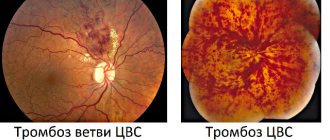
Signs of occlusion
The main signs of central occlusion are:
- muscular;
- articular;
- dental
In the latter case, it is necessary to determine what the surface contact will be and whether it is complete. It is necessary to determine how exactly the opposite rows are brought together, if there are any violations, what kind of overlap is for the top row. Also, when determining occlusion, the specialist looks at whether the upper molar comes into full contact with the lower molar, whether there is a coincidence or displacement.
Signs of prognathic occlusion (2)
Malocclusion is characterized by changes in the way the teeth fit together, but additional external signs may also be present. All manifestations of distal occlusion can be divided into 3 groups:
- 1. Intraoral : protruding front teeth, the presence of a distance between the incisors of the upper and lower rows when closing.
- 2. Functional : discomfort when swallowing and chewing, impaired diction, difficulty in nasal breathing. At the same time, an adult who has suffered from the problem since childhood will most likely adapt and will not feel such inconveniences.
- 3. External : protrusion of the nose and upper lip, but sinking of the lower lip, reduction of the chin, in advanced cases the mouth is constantly slightly open. A distal bite can also affect posture: there is a stoop, the body is tilted forward, and the stomach protrudes.
If signs of distal occlusion are detected in a child or adult, you should contact the doctors at Leonid Gorbunov’s orthodontic studio for comprehensive diagnosis and treatment.
Signs of correct contact
General signs of correct contact are:
- convergence in the vertical plane;
- molars and incisors in both rows have antagonists;
- the upper eighth teeth do not have antagonists;
- the lower central incisors do not have antagonists.
Signs that apply only to the front teeth:
- if the face is conventionally divided by a central line, then the central axis of symmetry should pass between the front teeth;
- the overlap of the upper row of the lower row can be up to 30% in height of the crown size;
- The cutting edges of the lower teeth are in close contact with the cusps of the upper teeth.
Signs that apply only to lateral teeth:
- the distal buccal cusps of the upper row are located between the 6th and 7th lower molars;
- the lateral elements of the lower and upper rows close so that they fall into the intertubercular grooves.
Reasons for development
The causes of distal occlusion can be correctable or non-correctable . In the first case, the development of the anomaly can be prevented if risk factors are eliminated. In the second case, it is impossible to influence the causes. In most cases, prognathic occlusion develops due to a combination of different risk factors, which include:
- 1. Genetic changes . In more than half of clinical cases, genetic predisposition plays a decisive role in the development of the anomaly. And exposure to other risk factors only aggravates the situation.
- 2. Disturbance of intrauterine development of the fetus . Any problems with the mother’s health, exposure to unfavorable external factors can lead to the fact that the newborn already has developmental anomalies, in particular problems with bite.
- 3. Incorrect breastfeeding, thumb sucking . Using bottles with openings that are too wide or not properly latching on to the breast leads to the fact that the lower jaw does not develop enough. Bad habits can aggravate the situation: sucking pacifiers, fingers or other objects.
- 4. Carious lesions or untimely loss of baby teeth . Both problems negatively affect the formation of a correct bite and jaw development.
- 5. Childhood diseases . General diseases of the child can also affect the growth of the jaws and the position of the teeth: problems with the respiratory system, systemic autoimmune diseases, rickets, deficiency of nutrients.
Development of distal occlusion in children as a result of thumb sucking:
It is not always possible to avoid the formation of a distal bite, even if you try to eliminate all of the listed risk factors. If a problem is detected, it needs to be corrected as soon as possible.
Basic methods
Central occlusion is determined at the stage of prosthesis production, which is necessary for the normal functioning of the structure and the effectiveness of treatment. When determining occlusion, various options are used:
- The presence of antagonists on both sides. This method is used if there are antagonists on both sides, but the height of the lower third of the face remains fixed. The occlusion indicator is based on the number of contact zones; during examination, specialized templates are used, which makes this option the simplest.
- Presence of 3 occlusal points. This method is used if there are three contact zones, while the natural height of the face is disrupted. When determining, special rollers are used that are placed on the bottom row. The patient clenches his jaws, resulting in an imprint of teeth on the ridge. This imprint is used in the laboratory during the manufacture of prosthetics.
