Publication date: September 9, 2019
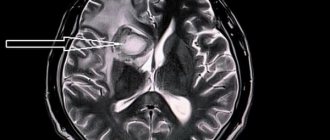
Stroke is a lesion of the central nervous system that develops as a result of a significant disruption of cerebral circulation. There are 2 types of strokes – ischemic and hemorrhagic. Ischemia is caused by blockage or prolonged spasm of the cerebral arteries. The hemorrhagic form is a consequence of hemorrhage due to rupture of a vessel. Ischemic stroke can develop gradually, while hemorrhagic stroke is characterized by a sharp increase in symptoms. Common causes of pathology are atherosclerotic changes in blood vessels and a significant increase in pressure (in particular, with hypertension). Recovery after a stroke on the left side is recommended to take place in specialized rehabilitation centers under the supervision of experienced specialists.
Why does left-sided paralysis occur?
The brain is the central organ of the nervous system.
It consists of certain zones, each of which is responsible for individual body functions.
When any of these areas are affected, characteristic symptoms appear.
In the development of pathology, the principle of so-called reverse symmetry , i.e. when the right hemisphere of the brain is damaged, paresis of the left side of the body develops.
The right side of the hemisphere is responsible for creativity and the emotional component. When a stroke develops in the right hemisphere, symptoms such as impaired speech or the inability to express thoughts clearly appear, so identifying such a condition is much more difficult.
As practice shows, circulatory disorders in the right side of the brain, in which the left side of the body is paralyzed, occurs in 57% of diagnosed cases.
Important! The main cause of paralysis of the left side of the body is a violation of blood circulation in the right hemisphere of the brain. Parts of the brain cease to be nourished, as a result of which the central nervous system is affected.
Signs of a stroke
Symptoms of a stroke, in which it is vital to immediately call an ambulance, are:
- sudden weakness and/or numbness of the muscles of the face and/or limbs - usually on one side of the body;
- difficulty speaking;
- a sharp decrease in vision (in one or both eyes);
- throbbing headache, dizziness;
- causeless loss of coordination of movements.
It is important to remember: the more quickly medical care is provided for a stroke, the higher the chances of keeping as many brain neurons alive as possible, and often the patient’s life. The most effective time for emergency treatment is 3-6 hours from the first manifestation of the disease. After this period, changes in the affected areas of the brain may become irreversible, and rehabilitation measures after a stroke may become virtually useless.
Symptoms
The following symptoms can help identify a right-sided stroke:
- the occurrence of headaches and a feeling of numbness in the left side of the body;
- paralysis of the left upper or lower limb. In this regard, when the patient tries to stretch both arms forward, a situation is observed where the left hand lags behind the right;
- patient complaints of dizziness, nausea and weakness;
- left-sided facial paralysis ;
- increased heart rate and pulse;
- decreased visual and hearing ability on the left side;
- the patient’s ability to independently rely exclusively on the right leg;
- impaired logical thinking;
- spasms ;
- at some point, a patient with right hemisphere damage may be found unconscious ;
- with this condition, patients report disturbed sleep, a state of exhaustion and a poor emotional state.
In a situation where a stroke has developed in an elderly patient, a coma is likely to occur, which will last no more than a day. If a person does not regain consciousness within the specified time, then the likelihood of acquiring disability increases at a tremendous rate every day.
Consequences of paralysis
Patients who have suffered a right-sided stroke lose balance , as well as measure and sense of tact.
In addition, a person who has suffered a stroke risks remaining disabled for the rest of his life.
With a right-sided stroke, the consequences can be very severe due to the death of brain cells.
In this case, the functioning of almost the entire body is disrupted .
The affected hemisphere of the brain subsequently does not function at full capacity. When blood circulation is impaired, a feeling of numbness occurs in the fingers. As a result, the patient is unable to hold objects, such as a pen or spoon, in his left hand. The process of tying shoelaces and fastening buttons becomes problematic.
Against the background of a hemorrhagic stroke, the right hemisphere of the brain becomes saturated with blood, which ultimately leads to serious consequences. The further life of such patients will depend on the degree of damage, timeliness of assistance and the rehabilitation process.
