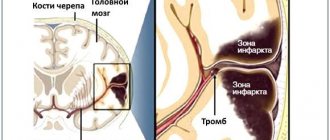
Introduction to an artificial coma after a stroke
Sometimes it is necessary to switch off a person's consciousness with medication to prevent life-threatening brain changes.
In the event of compression pressure on brain tissue, swelling, or hemorrhages and bleeding resulting from traumatic brain injuries, the patient is placed in an artificial coma, which can replace anesthesia during times of crisis.
Long-term analgesia allows you to constrict blood vessels, reduce the tension of cerebral flow, and avoid necrosis of brain tissue.
Sedation is caused by the administration of a controlled high dose of special drugs that have a depressant effect on the central nervous system in intensive care conditions.
This condition can last a long time and requires constant monitoring of the patient's condition. Any reactions to external stimuli or movements indicate the possibility of returning consciousness.
The task of the medical staff is to provide assistance in recovering from a coma.
Introduction to sedation has side effects, including complications of the respiratory system (tracheobronchitis, pneumonia, pneumothorex), hemodynamic disorders, renal failure, and neurological pathologies.
Main consequences of the condition
There are several outcomes that can result from coma after a stroke. Firstly, the patient will return from a dangerous condition with (in rare cases, complete) restoration of vital functions. Secondly, death as a result of brain death, which can occur due to severe hypoxia.
Thirdly, a way out of the situation without restoration of functions, with preservation of paralysis and paresis, as well as with impaired memory and intelligence. Fourthly, the transition to a vegetative state with the preservation of limited reactions to stimuli, while the person cannot speak or think.
Proven fact: full restoration of health is possible only in 10% of cases.
Common Causes
The listed pathologies and injuries in the subtypes of comatose states are not an exhaustive list of possible root causes. Also, not all of them are common. Therefore, it is worth paying attention to the most common causes of coma in people of different ages and conditions. Thus, they can vary significantly among adults, children and pregnant women.
Adults most often fall into a coma when they have a sudden stroke that causes bleeding in the brain. This root cause accounts for approximately 50% of cases. The second place in the frequency of coma development is occupied by drug abuse and is about 15%. They are followed by TBI in accidents, drug poisoning, diabetes and alcohol intoxication. Often, a cancer patient or a person with heart problems may encounter this condition.
Even newborns can fall into a coma. This happens when infected with infections. Children experience noticeable symptoms in a comatose state; the signs usually boil down to convulsions, disturbances in consciousness and hemodynamics. A preschool child may experience this condition due to poisoning with drugs or chemicals. A common cause in schoolchildren is head injuries, and in adolescents – alcohol or drug abuse. Hypoxia and hypovolemia are also considered a common cause for children of any age.
In pregnant women, a coma can develop from heavy loads on a weakened body. Women who have chronic diseases, hereditary predisposition or allergies are most at risk of experiencing this. Very often, the root cause is heart problems, liver dystrophy, nephropathy, eclampsia, diabetes combined with hyperglycemia, atherosclerosis, hypertension, tumors, infections, as well as excess lactate or lack of insulin.
Coma can be dangerous not only for the pregnant woman, but also for the fetus. The risk of losing a child in this condition is very high.
Degrees of condition
How long a coma will last after a stroke depends on the initial condition of the patient, but this time is usually 2-10 days. Less often, the patient is in a state of sleep for less than 24 hours. A person is rarely unconscious for several years or months after a blow.
- Why does coma occur during a stroke and are there any chances?
It is impossible to determine exactly at the moment sleep begins how many people will remain in it.
But there is one important pattern: the longer a person is in this state, the lower the risks of surviving and returning to normal life. The duration of sleep also affects the ease of recovery after being in a coma. In 70-90% of clinical cases, a person remains with 1-3 degrees of disability, and important body functions are lost. There are 4 degrees of coma after a stroke:
- Pre-coma . The person is in normal consciousness, his muscles are working, but lethargy and loss of tone are noticeable. Partial numbness of the skin occurs. At this stage, the transition to unconsciousness can be prevented
- Second degree . At this moment, the person falls into a deep unconscious sleep and stops responding to any stimuli. Breathing gradually changes: it becomes noisier and more intermittent, and the muscles begin to contract involuntarily.
- Third degree . It is formed mainly during a major stroke. The person completely loses consciousness, physiological reactions, including muscle cramps, go away. The temperature is decreasing.
- Fourth degree . In this case, the chances of surviving a coma caused by a stroke are almost zero. Even spontaneous breathing, which remains a reflex, is absent. The person is connected to special devices.