- There are no antagonistic pairs. This is the most labor-intensive method, which is used in the complete absence of antagonists on both sides. The method includes the formation of a prosthetic plane, determination of the normal height for the lower third of the face, and fixation of the mesiodistal relationship for the lower and upper jaws.
The test is carried out by closing the teeth and includes the following simple steps:
- a thin strip of wax is placed on the surface of the roller and glued to it;
- the structure heats until the wax softens;
- special heated templates are carefully placed in the patient’s oral cavity;
- The teeth are brought together, after which a clear imprint remains on the wax.
| Click to sign up for a FREE consultation |
Based on the test results, the specialist calculates the height of the bite at rest and with the jaws fully brought together. Techniques for correct positioning of the lower jaw can be different. These are not only functional, but also instrumental methods of correction. But such work is very difficult, it completely depends on the experience and qualifications of the specialist. If violations were made during the inspection, this can lead to the following problems: overbite or underbite, the appearance of permanent occlusion (anterior or lateral). The causes of errors may be improper preparation of the templates, insufficient softening of the wax, too much pressure on the rollers when closing, errors on the part of the person performing the inspection or the technician.
Errors in the treatment of mesial occlusion
All mistakes are made due to incorrect treatment planning.
Most often this is expressed in a discrepancy between the level of treatment and the level of the cause of mesial occlusion. For example, if the upper jaw is to blame, the lower jaw is operated on. Or the jaws are to blame (the problem is skeletal), and they are trying to solve the problem “on the teeth” (only with braces). Incorrect determination of the level of the problem occurs when diagnostics are insufficient in scope or incorrect interpretation of diagnostic data. Those. when they try to treat mesial occlusion only on the basis of external signs (essentially “by eye”). Without considering the real reason.
Attempting to control the growth of the lower jaw using a sling.
A very common mistake in the treatment of mesial occlusion in children is an attempt to restrain the growth of the lower jaw using a special sling.
Many people try, but no one has managed to “contain” anything yet. Because you can’t go against nature. She (nature) will still take her course. As much as is genetically determined, so much will grow. But you can easily get complications when using such a sling.
Treatment in installments
The Orto-Artel clinic offers installments for the entire process of treating any disease. Personal conditions are considered on an individual basis.
Find out more
or call 8 (495) 128-11-74
Upcoming events
2021-09-01BASIC COURSE ON DENTAL IMPLANTATION WITH DR. FRIEDMAN FOR STUDENTS AND RESIDENTS (Annual course)
2022-01-01Forum of managers and doctors of dental clinics
2022-02-05International Implantology Congress
Rice. 7.The force vector is oriented in the orthograde (natural, physiological) direction along the axis of the implants. It should be noted that the central fossa (Fossa) of the lower molar is additionally shifted in the lingual direction, i.e., lingualized.
Determination of the central relationship of the jaws
At this stage, you cannot simply tell the patient, close your mouth correctly. Even my grandmother often complained that these words were confusing: “And you don’t know how to shut your mouth. It seems that no matter how you close it, everything is right.”
To close the mouth “correctly,” the doctor places his index fingers on the bite ridges in the area of the chewing teeth of the lower jaw and at the same time pushes the corners of the mouth apart. Next, he asks the patient to touch the posterior edge of the hard palate with his tongue (It is better to make a wax button in this place - not all patients know where the posterior edge of the hard palate is.) and swallow the saliva. The doctor removes his fingers from the chewing surface of the roller, but continues to move the corners of the mouth apart. When swallowing saliva, the patient will close his mouth “correctly.” They repeat this several times until the doctor is absolutely sure that this is the correct central ratio.
11) Next stage. The doctor fixes the rollers in a central ratio.
“Reduced” occlusion according to Gerber® (reduzierte Okklusion)
To eliminate the effects of destabilizing forces in complete removable prosthetics, the principle of reducing the surface of occlusal contacts in the area of the buccal tubercles has been used for 50 years (“reduced” occlusion according to Gerber®, Gerber A., 1960, 1965,1973). Due to this, the point of application of the load shifts in the lingual direction and the force vector is directed almost vertically (Fig. 4a, 4b).
