- Thrombotic vascular lesions
- Fat embolism
- Air embolism
- Which vessels can be affected by embolism and how does it manifest?
- Carotid embolism
- Occlusion of mesenteric vessels and renal artery
- Peripheral vascular occlusion
- Treatment and prevention of pathology
- Prevention and treatment of fat embolism
- Prevention and treatment of air embolism
- Amniotic fluid embolism
- Causes
- Treatment and prevention
Vascular embolism is a condition in which the lumen of a blood vessel is completely or partially blocked. This leads to disruption of blood supply, which causes oxygen starvation of tissues. If left untreated, they gradually die off as the cells stop receiving oxygen and nutrients. Vessel blockage can be caused by:
- blood clots;
- particles of adipose tissue;
- air bubbles;
- foreign objects.
Regardless of the cause, vascular embolism poses a threat to the health and life of the patient. This condition requires treatment, which can be conservative or surgical.
Thrombotic vascular lesions
It is the most common type of embolism and can occur with the following diseases:
- varicose veins;
- heart disease (heart attack, myocarditis, etc.);
- excess body weight;
- thrombophilia.
The risk of pathology increases with a hereditary predisposition to thrombosis, after extensive surgical interventions, when taking hormonal contraceptives, and low physical activity. The most dangerous for the patient are thrombotic lesions of the great vessels of the brain, kidneys and intestines. In this case, there is a direct threat to life due to the development of tissue necrosis of vital organs. If treatment is not carried out in a timely manner, the patient's life can be saved, but he may remain disabled.
If a blood clot occludes a peripheral vessel, gangrene of the limb may develop and amputation may become necessary. Thromboembolism of peripheral arteries is easier to diagnose, which helps prevent severe complications.
Pulmonary thromboembolism is very life-threatening. A blood clot can block the main trunk of the pulmonary artery or its branch. This condition occurs suddenly, and the pathology leads to a very rapid deterioration in the patient’s well-being. He develops cardiopulmonary failure, which ends in cardiac and respiratory arrest.
The main cause of the pathology is the migration of a blood clot from the veins of the lower extremities or pelvis.
Literature
1. Gladyshev V.Yu. Diagnostic and operative hysteroscopy. Met. recommendations. Voronezh.2008; 89. 2. Zilber A.P., Shifman E.M.. Obstetrics through the eyes of an anesthesiologist. Sketches of critical medicine. Petrozavodsk: PGU Publishing House, 1997. 3. Savelyeva G.M., Breusenko V.G., Kapusheva L.M. Hysteroscopy. M.: GEOTAR-MED, 1999; 176 p. 4. Sarkisov S.E., Kukovenko E.M., Litvintseva N.G. Materials of the VIII All-Russian Forum “Mother and Child” 2006; 509–510. 5. Tito V., Peretz-Tamayo A. Pulmonary embolism. Clinical surgery. M.: 1998; 466–476. 6. Elbin M.S. Scientific review. Emergency Medicine 2008; 3(16). 7. Wolf S., Albin MS, Winnem B. Spontaneous migration of a central venous catheter and its repositioning: Technical note. Neurosurgery. 1980; 6: 652.
Fat embolism
Pathology occurs:
- when injecting oil solutions;
- for injuries and damage that are accompanied by bone fractures and vascular injury;
- with necrotic lesions of pancreatic tissue.
Lipid droplets enter the blood from the yellow bone marrow if the damaged bone is damaged or as a result of surgery. They are able to merge into a single whole and move with the bloodstream throughout the body. Having reached a certain size, the accumulation of adipose tissue particles blocks the lumen of the vessel. Most often, the pathology affects the tissues of the spinal cord, brain, heart, and lungs.
Air embolism
The pathology is characterized by blockage of the vessel with air or gas bubbles. The reason is:
- improper administration of intravenous injections;
- damage to large vessels;
- decompression sickness.
If a large vein is injured and the bleeding is not stopped in time, air can get inside and move with the blood along the arterial bed, which ultimately leads to a blockage. A type of air embolism is gas embolism, which is caused by the so-called decompression sickness. It develops in people who engage in scuba diving. If a person rises to the surface too quickly, the inhaled gas mixture does not have time to be absorbed. Air bubbles block the vessels and lead to embolism. The person may lose consciousness, and in severe cases, a stroke is possible.
