Prognosis after ischemic, hemorrhagic
Cerebral hemorrhage usually occurs in a more severe form. The mortality rate in such patients reaches 70%; even after removal of the hematoma, the rate is not much lower. Unfavorable factors include:
- breakthrough of blood into the ventricles of the brain;
- uncontrolled arterial hypertension;
- large volume of hematoma;
- progressive cerebral edema;
- signs of displacement of the stem part;
- acute heart failure;
- increase in creatinine content in the blood;
- convulsive syndrome, lack of consciousness, reactions to painful stimuli for more than 3 days;
- age after 70 years.
With ischemic stroke, a more benign course is observed; it is rarely accompanied by a profound impairment of consciousness. This happens with repeated vascular accidents, massive blockage of the brain arteries with cholesterol plaques, lack of treatment or complete disregard of doctors’ recommendations.
Blockage of arteries in the brain
Precoma and the first degree of coma can still give the patient a chance for recovery; with a higher degree, the prognosis is considered doubtful, and the onset of extreme coma is usually regarded as fatal.
Severity of coma in older people
- Prekoma. In this state, elderly people experience slow reaction, weakness, confusion, or, conversely, develop psychomotor agitation. Pathologies occur in the functioning of internal organs according to the characteristics of the disease that caused the onset of coma in an elderly person. Reflex reactions remain.
- Coma I degree. The patient begins to develop deafness, and the reaction to stimuli is inhibited. An elderly person in a coma of this degree is able to swallow liquid food and perform simple movements, but it is already quite difficult to establish contact with the patient. Reflex reactions are inhibited or exaggerated depending on the type of coma.
- Coma II degree. In this state, the patient experiences deep sleep, sometimes uncontrolled movements of the limbs appear, and contact is impossible. An elderly person in a coma experiences pathological noisy breathing, arrhythmia, and involuntary emptying of the bladder and intestines. There are no reflex or pupillary reactions, skin sensitivity does not appear.
- Coma III degree. Patients lack consciousness, pain sensitivity, reflex reactions, and the pupils are dilated. An elderly person in a coma experiences a decrease in body temperature, depressed breathing and a drop in blood pressure.
- Coma IV degree. Patients are diagnosed with complete impairment of consciousness, absence of reflex reactions and muscle tone, decreased body temperature and blood pressure, sudden stops in respiratory movements, which requires connecting the patient to a ventilator.
Read material on the topic: Life after 80 is just beginning
Consequences
If patients can be saved, they experience neurological deficits—symptoms caused by damage to the area of the brain where the hemorrhage occurred.
These may be consequences of a hemorrhagic stroke:
- paresis and paralysis - impaired movement of the limbs on one half of the body, since they are constantly in a half-bent position and it is impossible to straighten them;
- speech impairment and its complete absence;
- mental disorders and irritability;
- constant headaches;
- movement coordination disorders;
- inability to walk or even sit independently;
- visual impairment up to complete blindness;
- facial distortion;
- vegetative state - the absence of any signs of brain activity (consciousness, memory, speech, movements) with preserved breathing and heartbeat.
Symptoms of the disease and their duration depend on the location of the hemorrhage and its volume. The first 3 days are the most dangerous, since during this time severe disorders occur in the brain. Most deaths (80–90%) occur during this period. The remaining 10–20% of patients die within one to two weeks. Patients who survive recover gradually from a few weeks to 9–10 months.
Provocateurs of hemorrhagic stroke
The trigger for the appearance of HI can be quite a variety of factors that have a negative impact on intracranial hemodynamics and the condition of the cerebral vessels:
- persistent arterial hypertension (in 50% of cases);
- cerebral amyloid angiopathy (12%);
- oral administration of drugs from the anticoagulant spectrum (10%);
- intracranial neoplasms (8%);
- other causes are arteriovenous and cavernous malformations, thrombosis of the cerebral sinuses, aneurysms, vasculitis of intracranial vessels, etc. (20%).
Many of the patients with a history of hemorrhagic stroke have diabetes mellitus. It is a proven fact that diabetics, like hypertensive patients, are at risk. In long-term diabetes mellitus, blood vessels, including cerebral ones, are destroyed due to modification of blood chemistry with a predominance of glucose. If, against the background of elevated blood sugar, there is a tendency to constant increases in blood pressure, the likelihood of a hemorrhagic stroke increases by 2.5 times.