Rice. 4a. When the buccal cusps are separated by approximately 2 mm, the chewing force acts in the lingual direction (indirectly, through the bolus). The effect of force in the buccal direction is significantly reduced.
Rice. 4b. Molars in occlusion, lateral view. Set of teeth for working according to the Gerber® method.
The less contact between the buccal cusps (contact opening), the greater the effect of stabilizing the occlusion. In complete removable prosthetics according to the concept of “reduced” occlusion, the separation of the buccal tubercles should be at least 2 mm. With a very favorable ratio of alveolar ridges, sufficient salivation and viscous saliva, contacts between the buccal cusps are allowed so that the denture on the upper jaw does not tip over (carry out a test using cotton rolls).
Malocclusion: what is the problem?
Is this really possible? Most people think so. We have to disappoint you, but this is true. After all, a correct bite is necessary not only for a beautiful smile and correct pronunciation, but also for the normal functioning of the TMJ (temporomandibular joints), the digestive tract, and the muscular system of the head and neck. Due to an incorrect bite, food is poorly chewed, which does not have the best effect on the functioning of the digestive system. An incorrect bite leads to constant tension in the muscles and joints, hence headaches, pain in the temporal joints, and cervical spine. By the way, an incorrect bite can cause aesthetic problems, for example, an unattractive profile.
Diagnosis of distal bite
Only a professional orthodontist can accurately determine the presence of distal occlusion. First, the doctor examines the oral cavity and can first judge what malocclusion the patient has. However, to confirm the diagnosis and draw up a further treatment plan, additional studies are carried out:
- 1. Computed tomography . Obtaining three-dimensional images of the dentofacial apparatus allows you to determine: the size of the jaws, their relationship, bone structure, the condition of the TMJ, and so on.
- 2. Casts . Taking impressions of the dentition allows you to determine the characteristics of the closure of the teeth. The study helps create a plan for further tooth movement to form a correct bite.
- 3. Photo protocol . Photos are taken with the mouth open and closed, in front and in profile, with a smile and from different angles. This allows you to track the dynamics of bite correction.
Contact our clinic, where diagnostics are performed using modern, precise equipment with a guarantee of reliable results.
Yesterday Today Tomorrow
Orthognathic occlusion
Orthognathic occlusion is characterized by A, B and C contacts (“A” between the buccal cusps, “B” - between the buccal and palatal cusps, “C” - between the palatal and lingual cusps, translator’s note). This is how nature works, although in many cases there are deviations from the classical picture. During the chewing process, the resulting vector of forces in the upper jaw is oriented upward and slightly in the buccal direction. However, in the manufacture of implant-supported prosthetic work, and in particular complete removable dentures, this direction of force influence negatively affects the statics of the prosthesis (Fig. 2a).
In Fig. Figure 2b analyzes the direction of force vectors on various internal slopes of the cusps (facets) of the mandibular molar on the left. It can be seen that only on one internal slope of the tubercle (facet) the force acts in the oral direction and upward (green line). In the area of the other two facets, the force acts in the buccal direction (red lines). This results in destabilizing torques in the area of the buccal cusps, causing the prosthesis to tip over.
Rice. 2a. With unilateral loading on the left side, the prosthesis on the right side is reset.
Rice. 2b. Upper molar: lines indicate the direction of forces in the area of each internal slope of the cusp (facet). The blue line marks the resulting vector of forces. It is directed outward from the alveolar ridge and this leads to the shedding of the prosthesis.
Rice. 2c. Molars in occlusion, contacts A, B, C according to Gysi. Standard modern set of artificial teeth (side view).
Features of prosthetics on implants
The greater the distance from the supporting structure (alveolar ridge) to the occlusal surface of the tooth, the more outward in relation to the supporting structure the action of the chewing force is directed. When using prosthetics on implants, the lever arm is larger, and, accordingly, the torsion (torque) force acting in the area of connection between the implant and the superstructure is greater (Fig. 3).
Rice. 3. For contacts in the area of the buccal cusps, the force acts in the buccal direction. This causes the screws on the implants to loosen or break.