If an ischemic stroke of the right hemisphere occurs, then paralysis of the left side of the body develops. Along with this, patients face the following problems:
- Deterioration of motor functions of the arms and legs. This may be accompanied by a feeling of weakness or a complete lack of control over the left arm and leg;
- Loss of sensation in limbs;
- The occurrence of memory problems, which is accompanied by impaired short-term memory;
- If a person is left-handed, then with such a pathology speech is impaired;
- There is a loss of key reflexes, including swallowing or urinary incontinence;
- The emergence and development of post-traumatic epilepsy syndrome.
Symptoms of a left-sided stroke
Please note: Increasing headaches in the evening, which are not helped by analgesics, as well as a sharp increase in blood pressure and tinnitus, are one of the precursors of a hemorrhagic stroke. Common clinical signs of stroke development are also:
- profuse sweating;
- nausea;
- vomit;
- weakening of the pulse;
- loss of touch on the affected side of the body;
- general weakness;
- numbness of the limbs;
- articulation disorder;
- weakening or loss of vision in one eye (if the lesion is localized in the occipital lobe);
- loss of orientation in space;
- loss of coordination (if the pathological process has affected the cerebellum);
- difficulty swallowing;
- disturbance of the respiratory rhythm (if the focus is in the brain stem).
A left-sided stroke often leads to the development of paralysis of the right side of the body, which is manifested by the disappearance of all forms of sensitivity and a sharp change in muscle tone. Damage to the left hemisphere is characterized by motor aphasia (severe speech impairment). In relatively mild cases, the patient pronounces individual nouns (the symptom is called “telegraphic style”), and against the background of extensive damage, speech virtually disappears.
Important: Speech disorders significantly complicate the diagnosis.
When the lesion is localized in the left hemisphere, a disorder of logical thinking occurs. Patients are very often depressed if the neurons of the left temporal lobe are affected.
Therapy
Treatment of stroke includes basic and specific measures. To begin with, the patient is taken to the intensive care unit and undergoes a course of therapy, the purpose of which is to maintain basic vital functions, including blood circulation, breathing, and also eliminate swelling of the brain.
In the case of ischemic stroke, specific anticoagulant and thrombolytic therapy is carried out. In the case of hemorrhagic damage to the right side of the brain, the treatment, on the contrary, will be aimed at the use of drugs that lead to the formation of blood clots and closure of the bleeding.
Important! Rehabilitation involves undergoing physical therapy, a massage course, taking medications and various physiotherapeutic interventions.
Exercises
As for physical exercises, it is recommended to begin them immediately after the patient’s general condition has stabilized.
At the initial stage, these exercises are performed in a lying position with the help of another person.
So, for example, you should bend and straighten your left arm and leg, and also try to change the position of the fingers that have been paralyzed.
Once the person is able to stand, the exercises will be performed in a standing position.
It is also worth noting that the intensity of physical activity should correspond to the patient’s condition.
Features of patient care after a stroke
Features of patient care after a stroke.
Stroke is an acute disorder of cerebral circulation, most often developing as a complication of hypertension, cerebral atherosclerosis, coronary heart disease, cerebral vascular abnormalities, aneurysms, and diabetes mellitus.
If your ward has one of the diseases listed above, there is a risk of stroke. We will analyze the symptoms of the disease in order to provide first aid in a timely manner during an attack.
There are hemorrhagic and ischemic strokes (cerebral infarction), as well as subarachnoid hemorrhage.
| Hemorrhagic stroke | Ischemic stroke |
| The development of a stroke may be accompanied by emotional distress or physical stress. | Provoking factors include emotional stress, fatigue, and infectious diseases. |
| This is a cerebral hemorrhage. Occurs as a result of rupture of an artery due to fluctuations in blood pressure or the functional state of blood vessels. | Occurs in old age as a result of blockage (thrombosis or embolus) or sharp narrowing of atherosclerotic cerebral vessels. |
|
|
There is also a subarachnoid hemorrhage, which occurs when a cerebral aneurysm ruptures. Characteristic
| |
Home care for patients after a stroke
No matter how severe the stroke may be, with proper treatment and the patient’s active participation in rehabilitation procedures, most of the body’s functions are restored.
The patient needs a full range of procedures for rehabilitation, including therapeutic exercises and massage.
Turn a bedridden patient every two hours to prevent the formation of bedsores. Properly position the patient's paralyzed arm and leg:
In the supine position:
1. To prevent the development of stiffness in the shoulder joint and the appearance of pain in it:
• Place a stool next to the bed, on the side of the paralyzed side, and place a large pillow on it so that the corner of the pillow is under the patient’s shoulder joint.