Pathogenetically, a hemorrhagic effect can develop as a result of rupture of a vessel (the predominant mechanism) or the leakage of blood elements into the surrounding brain tissue through the walls of capillaries due to their impaired tone and permeability. In the second option, there is no rupture and, as such, profuse hemorrhage. Just a small vessel allows blood to pass through pointwise. But even small-point hemorrhages, merging, can turn into very extensive foci, with no less fatal consequences than after a rupture of an artery or vein.
What it is?
Hemorrhagic stroke is an acute hemorrhage in the brain due to rupture or increased permeability of blood vessels. This cerebrovascular accident differs from classic (ischemic) stroke, which is more common (70% of patients).
The nature of changes in blood vessels during an ischemic stroke is the blockage of their lumen by blood clots, resulting in gradual necrosis of brain cells, and in a hemorrhagic stroke there is a violation of the integrity of the vascular wall, as a result of which the brain tissue is saturated and compressed by the gushing blood.
Hemorrhagic cerebral stroke is a dangerous and insidious disease. It is characterized by:
- High mortality (60–70% of patients die within the first week after the onset of the disease).
- Suddenness (in 60–65% of patients, hemorrhage occurs without any previous symptoms).
- Profound disability of surviving patients - 70–80% of people are bedridden and cannot care for themselves, the remaining 20–30% have a less pronounced neurological deficit (the function of the limbs, walking, speech, vision, intelligence, etc. is impaired)
More than 80% of brain hemorrhages are associated with increased blood pressure (hypertension). By taking antihypertensive drugs (blood-lowering drugs), you can reduce the risk of stroke, the amount of hemorrhage and the severity of brain damage. If patients are admitted to a medical facility within the first 3 hours, this increases the chances of survival. Specialized rehabilitation centers help restore lost brain functions as much as possible after a stroke. Complete cure is rare, but possible.
Treatment
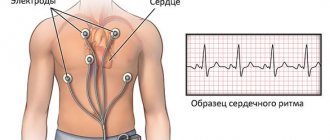
Treatment begins with stabilizing the respiratory rate (respiratory rate), and it is also very important to restore all functions of the cardiovascular system. The development of a treatment plan should begin only after all necessary research has been completed. It is very important to quickly replace all vital functions with artificial ones. For example, supplying oxygen to the body, stabilizing body temperature, and providing nutrition are very important.
Hemorrhagic stroke is treated only with surgery. With this operation, bleeding in the brain is eliminated and the aneurysm, which was the causative agent of the bleeding, is clogged. After all these manipulations, the swelling begins to rapidly subside. Such an operation requires a highly qualified neurosurgeon.
Prognosis, recovery after coma
Post-stroke coma is considered the most severe type of coma (1):
- Stroke on the left side: consequences and features of recovery. How long do people live with this diagnosis?
- only 3% of patients manage to recover and fully recover;
- 74% of comas after a stroke end in death;
- 7% of patients manage to regain consciousness, but they lose all higher functions (the ability to think, talk, perform conscious actions, carry out commands);
- 12% of patients remain deeply disabled;
- 4% of people recover, maintaining moderate impairment.
Factors influencing the forecast:
- Localization of the focus of necrosis. If a stroke affects the medulla oblongata, where the centers for controlling breathing and heartbeat are located, death occurs very quickly.
- Duration of coma: the longer it lasts, the less hope for a full recovery, the higher the risk of death.
- Depth of coma. In medicine, the Glasgow scale is used to assess it. During the examination, the doctor tests a person’s ability to open their eyes when exposed to various stimuli, speech, and motor reactions. For each attribute a certain point is awarded (table). The lower the score, the less favorable the outcome for the patient.
| Reaction | Ball |
| Eye opening when pressed | |
| There is | 2 |
| No | 1 |
| In response to the patient's question | |
| answers inappropriately | 3 |
| makes strange sounds | 2 |
| does not react | 1 |
| When a limb is pinched forcefully | |
| withdraws | 4 |
| bends | 3 |
| unbends | 2 |
| does not react | 1 |
Coma degree (based on total points):
- 6-7 – moderate;
- 4-5 – deep;
- 0-3 – brain death.
When is coma possible in older people?