List of sources
- Matyushenko A.A. “Pulmonary embolism as a general medical problem”, article in the journal RMZh No. 13 dated 07/03/1999
- Atayan A.A., Kosenkov A.N., Kuznetsov M.R., Chernookov A.I., Ivanova M.I., Khachatryan E.O. “Hybrid tactics in the treatment of acute disorders of mesenteric circulation”, RMZh No. 8(II) dated 10.25.2019
- Yavelov I.S. “The use of anticoagulants during thrombolytic therapy in patients with signs of acute occlusion of the coronary artery: how to individualize treatment?”, RMZh No. 26 of November 30, 2011
Anatomical description of the disease
Occlusion of the carotid (carotid) arteries is a partial narrowing or complete occlusion of the large canals supplying the brain. There are episodes of asymptomatic progression, often accompanied by systematic oxygen deprivation of brain areas and arterial strokes. According to medical statistics, ischemia is most often caused by damage to the extracranial parts of the circulatory system. Intracerebral degeneration of vascular tracts is detected four times less frequently. Blockage of the carotid ducts is the cause of ischemic disease of the central nervous system in 56% of cases. A third of all recorded impacts occur as a result of the closure of these channels.
The narrowing of the bloodstream may be partial, then a diagnosis of stenosis is made. When the vessel is completely blocked, a stroke occurs, and sometimes the disease causes sudden death.
Fundamentals of occlusion and biomechanics of the jaws: a new look at old concepts
A deep understanding of the basics of occlusion and biomechanics of the jaws is one of the most important and necessary components for providing comprehensive patient rehabilitation in dental practice. Knowledge of the principles of differential diagnosis of pain, planning of future iatrogenic intervention, as well as algorithms for the treatment of prosthetic disorders provides the doctor with all the necessary tools for further normalization of the patient’s dental status.
An orthopedic doctor simply cannot do without understanding how significant the concept of occlusion is not only in pathology, but also in a state of stable and adequate function. The formation of appropriate occlusal schemes is based on the redistribution of acting forces, because, in fact, it is precisely because of the excess of such indicators that diseases, pathologies and dysfunctions of the elements of the dentofacial apparatus arise.
Occlusal disorders can manifest themselves in the form of various structural damage to the dental status, such as pathological abrasion, fractures, and premature wear of restorative structures. In addition to the latter, functional pathologies are characterized by tooth mobility, loss of volume of soft and hard tissues, muscle pain, as well as pain and noise in the joints (the so-called clattering), limitation and impairment of movements of the lower jaw, remodeling changes in bone tissue in the structure of the temporomandibular joint . In such cases, patients form so-called parafunctional habits, the presence of which he himself does not know. Clinically, signs of such are manifested by excessive wear of one’s own teeth and various types of restorative structures present in the oral cavity.
There are different opinions regarding the relationship between the state of occlusion and disorders of the temporomandibular composition. According to the most extensive literature reviews, such associations are rather weakly expressed, as evidenced by the fact that when correcting occlusal relationships, it is not always possible to prevent the development and progression of joint pathologies. Based on the available data, the following conclusions can be drawn: only the absence of traumatic occlusal injuries, which are manifested by the action of excessively high parafunctional forces exceeding the adaptive capabilities of the body, ensures complete prevention of the occurrence of pathologies and dysfunctions, or the presence of such in the acceptable adaptation range. This conclusion is evidence-based, regardless of how ideal or non-ideal the occlusal schemes of each individual patient are. On the other hand, with prolonged exposure to excessive occlusal forces, the development of corresponding dysfunctions and diseases occurs regardless of the characteristics of a particular occlusal scheme. The corresponding pathological types of occlusion only further aggravate the course of related prosthetic diseases.
From the above it follows that if the doctor is fully familiar with the specifics of occlusal movements in a particular patient, and also understands their impact on the condition of soft and hard tissues, muscles and joints, then he can ensure the formation of such occlusal patterns that would be the most stable and least traumatic for each specific patient. In other words, understanding the basics of occlusion helps doctors not only plan future interventions, but also predict the functional rehabilitation of prosthetically compromised patients. The main connecting link between the pathology of the temporomandibular joint, the state of occlusion and the functional disorder of the dentofacial apparatus is the repeated action of excessive occlusal load, which goes beyond the adaptive range of the body. Based on this, the author considers it wrong to separate the dynamics of the application of force on human tissue from disorders and diseases developing in the same tissues - after all, in fact, these processes are of an indirect cause-and-effect nature.