• Extend your client's arm at the elbow. Place it palm up, straighten your fingers, apply a splint and bandage it to your arm. The longueta should reach the middle of the forearm.
• Move the patient's arm to the side 90° (maintaining a palm-up position) and place it on a pillow so that the shoulder joint and the entire arm are at the same level horizontally.
• Place a roller between your arm and chest so as to fix the arm in the correct position; if necessary, place a 0.5 kg sand bag on the roller.
2. Bend the patient’s paralyzed leg at the knee 15-20°. Place a cushion under your knee.
3. Place your foot in the middle position between flexion and extension and secure it with a stand.
In the “healthy side” position:
• bend the patient’s paralyzed arm at the shoulder and elbow joints and place a pillow under it;
• bend the paralyzed leg at the hip, knee and ankle joints and place a pillow under it.
In the “lying on the paralyzed side” position:
• tilt the patient's head down slightly;
• Stretch the patient’s paralyzed arm forward at a right angle to the body and turn it palm up;
• place the patient’s healthy arm to one side or move it back (but not forward!);
• slightly bend the patient's paralyzed leg at the knee joint, but straighten it at the hip;
• Bend your healthy leg at the hip and knee joints and place a pillow under it.
To maintain mobility of the joints in the paralyzed arm and leg, perform “passive exercises” with the patient: first take the patient’s hand and carefully make certain movements, and then make movements with the patient’s paralyzed leg.
Perform a set of therapeutic exercises with your ward every 4 hours.
Make sure that the movements are smooth and do not cause pain.
Make sure that the patient does breathing exercises. Breathing affects muscle tone.
Keep in mind that the behavior of patients with right-sided paralysis differs from the behavior of patients with left-sided paralysis.
| Right-sided violation - paralysis of the left side of the body | Left-sided violation - paralysis of the right side of the body |
| Underestimating the scale of movement disorders, the patient is indifferent to his situation. | Lethargy, passivity, loss of complex emotional experiences. |
Characteristic:
| Characteristic:
|
|
|
Restoring motor activity after a stroke.
Exiting bed rest should be done gradually and only in consultation with a doctor.
First, they teach the patient to sit down, then do exercises for the legs, then stand up, and only then walk.
If the person in your care cannot sit up independently:
1. Help him sit up first.
2. Then he needs to learn to sit in bed.
3. Provide the bed with special devices so that the patient can sit up without your help.
4. Teach the patient to lower his legs from the bed and transfer to a nearby chair or wheelchair.
5. Gradually teach the patient:
1) stand;
2) transfer the weight of the body from one side of the body to the other;
3) take steps on the spot;
4) to learn to walk, purchase a walker.
6. When teaching walking, stay close to the patient on the affected side.
Helping patients eat after a stroke.
The physician should assess the patient's ability to swallow and chew and prescribe an appropriate diet.
It is easier for a patient with impaired chewing and swallowing functions to swallow soft food than liquid food.
If you are drooling from the paralyzed side of your mouth, make sure your face is dry and clean. Lubricate the skin near your mouth with a protective cream.
Always serve food to your client from the side, on the uninjured side, and place it on the side of the mouth that is not affected.
After eating, make sure that there is no food left in the patient's mouth.
Monitoring the patient.
Watch your skin and take all measures to prevent bedsores.
Such patients often have urinary and fecal incontinence; take proper care of the patient.
To restore a normal sleep cycle:
• lower the air temperature in the patient's room at night;
• reduce the calorie content of food and its temperature (after a hot, hearty meal a person falls asleep);
• organize your ward's daytime so that he has something to do all the time.
Call a doctor if
• there was an increase in temperature, severe pain in the side. Bedridden patients have a high risk of pneumonia;
• swelling appears on the paralyzed side - this may be a sign of vein thrombosis.
Provide your client with emotional support. Reassure him that his family loves and appreciates him regardless of his condition.
https://schule.bz/osobennosti-uhoda-za-bolnimi
Recovery and rehabilitation
In addition to massage and physical activity, the following manipulations will help restore the body’s functioning:
- have a good effect . In this way, sensitivity is stimulated, which speeds up the rehabilitation process;
- Speech therapy and breathing exercises help restore a person’s ability to express thoughts clearly. They consist in communicating with the patient as much as possible;
- Treatment with leeches demonstrates excellent results ;
- Dietary nutrition is important .
Prognosis of paralysis
Is recovery possible if the left side of the body is paralyzed after a stroke?