In a comatose state, consciousness is switched off, and reactions to external stimuli are completely absent.
Coma in older people develops as a result of acute circulatory disorders in the brain, which leads to damage to the central nervous system and changes in the functioning of vital body processes. The duration of the coma lasts about 2–4 weeks. The outcome directly depends on the reasons that caused it, the severity and location of the damage. When recovering from a comatose state, older people have a high probability of developing physical, psychological, and intellectual pathologies. After regaining consciousness, tests are performed to help assess the patient's health. The source of coma can be:
- cerebral circulatory disorders;
- diabetes;
- brain injuries and tumors;
- acute renal or liver failure;
- violation of water and electrolyte metabolism in the body;
- stroke;
- intoxication of the body.
Read material on the topic: Diseases of old age: types, causes, symptoms
Causes
Post-stroke cerebral coma is a common complication of hemorrhagic and ischemic stroke of the brain. This condition occurs when a major brain accident disrupts the normal functioning of the central nervous activity.
The following conditions can trigger ischemic stroke:
- Atherosclerosis of cerebral vessels. When intravascular proliferation of an atherosclerotic plaque occurs, a blockage of the lumen of this vessel is observed, leading to disruption of the nutrition of a separate area of the brain;
- Hemodynamic disorders. With constant lability of blood pressure and organic disorders in the vessels of the brain, a violation of the nutrition of soft tissues occurs;
- Cardioembolic disorders. In this case, the blockage of blood vessels in the brain is caused by blood clots brought in from the heart valves or heart chambers. Conditions such as myocardial infarction and arrhythmia can provoke blood clot detachment.
The following factors contribute to the development of so-called coma and hemorrhagic stroke:
- Presence of vascular aneurysms;
- External damage to large vessels;
- Defect in the development of the blood vessel wall.
Hemorrhagic cerebral stroke is a more severe and life-threatening condition. This condition is associated with cerebral hemorrhage. Brain hemorrhage is difficult to deal with. Coma after a hemorrhagic stroke is more difficult to tolerate.
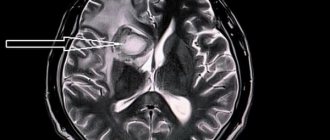
Diagnostic methods
In the acute phase of a hemorrhagic stroke, the patient must be urgently examined to preliminarily determine the prognosis and select treatment tactics. The condition is complicated by the following factors:
- extensive hematoma in the brain tissue, which occupies an area of 7 square cm or more;
- large intraventricular hematomas - more than 2 square cm;
- high blood pressure;
- elderly age of the patient;
- any chronic diseases;
- presence of dislocation syndromes.
Dislocation syndromes are signs of an increase in the volume of the brain with a subsequent change in its localization in the skull. Using these symptoms, you can determine in which area the main pathological focus is located, as well as predict the chances of recovery. The primary diagnosis of strokes is based on the clinical picture, so dislocation syndromes play an important diagnostic role. In total, there are 9 options for how the brain matter can shift. However, when diagnosing strokes, 2 of them are most important.
How many days does the coma last?
It is impossible to predict with accuracy how long a coma will last after a stroke. There are a number of factors that can affect the prognosis:
The age of the patient - the younger the person, the greater the chance that brain cell regeneration will occur faster. The area of ischemia - the larger the area of brain damage, the less chance of exiting the coma and returning to your previous life. Localization and cause of stroke - blockage of small vessels, which can be corrected, is less dangerous than an aneurysm or thrombosis of large coronary vessels. Speed of first aid – the earlier a stroke is noticed, the greater the likelihood of a favorable outcome. Diagnostics - it is important to identify not only the area of brain damage, but also the root cause that provoked what is happening. Type of stroke - hemorrhagic stroke has a more rapid development and more disappointing prognosis than ischemic stroke.
There are medical statistics that provide approximate data on whether a person is in a coma to varying degrees:
- The first stage - on average, the patient recovers in 10-14 days, which usually takes place in the intensive care unit and intensive care wards (it is impossible to treat coma at home). During this time, all vital functions are restored, and brain function is normalized.
- The second stage - when appropriate measures are taken, the person regains consciousness within 3-5 days, and complete rehabilitation and restoration of other functions can take up to 1 year. In half of all cases, a person is able to come out of a coma on his own, as soon as the drug therapy has shown the first results.