The question is different: what is the true connection between the existing parafunction, the state of occlusion and functional deviations of the dentofacial apparatus. In order to understand how the jaw functions and where occlusion begins, you need to repeat in detail the anatomy of the masticatory muscles, the temporomandibular joint, and, of course, the teeth, taking into account the functional parameters of each of the above-mentioned components. After analyzing the anatomy, you should focus on how the relationship between the upper and lower jaws is generally formed, taking into account the occurrence of static and dynamic contacts between the surfaces of antagonist teeth. After this, the data obtained during the analysis can be implemented into a plan for future iatrogenic intervention aimed at eliminating structural disorders of the dentition and aesthetic problems, while ensuring not only the functional comfort of the dentofacial apparatus, but also the stability of the achieved results of complex rehabilitation.
In the course of analyzing the features of anatomy and intermaxillary relationships, doctors should look for key parameters of each of these components, on the basis of which they will subsequently make a decision regarding one or another possible treatment plan.
In this article, the author will refer to the concept of dental treatment planning, which takes into account changes in the facial profile during iatrogenic interventions, developed by Frank Spear. With significant destruction of the tooth structure, the main occlusal landmarks are simply lost, and the pathology goes beyond the boundaries of possible dental-alveolar compensation. Consequently, the clinician’s task is also to restore the supporting occlusal points of the intermaxillary relationship, and then, based on their stability, carry out further prosthetic rehabilitation. When implementing an approach to treatment taking into account changes in the facial profile, it is possible to ensure successful prosthetic reconstruction of the bite, based precisely on the position of the supporting occlusal landmarks.
Pankey rules and the concept of optimal occlusion
Dr. LD Pankey, being a pioneer and developer of comprehensive approaches to dentition restoration, proposed a specific concept that helps critically evaluate occlusion both during systemic dental rehabilitation and during everyday dental care:
- When the condyle of the jaw is completely in the glenoid fossa, all the posterior teeth exhibit equal and uniform contact, while the anterior teeth only lightly touch the opposing teeth.
- When the jaws are clenched, neither the teeth nor the lower jaw move.
- When the mandible moves in any direction, none of the back teeth contact faster or more strongly than the teeth in the anterior region.
Having analyzed these features, we can take a fresh look at the specifics of the anatomy of the dentofacial apparatus.
Anatomy of the temporomandibular joint
In Photo 1 you can see that the condyle of the mandible is in very close contact with the biconcave disc of the joint. These elements of the joint are located inside the capsule, which is protected behind by retrodiscal ligaments, and below, by means of capsular ligaments, is attached to the neck of the condylar process. Anteriorly, the superior portion of the lateral pterygoid muscle attaches to both the disc and the neck of the condylar process, while the inferior portion of the muscle attaches only to the neck of the condyle. Behind the joint is the external auditory canal. Anterior and superior to the condyle is the eminence, and directly above it is the glenoid fossa. The articular surfaces are covered by fibrocartilage, which is a smooth structure, and is supported by synovial fluid. The latter lubricates the surfaces of the joint, providing them with nutrients and oxygen, as well as ensuring the removal of possible debris. In the structure of the capsule, the number of blood tissues is very limited, or they may be completely absent.
Photo 1. Classic diagram of the anatomy of the temporomandibular joint.