The general life prognosis for such patients is favorable.
However, it is important to understand that the process of restoring lost abilities and returning to normal life is determined by several factors.
To begin with, what is important is the fact which part of the brain was affected by the pathological process.
Equally important is the volume of hemorrhage. The smaller it is, the less will be the degree of negative impact on the body. One of the key factors is the speed of first aid. And finally, the prognosis for improvement of the patient’s condition will depend on the chosen recovery methods.
Useful video on the topic:
Duration of rehabilitation
How long does it take to recover from a stroke affecting the left side of the body? Rehabilitation from a stroke takes time. Every improvement in a patient's skills and condition is a victory, and over time these small gains begin to add up. For persons receiving rehabilitation services in the conditions of the community of rehabilitation specialists Irakli Pozharisky, the period of rehabilitation work often lasts from two to four weeks. After this, most clients can continue working independently at home.
Care and psychological assistance
Care for these patients will depend on their condition and presenting clinical picture. However, in any case, such people need to be provided with a bed with a raised base at the head. In addition, periodic rubbing of the skin is important for such patients. In order to avoid the formation of bedsores, the patient’s body position should be changed every 3 hours.
Already from 5-6 days after a stroke, you can begin the first measures in terms of rehabilitation. The speed and scale of restoration of lost functions will depend on their regularity and compliance with the patient’s condition. The patient’s chances for maximum recovery depend on how early rehabilitation is started.
If the patient’s loved ones have decided to independently care for him, then they should undergo a special course for the rehabilitation of such patients. However, if the condition of a person with a stroke is extremely serious, then it is better to entrust his care to a professional. In order for a person to be able to independently care for himself and gradually return to everyday life, he needs to re-master these skills.
Important! Psychological assistance is an essential component of recovery. The altered emotional state of such a person may be caused either by the stroke or by a reaction to it.
At a minimum, such a person should be provided with a comfortable and favorable psychological climate, communicate with him and avoid any disputes and conflict situations. If relatives are unable to establish contact with such a patient, then they can resort to the help of a professional psychologist, who should increase the patient’s motivation to recover.
Motor rehabilitation
Passive gymnastics. Motor rehabilitation of patients who have suffered a stroke is an integral and one of the most important components of the recovery process. The basic method of motor rehabilitation is physical therapy, which begins as soon as the patient’s condition allows. The objectives of physical therapy include restoration (full or partial) of range of motion, strength and dexterity in the affected limbs, balance function, and self-care skills.
In the early period, immediately after a cerebrovascular accident occurs, passive gymnastics is performed. It allows not only to normalize the tone of the limbs, but also to prevent the formation of bedsores. Passive gymnastics is performed by exercise therapy specialists together with the patient’s relatives.
When performing gymnastics, passive movements of paretic limbs are performed at a slow pace, carefully, slowly, while trying not to cause pain or increase muscle tone. Such gymnastics is first performed on the healthy side and then on the sore side. It is important to start proximally, in isolation at each joint. In this case, 8–10 movements are performed in each joint.
Active gymnastics. The next stage of recovery is the beginning of active gymnastics, which begins with simple movements of the limbs and becomes more complex as the patient becomes more active. The patient is taught to sit up in bed, maintain balance and stand up, then walk, first accompanied or with support, and then independently.
Great importance is given to motor rehabilitation in the affected upper limb, in particular the restoration of fine motor skills, which is the key to full social and everyday readaptation. The patient learns simple self-care skills, in particular eating, personal hygiene, using the toilet and bathroom, as well as dressing independently, in stages.
The duration of the various stages of motor recovery depends, first of all, on the extent of the area of brain damage. An important part of rehabilitation, both motor and psychological, is the early involvement of patients in household work and the preparation of able-bodied patients to go to work.
Massotherapy
Along with physical therapy, positioning of the lying patient and therapeutic massage are important for the recovery of the patient. The purpose of these therapeutic measures is to prevent the development of muscle contractures and maintain normal joint function, prevent bedsores and pulmonary complications, primarily congestive (hypostatic) pneumonia. When conducting massage sessions, certain principles must be observed:
- the extensor muscles are usually massaged on the arm,
- on the leg - the flexor muscles of the leg and the dorsum of the foot.
Massage is carried out throughout the entire recovery period.
Physiotherapeutic procedures, acupuncture, acupressure, cryotherapy, and water procedures are widely used as additional methods that speed up the rehabilitation process.