A comment
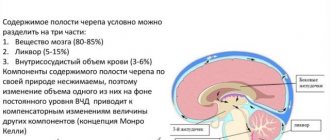
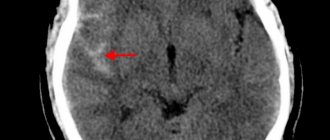
The team of authors provides a clinical observation of the development of venous and paradoxical air embolism in a patient with a brain stem tumor. This is a very serious and sometimes fatal complication of neurosurgical operations performed on patients in a sitting position. The article discusses various approaches and methods previously published by domestic and foreign researchers, aimed at both preventing the development of air embolic complications and their treatment. Algorithms for pre- and intraoperative examination and patient management are discussed. During the discussion of this clinical observation, the authors provide literature data on the possible causes of venous and paradoxical air embolisms in neurosurgical practice.
In the presented clinical case, a paradoxical air embolism that developed during neurosurgical intervention in a sitting position led to the formation of acute myocardial infarction and cerebrovascular accident, which ultimately caused the death of the patient. The authors focus readers' attention on methods for pre- and intraoperative diagnosis of these complications, pointing out that effective methods for treating venous and paradoxical air embolism have not currently been developed. The authors come to a conclusion, one of which indicates the need to switch to performing neurosurgical interventions in the supine position in all technically possible cases and to avoid surgery in the sitting position as much as possible to reduce the risk of developing air embolic complications.
The article may be useful not only to neurosurgeons and anesthesiologists-resuscitators, but also to all related specialists involved in the treatment of patients with brain damage.
S.V. Sviridov (Moscow)
Which vessels can be affected by embolism and how does it manifest?
Blockage of the lumen can occur in any vessel. Depending on the location of the pathology, its symptoms vary. Signs of arterial embolism are:
- a sharp drop in blood pressure;
- irregular pulse and breathing;
- sweating;
- pallor;
- chest pain that radiates to neighboring areas of the body;
- weakness, dizziness;
- loss of consciousness.
Carotid embolism
Signs of pathology are:
- weakness and dizziness;
- headache;
- deterioration in coordination of movements;
- fainting state.
Occlusion of mesenteric vessels and renal artery
In this case, the superior and inferior mesenteric arteries are affected. The pathology is manifested by severe abdominal pain, bloating, loose stools mixed with blood, and impaired intestinal motility.
If there is a blockage of the renal artery, the patient experiences severe pain in the lower back. The functioning of the kidney is disrupted, which causes difficulty urinating until it completely stops, and blood is released in the urine.
Peripheral vascular occlusion
Embolism of the arteries of the extremities leads to pain in the affected area, which is accompanied by spasms and muscle cramps. Due to impaired blood supply, the skin turns pale. Trophic ulcers appear on the surface - non-healing wounds that can lead to gangrene.
Treatment and prevention of pathology
Treatment of the disease depends on its type. A treatment protocol has been developed for each type of pathology. It is aimed at normalizing vital functions and eliminating the cause that led to blockage of the vessel.
Conservative therapy includes taking medications:
- anticoagulants;
- glycosides;
- fibronolytics;
- glucocorticosteroids.
If the pathology occurs due to injury or infection, antibiotics are prescribed.
A patient with thromboembolism is prescribed ozone therapy, which eliminates the lack of oxygen in tissues and has a bactericidal effect.
If drug therapy is not effective enough, surgery is performed to remove the blood clot. To prevent thromboembolism, it is necessary to regularly monitor blood clotting parameters. There is a special analysis for this - a coagulogram. If necessary, a patient at high risk of thrombosis should take anticoagulants.
Varicose veins and heart disease are factors that provoke thrombotic damage to the arteries. If you have such diseases, it is important to monitor your condition and undergo timely treatment.
Prevention and treatment of fat embolism
In case of fat embolism, the patient needs to be hospitalized in the intensive care unit and connected to a ventilator. Drug therapy involves taking drugs that dissolve fatty particles. The patient is also prescribed anticoagulants, cardiac glycosides, and oxygen therapy.