When analyzing a joint, it is necessary to note the most important relationships of its individual components. First, there is the close condyle/disc/fossa connection. Essentially, they are in as much contact as possible, allowing the joint to withstand the necessary loads. On the other hand, this form of connection of the elements ensures the anatomical and functional integrity of this organ during dynamic movements of the lower jaw. In certain articular pathologies, this relationship is disrupted, which leads to permanent functional changes. It is obvious that the variation in the size, volume and shape of the temporomandibular joint is quite significant, and these differ greatly from person to person. Historically, we have assumed that the dimensions of the condylar process are relatively stable. However, recent research has established that the size of this anatomical structure can change and adapt over time and depending on the prevailing circumstances. A striking example is the increase in condyle size when using night guards. Due to the protrusion of the mandible to maintain patency of the upper airway, the condyle also remodels, increasing in size. Thus, it is obvious that this bone structure can not only adapt to functional conditions, but also change its shape, increasing in its geometric parameters. Consequently, the previously determined dimensional stability is very, very relative. As the first occlusal guideline, the doctor can use the position of the condyle during the registration of the centric relation, which is the most desirable. Firstly, the central ratio is a parameter that, with adequate execution technique, can be quite accurately and easily recorded. In addition, this position of the structures is repeatable, and it can be restored even if the position of the teeth changes or the contact between them is disrupted. A stable joint in this position has the ability to withstand significant loads, and the lateral pterygoid muscle can remain in a passive state even with strong clenching of the jaws (photo 2, 3).
Photo 2. Muscles that lift the mandible on the right side.
Photo 3. Muscles that lift the mandible on the left side.
Anatomy of the masticatory muscles
The function of raising the lower jaw is provided by three masticatory muscles. With parafunctional habits, such as bruxism, these masticatory muscles can develop significant force acting on all structures of the dentofacial apparatus. The masticatory muscle starts from the zygomatic arch and is attached to the lower edge of the lower jaw. The force vector of this muscle is directed upward and forward. The cross-sectional thickness of the masticatory muscles justifies the fact why they can develop the most significant strength indicators, located anterior to the temporomandibular joint. The temporalis muscle begins in the area of the temporal fossa and the deep part of the temporalis fascia. It is directed medial to the zygomatic bone and forms a tendon that is attached to the coronoid process of the mandible, and also passes into the region of the retromolar fossa distal to the last molar of the mandible. Since the muscle splits along its course, the action vectors of its force also diverge: the anterior component is directed upward and slightly anteriorly, while the posterior component is directed upward and posteriorly. This feature should be taken into account when diagnosing pain symptoms arising in the area of this particular muscle.
The medial pterygoid muscle consists of two heads: the main part of the muscle begins directly above the medial surface of the lateral pterygoid plate, while the superficial head begins from the maxillary tubercle and the pyramidal process of the palatine bone. The fibers of this muscle are directed downward laterally and posteriorly, and through the tendon are woven into the lower and posterior parts of the medial surface of the angle and ramus of the mandible. Insertable fibers connect this muscle with the masseter, forming common tendon slings, which allows both muscles to jointly perform the function of raising the mandible.
All of the above anatomical factors determine the direction vector of forces when activating the above-mentioned muscles. First, the directions of force of all three muscles shape the position of the condyle in the glenoid fossa: anteriorly and superiorly opposite the eminence and slightly medially, so that the medial pole of the condyle is the most load-bearing side of the joint. In other words, if we exclude the action of interdental contacts, then it is these muscles that determine the most superior position of the condyle, thereby ensuring close contact between the condyle, disc and glenoid fossa. The digastric muscle is one of the main muscles that lowers the lower jaw and opens the mouth. It begins in the area of the mastoid notch, forms a tendon along its path, and ends at the lower border of the mandible near the symphysis on the side of the digastric fossa. Since this muscle lowers the jaw, pain in this area is a rather unusual symptom. The lateral pterygoid muscle moves the lower jaw laterally and also forward. The upper head of this muscle starts from the infratemporal wing of the sphenoid bone, and the lower head starts from the lateral pterygoid plate. The muscle is woven in two bundles into the neck of the condylar process and the articular disc. Part of its function is to coordinate the position of the disc relative to the condyle to maintain the desired functional relationship, but in addition it provides support for the mandible in an eccentric position during intense clenching or bruxing when appropriate jaw movement is required to achieve maximum intercuspidation at existing tooth contacts . The three main levator muscles produce much more force than the lateral pterygoid muscle, therefore it must provide sufficient contraction to counteract the aforementioned elevator muscles. If these parameters do not correspond, painful sensations and even spasms may occur, which indicate a violation of muscle function.
Posterior teeth relationship
Pankey's first rule states that by positioning both condyles in centric relation, the posterior teeth form simultaneous and uniform contact, while the anterior teeth contact either slightly less or to a similar degree (Plates 4, 5).
