ARTERIAL PRESSURE
BLOOD PRESSURE, blood pressure in the arteries. Blood pressure level is expressed in millimeters of mercury (mm Hg) and depends on the pumping force of the heart, peripheral. vascular resistance and circulating blood volume. Systolic pressure reflects max. blood pressure on the walls of the arteries during contraction of the heart, diastolic - at the moment of its relaxation and depends mainly. from peripheral vascular resistance. In humans, for example, the systolic ratio and diastolic pressure is normally 120/80, in a giraffe 340/230, in a dog 156/100, in a shark 32/16 mm Hg. Art. There are also pulse pressure (the difference between systolic and diastolic), depending on the volume of blood ejected with each contraction of the heart and the elastic properties of the aorta, and average blood pressure (equal to the sum of diastolic and 1/3 pulse pressure), proportional to the volume of blood, ejected by the heart in 1 minute, and general peripheral. resistance of the blood vessel system. In most mammals (including humans) it is 100 mm Hg. Art. Blood pressure values decrease as the vessel moves away from the heart. For example, in a healthy adult, systolic. the pressure in the aorta is 110–130 mm Hg. Art., in arterioles – 20–50 mm Hg. Art. During the day it fluctuates depending on functional activity and decreases significantly at night during sleep (70–80 mm Hg). In vessels located above the level of the heart, the pressure decreases in proportion to the size of the hydrostatic column. A giraffe, for example, needs a high blood pressure so that blood can reach the head. Max. blood pressure values in annelids and arthropods are 5–10 mm Hg. Art., for active fish (e.g. salmon, eel) – 65–75, for the green frog – approx. 40, in birds – 140–180 mm Hg. Art. Male warm-blooded animals have a higher blood pressure than females, and cold-blooded animals have a lower blood pressure than warm-blooded animals.
In vertebrates, conservation refers. The constancy of the blood pressure level is ensured by a regulatory system, due to which a certain relationship is achieved between the work of the heart, the lumen of blood vessels, the capacity of the vascular bed and the amount of circulating blood. The action is physiological. regulation mechanisms can be short-term or long-term. The former include the renin-angiotensin-aldosterone system and cardiovascular reflexes. These reflexes are mediated through the center. nervous system (the so-called baroreflex, chemoreflex, cerebroischemic reaction), maintain a normal blood pressure level from several. minutes to several minutes hours.
Baroreceptors located in the wall of the aortic arch and in the area of the branch of the common carotid artery (carotid sinus) respond to the degree of stretching of the vascular wall with an increase in blood pressure. The frequency of impulses coming from the baroreceptors to the cardiovascular center in the medulla oblongata increases, which leads to to a reflex decrease in cardiac output and peripheral resistance. vessels and, as a consequence, a decrease in blood pressure. The higher the pressure in the aortic arch and carotid sinus, the stronger the nervous influences leading to a decrease in blood pressure. When blood pressure falls, the frequency of impulses coming from the baroreceptors decreases and reflexively increases cardiac output and resistance of small arteries and arterioles and hence pressure. The baroreflex acts as a buffer, smoothing out rapid fluctuations in blood pressure, for example. with a sharp transition from a horizontal to a vertical position, no phenomena associated with impaired blood supply to the brain are felt.
The chemoreflex is triggered both from the peripheral. receptors located in the aortic and carotid reflexogenic zones, and from the center. chemoreceptors localized in the medulla oblongata. The first ones are activated first. when there is a deficiency of oxygen in the blood, the latter react to an excess of carbon dioxide in it. Activation of chemoreceptors leads to reflex activation of the sympathoadrenal system. In the end, out of cuteness. nerve endings release norepinephrine, which acts on the so-called. alpha-1 adrenergic receptors on the smooth muscles of blood vessels and causes their constriction; beta-1 adrenergic receptors mediate an increase in cardiac output. Adrenaline secreted by the adrenal glands, through the activation of beta-2 adrenergic receptors, expands the bronchi, activates glycogenolysis, which leads to an increase in blood glucose.
The cerebroischemic reaction occurs when there is a significant decrease in the blood supply to the neurons of the cardiovascular center. When means. blood loss, the average blood pressure can drop to 60–70 mm Hg. Art., which leads to a deficiency of blood supply to the cardiovascular center and direct stimulation of the sympathoadrenal system and partial normalization of blood pressure. With blood loss accompanied by a decrease in blood pressure to 40–30 mm Hg. Art., hemorrhagic shock, as a rule, becomes irreversible.
When the renin-angiotensin system is activated, the increase in blood pressure is caused by the formation of angiotensin-II (formed with the participation of renin), which causes vasoconstriction, and an increase in the secretion of aldosterone, which leads to an increase in the volume of circulating blood.
Long-term regulation of blood pressure is carried out with the participation of the kidneys, which ensure a balance between the consumption and release of sodium and water ions; even a slight increase in blood pressure is accompanied by a significant increase in fluid secretion by the kidneys. It is well-functioning kidneys that maintain the average blood pressure within the normal range throughout a person’s life.