- The third stage – the probability of returning to consciousness is only 25%, which persists only for people under 45 years of age. After this age, there is a high probability of developing a vegetative state, which is characterized by the loss of all reflexes and functions.
- The fourth stage is characterized by complete swelling of the brain. The prognosis is the most unfavorable, and the number of people around the world who have returned to their former lives after stage 4 coma can be counted on one hand. A vegetative state, in which all vital processes are carried out by special devices, can last for years. Although in practice, after the third month of the last stage of coma, there is no point in supporting the patient’s vital functions, since irreversible processes that have already occurred will not allow the person to ever be the same as before.
However, these figures should not be taken as a scientifically established and fixed indicator. The numbers are taken from general statistics of all patients who have suffered a coma.
We must not forget that even with the first degree of coma, death can occur, just as the third degree does not guarantee a 100% fatal outcome.
Thus, coma accompanying a stroke is a dangerous physiological condition with a high risk of death.
Only timely seeking medical help can reduce the risk of worsening a stroke, giving a person a chance for a full recovery. A stroke suffered on the feet or at home, without appropriate medical care, increases the risk of death to 98%, which develops within 2-3 days.
What is the prognosis for treatment of stupor after a stroke?
For stupor after a stroke, it is important to start the course of treatment as quickly as possible. No one can guarantee a forecast for successful completion.
If the condition is caused after an illness, including oncology, the chances of a complete recovery are extremely small, but they exist.
When in a stuporous state that arose after using drugs, the situation can take on a positive aspect. Even if brainstem reflexes and motor reactions have disappeared, the prognosis for successful treatment still remains.
The prognosis for the treatment of stupor is even better when the patient is provided with careful and careful care
It is important not to allow stimulants, opiates, etc. to be taken. It is necessary to properly feed, care for the patient’s face and prevent bedsores.
https://mozgvtonuse.com/bolezni/sostoyanie-sopora.html
Patient care
A comatose person is in intensive care, where his existence is supported by machines. Coma is a condition in which the heart continues to beat and the ability to breathe on its own is almost always maintained. Only consciousness is missing, which means that a person is unable to move, speak, hear and see, as well as cope with natural needs.
A patient in a coma needs care: feeding, hygiene, massage. Medical measures are required.
- Nutrition. Food enters the patient's stomach through a tube. To prevent dehydration, supporting vitamin drips are placed. The food itself is a mixture in powder form, similar to baby formula. It is prepared in the same way. You can also use baby fruit and vegetable purees.
- Hygiene. Every day it is necessary to wipe the body with a cloth soaked in soapy water and clean the patient’s mouth with a damp gauze cloth. You should wash your hair at least once a week. There are special care products for bedridden patients: lotions and foams for wiping the skin, napkins, caps for washing hair with shampoo.
- Massage. To prevent bedsores from forming on the body on the legs, shoulder blades and buttocks, you need to periodically turn the patient over, making light massage movements - the doctor will show them.
- Medical prescriptions for hemorrhagic stroke. If the patient has had a hemorrhagic stroke, then the possibility of recovery can only be discussed after removal of the hematoma in the brain through surgery. Neurosurgeons perform this procedure. A favorable outcome for hemorrhagic stroke is much less common than a fatal one. Subsequent treatment of a comatose patient takes place in the neurology department in the intensive care unit. If life-supporting functions are impaired, the patient is connected to a ventilator and a monitor on which all the necessary indicators are visible. They support the normal functioning of the body.
- Medical prescriptions for ischemic stroke. For ischemic stroke, the patient is prescribed anticoagulants and antiplatelet agents - Heparin, Trental, Warfarin, Acetylsalicylic acid, as well as drugs to stimulate cerebral circulation - Cereton, Actovegin, Gliatilin, Noocholin.
To protect against infections, a patient during a coma after any type of stroke is prescribed antibiotics and hepatoprotectors that restore the liver. Maintenance therapy must be supplemented with vitamins and minerals.
How to determine if a person is in a coma
Coma during a stroke is very similar in symptoms to fainting, but fainting passes quickly, and coma can last from 2-3 hours to several years. This persistent vegetative state is called a prolonged coma. Patients who have been unconscious for more than a year rarely return to life. The main characteristic of a comatose state: the patient does not react to anything and does not perform any actions.