To prevent fat embolism, it is necessary to eliminate factors that could cause lipid particles to enter the blood. In case of fractures, it is important to stop the bleeding as soon as possible, correctly fix the injured limb, monitor the patient’s condition, and control blood pressure.
Prevention and treatment of air embolism
If there are signs of pathology, the patient needs emergency care. He is fitted with a venous catheter for air aspiration and connected to an artificial respiration apparatus. To eliminate tissue hypoxia, oxygen instillations and hyperbaric oxygenation are performed.
To prevent air embolism, scuba divers must strictly follow safety rules when ascending from depth to the surface in order to prevent decompression sickness. The pathology can be caused by air entering an injured blood vessel, so it is important to promptly provide medical care to patients with such injuries and monitor their health.
When injecting drugs into a vein, it is important to follow safety requirements to avoid air bubbles entering the vessel.
O.V. Vozgoment
PGMA named after.
acad. E.A. Wagner, Perm We describe a case of a rare complication of liquid hysteroscopy, presumably an air embolism, which was the cause of an unfavorable outcome in a 45-year-old woman. The conclusion about the probable nature of the complication that arose was made on the basis of an expert assessment of the clinical situation and contrary to the conclusion of the forensic expert about sudden coronary death, for the occurrence of which there were neither morphological nor situational reasons.
Key words: hysteroscopy, complication, air embolism, examination.
About the author:
Vozgoment Oleg Vasilievich – Candidate of Medical Sciences, Associate Professor of the Department of Anesthesiology and Reanimatology of the Perm State Medical Academy named after. acad. E.A. Wagner
Amniotic fluid embolism
Amniotic fluid embolism is a pathological condition in pregnant women. It occurs when amniotic fluid enters the mother's bloodstream. This liquid contains prostaglandins and other components, the effect of which causes an anaphylactoid reaction.
Pathology manifests itself in the following forms:
- swelling of the lung tissue with the development of acute respiratory failure;
- cardiac shock, which is characterized by a thread-like rapid pulse, a sharp decrease in pressure, nausea and vomiting, pallor, bluish skin, loss of consciousness;
- convulsive syndrome, which affects all muscle groups;
- hemorrhagic bleeding from the nose and mouth, vagina;
- multiple organ failure, which manifests itself as a disruption in the functioning of the main organs and systems.
Causes
Amniotic fluid can enter the bloodstream of a pregnant woman if the pressure inside the uterus increases, the pressure in the veins of the uterus decreases, or if the vessels that contact the amniotic sac are damaged.
Risk factors are:
- multiple pregnancy or high fetal weight;
- breech presentation of the fetus;
- polyhydramnios;
- low elasticity of the cervix;
- rapid labor;
- individual anatomical features of the birth canal.
The development of embolism against the background of a decrease in venous pressure can occur in patients with diabetes mellitus, heart defects, and preeclampsia. Women with low vascular tone due to frequent childbirth and patients taking diuretics and antihypertensive drugs are susceptible to pathology.
The entry of amniotic fluid into the blood due to damage to the amniotic sac and vascular injury occurs during placental abruption, careless cesarean section or embryotomy - an operation to remove the fetus through the birth canal in the event of intrauterine death.
Treatment and prevention
In case of amniotic fluid embolism, a woman needs urgent medical care, which is aimed at eliminating the anaphylactoid reaction. First of all, oxygen therapy is used, which consists of connecting the patient to an artificial respiration apparatus and using oxygen instillations. To normalize hemostasis, blood products, blood replacement fluids, and high doses of glucocorticosteroids are used.
If the above measures lead to a positive result, delivery is possible naturally through the birth canal. If there is no improvement, an urgent caesarean section is required. To prevent amniotic fluid embolism, it is important to avoid conditions that can lead to such a pathology. It is important to visit your doctor in a timely manner to monitor the progress of pregnancy and eliminate uterine hypertonicity. In the case of placental insufficiency and other pathological conditions, it is necessary to take timely measures aimed at preventing embolism.