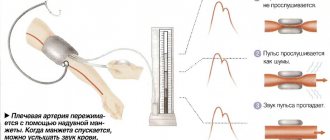
Blood pressure is most accurately measured directly using catheters inserted into blood vessels and connected to pressure sensors. A less accurate measurement method proposed by Ros. surgeon N. S. Korotkov in the beginning. 20th century, records the value of blood pressure using a tonometer - a pressure gauge connected to a rubber cuff, fastened around the arm in humans, and around a limb or tail (in rats) in animals. The air pumped into the cuff compresses the artery and the moment when the vessel stops passing blood is determined using a phonendoscope by the cessation of pulse sound vibrations. Slowly releasing air from the cuff, the moment of the sound caused by the contraction of the heart is recorded, and the systolic value is determined using the pressure gauge. pressure. The pressure gauge readings at the moment the pulse disappears correspond to the diastolic value. pressure.
In humans, blood pressure is considered elevated, at which the values of systolic. and diastolic pressures exceed 140 and 90 mm Hg, respectively. Art. A long-term increase in human blood pressure is arterial hypertension, a decrease is arterial hypotension.
Central aortic pressure and vascular stiffness: relevance in modern cardiology
The increase in cardiovascular diseases, observed in all developed countries of the world, requires close attention to the prevention and effective treatment of heart and vascular diseases.
Research data suggests that hypertension affects approximately 65 million Americans aged 18–39 years and 1 billion people worldwide. Arterial hypertension (AH) is a risk factor for the development and progression of atherosclerosis, coronary heart disease, chronic heart failure and acute cerebrovascular accidents. Changes in elastic vessels (aorta, pulmonary artery and large arteries branching from them) are an important part of the pathogenesis of hypertension. Normally, the elastic properties of these vessels, especially the aorta, help smooth out the periodic waves of blood produced by the left ventricle during systole and convert them into continuous peripheral blood flow. The elastic properties of the aorta modulate left ventricular function by reducing left ventricular afterload and end-systolic and diastolic volumes. This leads to a decrease in the tension of the walls of the left ventricle, as a result of which the trophism of the subendocardial layers of the myocardium, which are most sensitive to hypoxia, improves and coronary blood flow improves. One of the significant characteristics of elastic-type vessels is rigidity, which determines the ability of the arterial wall to resist deformation. The stiffness of the vascular wall depends on age, the severity of atherosclerotic changes, the speed and degree of age-related involution of the most important structural proteins elastin and fibulin, an age-related increase in collagen stiffness, genetically determined characteristics of elastin fibers and the level of blood pressure (BP). A number of studies have emphasized the role of inflammation in the pathogenesis of large artery stiffness. The classic marker of arterial stiffness/elasticity of large vessels is pulse wave velocity (PWV). The value of this indicator largely depends on the ratio of the thickness of the vessel wall to the radius of the vessel lumen and the elasticity of the vessel wall. The more distensible the vessel, the slower the pulse wave propagates and the faster it weakens, and vice versa - the more rigid and thick the vessel and the smaller its radius, the higher the PWV. Normally, PWV in the aorta is 4–6 m/s; in less elastic arteries of the muscular type, in particular the radial artery, it is 8–12 m/s. The gold standard for assessing aortic stiffness is the PWV between the carotid and femoral arteries.
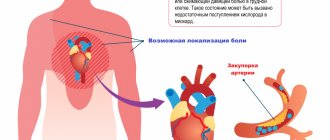
Central (aortic) and peripheral blood pressure
In a normal arterial system, after contraction of the ventricle in systole, the pulse wave is directed from the site of origin (aorta) to large medium and then small vessels at a certain speed. Along the way, the pulse wave encounters various obstacles (for example, bifurcations, resistive vessels, stenoses), leading to the appearance of reflected pulse waves directed to the aorta. With sufficient elasticity of large vessels, primarily the aorta, the reflected wave is absorbed. The sum of direct and reflected pulse waves differs in different vessels; as a result, blood pressure, primarily systolic blood pressure (SBP), differs in different main vessels and does not coincide with that measured on the shoulder. The degree of increase in SBP in the peripheral arteries relative to SBP in the aorta varies greatly between subjects and is determined by the elastic modulus of the arteries studied and the distance from the measurement site. Because of this, the cuff pressure in the brachial artery does not always correspond to the pressure in the descending aorta. A certain contribution to the increase in blood pressure in the brachial artery relative to blood pressure in the aorta is made by an increase in the rigidity of its wall, which means the need to create greater compression in the cuff. Unlike peripheral blood pressure, the level of central blood pressure is modulated by the elastic characteristics of large arteries, as well as the structural and functional state of medium-sized arteries and the microvasculature and, thus, is an indicator that indirectly reflects the state of the entire cardiovascular system. The greatest prognostic value is blood pressure in the ascending and central parts of the aorta, or central blood pressure. In the case of increased stiffness (decreased elasticity) of the aorta, the reflected wave is not absorbed sufficiently and, as a rule, due to a higher PWV, returns during systole, which leads to an increase in central SBP. The consequence of increased rigidity and increased central blood pressure is a change in afterload on the left ventricle and impaired coronary perfusion, which leads to left ventricular hypertrophy and increased myocardial oxygen demand.