Who is characterized by a complete or partial absence of reflexes - in many cases, a person cannot breathe, eat, or control urination on his own. He does not react to external stimuli - pain, sound, light. But don’t think that this always happens: symptoms may differ for each patient. For example, a coma can be so deep that all vital processes are performed for a person by devices (breathing, nutrition, excretion of urine and feces), and it happens that some reflexes are preserved and the patient, for example, can swallow food.
Another important issue regarding the symptoms of coma is brain activity.
Due to the fact that a massive hemorrhagic or ischemic stroke causes someone, the condition must be completely unconscious, because the brain tissue dies and, accordingly, can no longer perform its function. But some patients, having recovered from a coma, claim that they heard their relatives talking to them. Scientists confirm that this is possible, attributing the condition to unexplored brain reserves.
So, we can assume that a person is in a coma due to a stroke based on the following signs:
- The patient stops responding to external stimuli - pain, sound, light. The condition lasts for more than an hour.
- Breathing is often shallow, barely noticeable, and the pulse cannot be traced.
- Reflexes disappear - the patient cannot hold feces and urine.
- The heartbeat slows down or, on the contrary, increases.
Symptoms vary depending on the type of stroke. With a hemorrhagic stroke, coma occurs quickly; with an ischemic stroke, the immersion lasts from several hours to 3 days. Monitoring the onset of coma is very important - the condition can be prevented.
- With a hemorrhagic stroke, the patient's face suddenly turns red, becoming almost burgundy. He loses consciousness. The blood pressure is elevated, the pulse is clearly visible, breathing is loud with wheezing. The cheek on the paralyzed side droops. The eyeballs diverge to the sides or float. The pupils are unevenly constricted and practically do not react to light. The paralyzed side does not respond to pain, tendon reflexes are practically absent. The condition is accompanied by urinary incontinence and vomiting.
- For ischemic stroke. Usually the patient complains of malaise and dizziness - he often yawns, his speech loses coherence. Consciousness is gradually upset - up to 3 days, during which time (even before the coma) paralysis of the limbs can occur. The patient is pale, the pulse is arrhythmic, weak, breathing may become rapid or remain normal.
Even if the signs coincide, do not rush to draw conclusions - an accurate diagnosis is always made by a doctor. The doctor examines the condition using the AVPU scale or the Glasgow scale. Also, in order to understand what exactly happened and take action even before receiving the examination results, the doctor interviews relatives who may have observed the precomatose state.
It is important for those who were nearby to remember all the events and answer the doctor’s questions as accurately as possible. Consider whether the patient has had a stroke, epilepsy, diabetes, dizziness, vision problems or numbness in the limbs, whether he was taking medications, and how quickly the loss of consciousness occurred.
How to bring a person out of a coma
It’s worth starting with the fact that even from a severe coma, about 9-10% of patients return. At the same time, many continue to live in a normal state, without turning into a “vegetable”. In such patients, lost brain functions are restored, but this process can take quite a long time. It all depends on the degree of damage to the brain cells.
Coming out of a coma looks like this:
- The ability to swallow returns, muscles and skin begin to respond to irritants. The motor reflex is restored, the patient can turn his head.
- Consciousness returns slowly, but the patient begins to experience hallucinations. You should not be afraid of this - in this case it is a sign of positive dynamics. Speech, memory and vision are partially restored.
- The patient tries to move, sit independently, then begins to stand up and move around with support.
As soon as the patient regains consciousness, he undergoes a tomography to diagnose the extent of brain damage and select restorative therapy.
The rehabilitation process requires a lot of strength, both physical and moral, and not only from the patient - the most important role in his fate is played by close people. The main goal of rehabilitation is to prevent destruction of other parts of the brain. To do this, you will have to work out a lot and for a long time, performing a set of special exercises.
The task of relatives is to help the victim recover from the experience and create favorable conditions for the restoration of his normal functioning. To reduce the likelihood of a recurrent stroke, relatives need to follow some recommendations:
- Praise the patient even for small progress.
- Give hope for a full recovery.
- Create a homely environment and a favorable psychological climate around you.
- Learn how to massage and help the patient restore body functions.
Love and care work wonders. Pay more attention to the patient, this will help him recover faster.