 years. Newer materials are still being studied. Widespread practice of their use in the near future will provide cardiologists with more accurate information about their service life.
Where to get treatment
collaborates with the National Medical Research Center of Cardiology, which is an expert center for aortic valve replacement in the Russian Federation with experience of more than 1000 implantations.
The clinic is equipped with the latest equipment and software of the latest generation (such as intracardiac and intravascular navigation systems), which allow achieving maximum treatment results with minimal risks of complications. The specialists of our clinic are world-class experts in the field of transcatheter treatment of the heart valve apparatus, who perform TIAC procedures both in the Russian Federation and abroad.
What are the advantages of transcatheter aortic valve implantation over open surgery?
With intravascular aortic valve replacement, there are no large incisions, which significantly reduces the duration of postoperative rehabilitation, reduces pain and eliminates the development of complications associated with inflammation (suppuration) of postoperative sutures. Other important advantages of TAVI include:
- Ability to perform surgery on patients at high surgical risk, elderly patients and patients with severe comorbidities
- Short operation time, reduced surgical trauma.
- The operation is performed under local anesthesia (in some cases under general anesthesia)
- There is no need to connect to a heart-lung machine and “turn off” the patient’s heart
- Reducing length of stay in hospital
- Low percentage of postoperative complications and rapid adaptation after discharge from hospital
About the purpose of disability and prognosis
Non-working group II is determined for a period of one year after completion of the operation to restore the myocardium. In the future, transfer to group 3 is possible.
When establishing disability, cognitive deviations (decreased mental abilities) are taken into account individually.
How long do you live with an artificial valve? The average life expectancy in this case is approximately 20 years. However, theoretically, the valve’s lifespan is much longer (up to 300 years, according to doctors).
Controversy
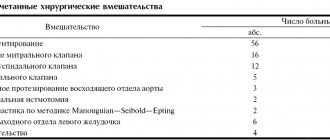
The new method spread very quickly. It was developed for patients who cannot undergo surgery due to high intraoperative risks. While the share of TAVI in 2007 was only 1.3% of all interventions for aortic valve stenosis (157 TAVI, 12,116 valve operations), in 2010 it was already 23.9% (3,629 TAVI, 11,582 valve surgeries).
Due to its rapid development, the method has become the object of criticism. The complaints boil down to the fact that this method will be used, including in those patients for whom surgery is more appropriate.
To counter this practice, university professors in the field of cardiology and cardiac surgery met in January 2011 to discuss the problem. At this Congress they defined the conditions that must be met for the effective and safe use of the new TAVI method.
Based on this, the German Heart Foundation organized an expert meeting in Frankfurt, which was attended by cardiac surgeons and cardiologists. The purpose of the meeting was to help patients receive the best therapy currently available.
Forecast
The prognosis after surgery is undoubtedly higher than without it,
since with heart defects severe heart failure develops, which not only impairs the tolerance of normal physical activity, but also leads to death. In patients after surgery, mortality is much lower, and is mainly associated with the development of thromboembolic complications (0.2% of deaths per year). Therefore, surgery to replace heart valves is an intervention that significantly prolongs the patient’s life and improves its quality.
Lifestyle
A person’s further life after surgery comes down to the following points:
- Regular visits to the doctor - monthly in the first year after surgery, every six months in the second year and annually thereafter, with constant monitoring of the functions of the cardiovascular system using ECG and echocardioscopy,
- Regularly taking prescribed medications (anticoagulants, antibiotics),
- Treatment of residual heart failure with the constant use of digoxin and diuretics (indapamide, veroshpiron, diuver, etc.),
- Adequate physical activity
- Compliance with the work and rest schedule,
- Following a diet - excluding fatty, fried, salty foods, eating large amounts of vegetables, fruits, dairy and cereal products,
- Complete elimination of bad habits.
Role of external cardiologists
The congressional document describes it as “perfectly acceptable” for outside trained cardiologists to perform heart valve implantations on their patients as visiting physicians at the center, in collaboration with the cardiac surgeons and cardiologists employed there. Responsibility and management of the intervention rests with the center’s team of internal cardiologists and cardiac surgeons.”
This controversial piece of Congress has already been discussed. In Frankfurt, experts were unanimous that it is in principle possible to perform TAVI by external cardiologists together with a cardiac surgeon and a cardiologist at the center. But the center's cardiologist must be informed about this in advance so that he can make an independent decision whether he will carry out the intervention together. However, the issue of the responsibility of external cardiologists when working together is not clear. Although the immediate responsibility for the intervention lies with the cardiologist who performs the intervention, responsibility does not end with the completion of the intervention. For example, the clinic is responsible for quality assurance. In addition, the question remains open of who is responsible in the event of complications that arise only a few days after the intervention.
Complications
The most serious complications after the introduction of a prosthesis are thromboembolic ones. Prevention of their development is lifelong antithrombotic therapy with the help of anticoagulants and antiplatelet agents - drugs that “thin” the blood. Such drugs include:
- Subcutaneous injections of heparin in the early postoperative period,
- Continuous use of warfarin under monthly monitoring of INR (international associated ratio) - an important indicator of the blood clot-forming system; normally it should be within 2.5 - 3.5,
- Constant use of aspirin (thromboAss, acecardol, aspirin Cardio, etc.).
No less dangerous consequences are the development or recurrence of infective endocarditis, the prevention of which is the rational prescription of antibiotics in the postoperative period, as well as their further use during any operations and minimally invasive interventions (tooth extraction, gynecological and urological manipulations, etc.).