Photo 4. Teeth contacts on the upper jaw.
Photo 5. Teeth contacts on the lower jaw.
Essentially, every type of occlusal design, regardless of condylar position, involves achieving multiple tooth contacts. With this ratio, the bite force is distributed more evenly over a larger number of tooth surfaces. In addition, maximal contact does not require activation of the lateral pterygoid muscles to maintain the mandible in the desired eccentric position. On the other hand, by ensuring simultaneous contact of the tooth cusps with flat bite pads, it is possible to guarantee the direction of the acting force down the long axis of the teeth, excluding the influence of deflecting lateral components (photo 6).
Photo 6. Areas of contact between the cusps.
It is the latter that provoke various structural damage to teeth, restorations, soft tissues and bone crest. And finally, with adequate contact of the posterior teeth, optimal distribution of the functional forces of the muscles that lift the mandible is ensured on both temporomandibular joints. When contact is ensured only in the area of the incisors, 60% of the total force generated by the muscles that lift the mandible is transferred to both joints, while with contact of the second molars this figure decreases to 5%. Posterior tooth contact is especially critical for painful and unstable joints.
Functional system assessment
Assessment of the functional system is a stage of diagnosing all conditions of the functioning of the dentofacial apparatus in each individual patient. The beginning of this stage is an analysis of how the patient talks to the doctor, and the idea of this approach was first proposed by Bob Barkley and later improved by Pankey. Barkley came to the conclusion that it is best when any disorders in a patient are diagnosed not only by the treating team of doctors, but also by the patient himself during diagnostic procedures. Therefore, a history review is a key initial aspect of treatment. A thorough and comprehensive patient examination algorithm was precisely described by William Lockard in his book “The Exceptional Dental Practice”.
Assessment of the functional state of the dental system includes diagnostics:
- temporomandibular joints
- masticatory muscles
- range and pattern of movements of the lower jaw
- analysis of static and dynamic tooth contacts.
The overall goal of a functional examination is to collect as much data as possible in order to determine whether the patient’s dental condition is stable or not. If the system is unstable, the doctor needs to determine where the structural damage occurred, what pathology could provoke it, and what type of dysfunction arose as a result. It is extremely important to consider all possible influencing factors before making a final diagnosis. Sometimes it happens that certain violations of functional parameters can be identified only at the end of the diagnostic process, or even between patient visits, based on his own complaints and comments that arose during a comprehensive examination. The order of diagnostic manipulations is determined by the attending physician himself, therefore the author developed the algorithm presented in the article himself, based on existing clinical experience. The first stage of diagnosis remains the assessment of joint function.
This step involves obtaining answers to the following questions:
- Do you feel pain when palpating your joints? If so, what is the nature of these sensations and how strong are they?
- Do you feel noises when moving your joints? If so, at what point in the movement and what is the nature of the sound? Is it painful?
- Is the movement of the lower jaw free and unrestricted? Are there any deviations? If so, how significant are they and in what direction are they observed?
- Can the joints withstand the forces or loads placed on them?