In unconscious sleep, a person needs special care from medical personnel: he is fed, served, and kept alive in accessible ways.
Degrees of coma
To simplify differentiation, doctors distinguish the following degrees of coma during strokes:
- 1st degree . It is determined by lethargy or loss of consciousness with preservation of reflexes. This is mild damage to brain cells during a stroke and slight depression of the functions of the nervous system. At the same time, skin reflexes are weakened and muscle tone is increased;
- 2nd degree . It is diagnosed by the patient falling into deep sleep, lack of response to external stimuli, skin reflexes and pain;
- 3rd degree . It is caused by extensive hemorrhage and is determined by the absence of many reflexes, consciousness, and the reaction of the pupils to light;
- 4th degree . It is not comparable to life, as it is characterized by the absence of spontaneous breathing, a sharp decrease in pressure and hypothermia. All reflexes are absent. A patient in this stage of coma has virtually no chance of returning to normal life.
Therapy
After transporting the patient to a medical facility, doctors from the intensive care unit will take charge of his health. The first actions will be aimed at ensuring breathing and blood circulation using hospital devices. After this, the patient awaits an urgent examination in order to make an accurate diagnosis and confirm the coma.
Diagnosis is made by taking an anamnesis. If the victim remains unconscious, his relatives may be called in to help. Doctors will also conduct a physical and neurological examination to assess the condition of the body. If anyone is suspected, their stage will be assessed using the Glasgow scale or another relevant one at that time. In addition, you will need to conduct laboratory tests with the study of blood and urine, neuroimaging and measure intracranial pressure. If the diagnosis remains unclear, an EEG or lumbar puncture may be prescribed.
The basis of treatment is various medications aimed at eliminating the root cause of coma. Doctors have to be very careful in their choice, since a coma makes it impossible to use some drugs. The patient’s survival will depend only on correctly selected medications.
Types of medications:
- anticonvulsants;
- sedatives;
- antiemetics;
- antipyretics;
- antibiotics;
- vitamin B;
- glucose.
If there is a suspicion of poisoning by low-quality food or medications, the patient may also be prescribed gastric lavage. If there are tumors or some other damage to the brain, surgery is often required.
The sooner the doctor begins treatment, the higher the chances of a positive outcome.
Prognosis and consequences of coma
Coma after a stroke is a dangerous condition; the prognosis of patients is disappointing and depends on the patient’s condition, the degree and timely response of doctors. It is extremely rare for older people to regain consciousness. The chances of recovery are reduced if the duration of coma exceeded 14 days. Patients with stage 1 have the most favorable prognosis, stage 2 gives questionable results, and with stage 3-4 the person does not recover from coma. If the patient manages to regain consciousness, it will take a long time to recover.
The risk of complications increases in parallel with the length of time a person remains in this condition. The patient may develop heart failure, nervous system disorders, infections, and bedsores. The result of mechanical ventilation is often:
- pneumonia;
- tracheobronchitis;
- stenosis.
Fistulas often form on the walls of the esophagus, gastrointestinal functions are disrupted, renal failure, sepsis develop, and blood circulation is impaired. Urinary retention can cause peritonitis and bladder rupture. Symptoms of heart failure and nervous system disorders often persist long after recovery from a coma. The following are considered fatal risk factors:
- recurrent stroke of any type;
- excess of more than 15 mg/l of creatine in the blood;
- complete loss of response to treatment and pain;
- existing brain damage;
- presence of twitching for more than 3 days;
- The patient's age is over 65 years.
If the patient ends up in the hospital in a timely manner, doctors will have the opportunity to stop the comatose process and reduce the severity of possible consequences.
- How many days does a coma last after a stroke and is there a chance of survival?
First aid
An inexperienced person will not be able to distinguish a sudden coma from a normal loss of consciousness. Since these are completely different phenomena in terms of danger, under no circumstances should you take rash actions to provide assistance. It is necessary to immediately call an ambulance so that specialists can determine the real condition of the patient. While waiting for the team, it is necessary to take important pre-medical measures aimed at preventing blockage of the airways.
Necessary actions:
- Place the victim in a lateral position.
- Unbutton the top of your clothing and loosen the collar.
- If he is partially conscious, find out what happened, clarify the location of the pain, ask about chronic diseases and the availability of medications.
When the ambulance is on site, all that remains is to quickly transport the person to the nearest hospital. In this case, the patient will be provided with respiratory function support using an oxygen mask, blood circulation will be stimulated, and the cervical spine will be stably fixed. If necessary, he will be given the necessary medications.