In recent years, special techniques have appeared (for example, applanation tonometry of the radial or carotid arteries) that make it possible to record such determinants of pulse pressure as pulse (oscillations of the arterial wall from the heart to resistive vessels) and reflected (oscillations of the arterial wall from resistive vessels to the heart) waves, and, using computer processing when recording radial artery oscillations, calculate the values of central pressure in the aorta (Fig. 1). Within 10 seconds, the pressure curve in the radial artery of the upper limb is recorded using an applanation tonometer. The data is processed using software: the average shape of the curve is calculated, which is transformed using the accepted mathematical method into a graph of central pressure in the aorta (CPA). Computer processing of the obtained central pressure curves allows one to determine the parameters of the central pressure: the time to the first (T1) and second (T2) systolic peaks of the wave. The pressure at the first peak/kink (P1) is taken as the ejection pressure, a further increase to the second peak (ΔP) means the reflected pressure, their sum (maximum pressure during systole) is the systolic central pressure (CPAs). In addition to the value of central blood pressure, there is an indicator of pressure increase, augmentation index (amplification, AIx) expressed as a percentage, which is defined as the pressure difference between the first, early peak (caused by cardiac systole) and the second, late (appearing as a result of reflection of the first pulse wave) systolic peak, divided by the central pulse pressure. Thus, central aortic pressure is a calculated hemodynamic parameter that depends not only on cardiac output and peripheral vascular resistance, but also on the structural and functional characteristics of the main arteries (their elastic properties). Differences between central and peripheral SBP levels are most pronounced in young people and decrease in older people. Central blood pressure, especially central pulse pressure, and the augmentation index have been shown to correlate with the degree of large artery remodeling and PWV as a classic indicator of vascular wall stiffness.
Arterial stiffness as a cardiovascular risk factor
Changes in the mechanical properties of large arteries have a clear pathophysiological relationship with clinical outcomes. Research suggests that PWV, a measure of arterial stiffness, may be a better predictor of subsequent cardiovascular events than known risk factors such as age, blood pressure, hypercholesterolemia and diabetes. Studies assessing PWV have established that increased arterial stiffness is a predictor of cardiovascular risk in apparently healthy individuals, patients with diabetes mellitus, end-stage renal disease, and the elderly. It has been demonstrated that arterial stiffness is a predictor of mortality in patients with hypertension. Thus, in a population-based study of the Copenhagen County population, it was demonstrated that an increase in PWV (>12 m/s) is associated with a 50% increase in the risk of cardiovascular events. In addition, the prognostic value of PWV was found in a Japanese study with an average follow-up of 8.2 years. Indirect indices of aortic stiffness and reflected waveforms, such as central aortic pressure and augmentation index, have been found to be independent predictors of cardiovascular events and mortality. Thus, in a study that included 1272 normotensive and untreated patients with hypertension, it was demonstrated that central SBP was an independent predictor of cardiovascular mortality after adjustment for various cardiovascular risk factors, including left ventricular myocardial mass and determination of intima-media thickness. with ultrasound examination of the carotid arteries. Moreover, patients with high aortic pressure have a worse cardiovascular prognosis than patients with better control of central aortic pressure.
Increased aortic stiffness is also an independent predictor of diastolic dysfunction in patients with hypertension (Fig. 2) and may also limit exercise capacity in dilated cardiomyopathy. In patients with heart failure with preserved left ventricular ejection fraction, systolic dysfunction and arterial stiffness appear with age and/or progression of hypertension. Increased arterial stiffness is associated with endothelial dysfunction and decreased nitric oxide (NO) bioavailability. Endothelial dysfunction in patients at high cardiovascular risk may explain why these conditions are associated with increased arterial stiffness in the early stages before the onset of atheroma. Therefore, drugs such as nebivolol that increase NO production may reduce large artery stiffness, which in turn may lead to a reduction in cardiovascular risk. Thus, the importance of arterial stiffness, assessed by PWV, for the risk of cardiovascular outcomes has been demonstrated in a number of prospective studies both in patients with hypertension and in the general population. Since 2007, assessment of PWV on the carotid-femoral segment has been recommended as an additional research method for identifying target organ damage in hypertension.
Authors
A.N. Belovol, Doctor of Medical Sciences, Professor, Corresponding Member of the National Academy of Medical Sciences of Ukraine;
I.I. Kknyazkova, Doctor of Medical Sciences, Associate Professor
Kharkov National Medical University
Article provided by the WEB site “Country of Doctors”