Positioning at the 12 o'clock position allows the doctor to examine the patient along the long axis of the head and at the same time analyze the existing deviations in movements and symmetrical relationships. In adult patients, full mouth opening exceeds 40 mm, and in some patients this parameter even goes beyond 50 mm. The lateral movement of the lower jaw is normally about 10 mm. In this case, the doctor must determine whether pain occurs during lateral movements? Do the ranges of lateral motion differ in any particular direction? The nature of the movements of the lower jaw is determined simultaneously by the state of the condylar process, disc, articular fossa and tubercle, as well as the stability of the lateral pterygoid muscles and the muscles that provide mouth opening. It is logical that movements in a damaged or unstable joint will be more limited than movements in a healthy state of the dental system. Therefore, assessment of the initial parameters of movements in the joint is a mandatory stage of a complex diagnostic algorithm. In addition, it is very important to record the position of the joint in the centric relation position. The author uses the bimanual centric relation technique developed by Dawson, as well as a leaf calibrator, a luchiu jig, and various types of frontal stoppers. The lack of contact in the area of the posterior teeth allows the muscles that elevate the mandible to position the condylar head more highly before the disc-fossa complex of the joint limits its position. The use of front stoppers is a fairly reliable method for recording centric relation. The patient is asked to stick the lower jaw forward and repeat this several times in the position of the frontal stopper - in this way it is possible to achieve activation of the muscles that understand the lower jaw. Initial attempts to determine the centric relation may be unsuccessful due to disc impairment, or fluid swelling within the joint capsule, not to mention possible spasms of the lateral pterygoid muscles. In such cases, the doctor will be able to determine only a preliminary central ratio. As the joints and muscles stabilize, more accurate centric relation parameters can be determined. Using the same three recording methods above, the doctor can also test the ability of the joints to tolerate force applied to them. In other words, the physician can determine whether the present condyle/disc/fossa condition is stable and healthy enough to withstand the forces of normal functional loading or even parafunctional conditions? In most cases, joint instability is caused by disorders such as inflammation, disc lesions, disturbances between the constituent surfaces, and pain in the area of attachment of the lateral pterygoid muscle to the condyle and disc. By repeated protrusive and retrusive movements of the patient using a sheet calibrator and a Lucia Jig, the condition of the joint and the lateral pterygoid muscle can be diagnosed. Adaptation to stress is tested using a bimanual technique, increasing the upward pressure force. After diagnosing the joint, they begin to evaluate muscle function. This part of the inspection is to determine the following:
- condition of the three muscles that lift the mandible. Is there any discomfort during palpation? What is the approximate cross-sectional thickness of the muscle? What level of tension is present when they are active? How does the patient react to palpation performed by the doctor?
- condition of the lateral pterygoid muscles. Does pain occur with palpation or the action of any other factor?
- condition of the muscles of the floor of the mouth.
- condition of the muscles in the neck and shoulders.
Palpation of each of these muscles is slightly different, but the doctor should palpate as many of them as possible. The physician should increase the pressure gently and slowly while observing the patient's response while rating their pain response on a scale of 1-2-3 (mild to moderate to severe). In addition, the clinician should analyze the relative cross-sectional thickness of the masseter and temporalis muscles, as this parameter is a reliable indicator of the patient's ability to generate loads of a certain force during jaw clenching or towing. Based on existing observations, it is known that patients with a shallower mandibular angle tend to have thicker masticatory muscles, which in turn allows them to generate more force during function.
And finally, the doctor needs to determine the nature of tooth contacts at different jaw ratios for a final understanding of the patient’s functional state. First, the first contact at centric relation must be determined, which will be considered the critical cutoff point, even if the patient has not reached the stage of restoration of centric relation. For this manipulation, the author uses a bimanual technique and a sheet calibrator. In addition, for the same purpose, you can use the “luchiu jig”, deprogramming the patient’s masticatory muscles, and then proceed to the bimanual technique with a progressive increase in the thickness of the calibrator sheets: this is how it is possible to evaluate the upper movement of the condyle deep into the articular fossa, and as a result, the area of occurrence of the most early contact in the dental area. This manipulation helps the clinician form an idea of the need to correct the corresponding vertical and horizontal components in order to achieve maximum contact between the antagonist teeth. To perform such a correction, it may be necessary to use various treatment methods, while at the same time it is necessary to evaluate whether such an intervention will be so effective as to compensate for all the changes in the dentofacial apparatus expected during its implementation, or whether performing it as a whole will be considered inappropriate.
conclusions
Understanding the anatomy of the joints, muscles and dentition, as well as their relationship, helps the doctor to objectively assess the parameters of the bite and the function of the dentofacial apparatus. This knowledge determines the adequacy of the choice of one or another treatment approach, based on the specific clinical conditions of each individual patient. Determining the forces generated during function and parafunctional states is a key step in diagnosing and solving the main clinical problems associated with occlusion and its constituent components. The following article will examine the features of the relationship of the anterior teeth and the dynamics of the movement of the lower jaw in case of malocclusion and various dysfunctions, including pathological abrasion of teeth. In addition, the concepts of treatment planning based on changes in the patient’s appearance remain promising in the structure of algorithms for restoring articulatory patterns, while helping to reduce the destructive influence of excessive forces on the state of the entire functional system.
Posted by Edwin A. McDonald III, DDS