| Right coronary artery | |
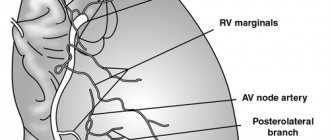
| Blood supply to the heart, with the right coronary artery labeled. | |
| Details | |
| Location | Heart |
| Reserves | right atrium (RA), right ventricle (RV), and 25% to 35% of the left ventricle. |
| Identifiers | |
| Latin | arteria coronaria dextra |
| Acronym(s) | RCA |
| TA98 | A12.2.03.101 |
| TA2 | 4131 |
| F.M.A. | 50039 |
| Anatomical terminology [edit in Wikidata] | |
The blood supply to the heart is the right coronary artery
(
RCA
) is an artery originating above the right cusp of the aortic valve, in the right aortic sinus of the heart. [1] [2] It moves down the right coronary sulcus towards the medulla. [1] [3] It supplies the right side of the heart and the interventricular septum. [2] [4]
Structure [edit]
The right coronary artery originates over the right aortic sinus above the aortic valve. [1] [2] It passes through the right coronary sulcus (right atrioventricular sulcus) towards the medulla. [1] [3] It gives off many branches, including the posterior interventricular artery, right marginal artery, conus artery, and sinoatrial nodal artery. [5]
Segments[edit]
- Proximal: starts from the beginning of the RCA, covers half the distance to the acute edge [6] [7]
- Middle: from the proximal segment to the acute edge [6] [7]
- Distal: From the middle segment to the point of origin of the posterior interventricular artery, where the posterior interventricular groove meets the atrioventricular groove at the base of the heart. [6] [7]
Options [edit]
In approximately 80% of patients (right dominant), the RCA gives off the posterior descending artery (PDA). In the other 20% of cases (left dominant or codominant), the PDA is released from the left circumflex artery or through the right coronary artery and left circumflex artery. [8] The PDA supplies the inferior wall, interventricular septum, and posteromedial papillary muscle.
The RCA also supplies the SA nodal artery in 60% of people. In the remaining 40% of cases, the SA nodal artery is supplied by the left circumflex artery.
Several anomalous courses of the right coronary artery have been described, although rare, including those arising from the left aortic sinus. [9]
Anatomy
The right coronary artery begins in the anterior internal sinus of the aortic bulb. Departing from the anterior surface of the aorta, the PVA is located on the right side of the coronary sulcus, approaches the sharp edge of the heart, goes around it and goes to the intersection and then to the posterior interventricular sulcus. At the intersection of the posterior interventricular and coronary grooves (crossing), the PVA gives off the posterior interventricular branch, which goes to the distal part of the anterior interventricular branch, anastomosing with it. Rarely does PVA end at the sharp edge of the heart.
Function [edit]
The right coronary artery supplies oxygenated blood to the right atrium, right ventricle, and the posterior third and inferior end of the interventricular septum. [2] [4] It can also supply 25% to 35% of the left ventricle (LV). [ citation needed
]
There is significant blockage of supply to the coronary arteries. [2] The right coronary artery is dominant to the left coronary artery 50% of the time, equal to it 20% of the time, and less significant than it 30% of the time. [2]
Coronary angiography
Physiological basis
The first-year university program includes studying the structure of the heart and its coronary vessels. But most often, textbook authors limit themselves to describing only large vessels. Clinicians use a completely different, but also international, nomenclature. Coronary angiography and stent implantation require a more detailed description of the heart vessels, which has found application in international practice.
From the anatomy course, everyone learned that two arteries depart from the aorta that supply blood to the heart itself: the left and right coronary arteries. The thickenings at the root of the aorta, from which these arteries emerge, are called the left and right coronary sinuses, respectively.
The following parts of the left coronary artery (LCA, left coronary artery) are distinguished: main trunk , which is divided into the anterior interventricular branch (ramus interventricularis anterior, RIVA or left anterior descending, LAD), as well as the circumflex artery (left circumflex coronary artery, LCx). The main trunk of this artery rarely exceeds 1 cm in length, and is then divided into its two terminal branches. The anterior interventricular branch is located on the anterior surface of the heart up to its apex. Along its length, the anterior ventricular branches (diagonal branches, RD/R.Diag) and anterior septal branches depart from this artery. In coronary angiography, for the purpose of topical indication of the location of the lesion, it is proposed to divide the coronary bed into segments. The proximal segment of the LAD begins with its branch from the trunk and continues to the point where the first septal or first RD departs from it, the middle part - to the branch of the second septal branch or the second RD, the distal part - to the apex of the heart / after the departure of the second RD.
The circumflex artery is always located on the posterior surface of the heart. In its proximal part, a branch of the obtuse edge (obtuse marginal artery, obtuse marginal branch, OMB) departs from it. Depending on the location of this branch, the proximal and distal parts of the circumflex branch are distinguished. Very rarely, another branch departs from the main trunk between the anterior interventricular branch and the circumflex branch in the middle, originating directly from the common trunk - the intermediate artery (RIM, ramus intermedius).
The following three parts of the right coronary artery (RCA) are distinguished: proximal (from the mouth to its first turn, usually located horizontally), middle (from the first to the second turn) and distal (after its second turn until the artery divides into branches at the “cross” of the heart (crux cordis) - the intersection of the posterior interventricular and atrioventricular grooves of the heart). Sometimes, immediately after the mouth itself, a small branch departs from the vessel - the branch of the conus arteriosus (ramus coni arteriosi, CB), as well as many small branches to the right atrium. The most important of these branches is the artery of the sinoatrial node (SA node artery, SNA). It is often located under the right ear of the heart. In rare cases, the branch of the conus arteriosus has its own orifice. This option should always be considered, since coronary angiography may mistake this artery for the main trunk of the right coronary artery. By blocking the entrance to this artery with a catheter, it is possible to cause local ischemia and, as a consequence, rhythm disturbances up to the flutter of the heart chambers. In the anterior part of the coronary sulcus, in the region of the acute edge of the heart, a branch of the acute edge (acute marginal artery, AMB), usually from one to three, departs from the right coronary artery, usually from one to three, which in most cases reaches the apex of the heart.
So, let's list all the abbreviations again:
Left coronary artery - left coronary artery (LCA): - Anterior interventricular branch (LAD), or anterior descending artery - left anterior descending artery (LAD); otherwise - ramus interventricularis anterior (RIVA/RIA); — Diagonal arteries (branches) — YES; ramus diagonalis (RD/Diag); - Circumflex branch (OB) of the left coronary artery, circumflex artery - left circumflex coronary artery (LCx)); - Branch of the obtuse edge, obtuse marginal artery, obtuse marginal branch, (OMB); - Septal interventricular branches, ramus septalis (RSA); — Intermediate artery, ramus intermedius (RIM).
Right coronary artery - right coronary artery (RCA): - Branch of the acute edge, acute marginal artery, (AMB); - Artery of the sinoatrial node - ramus nodi sinuatrialis (SA node artery, SNASA/RNS); — Posterior interventricular branch (ZMZHV), or posterior descending artery (PDA); otherwise - ramus interventricularis posterior (RIVP/RIP).
And once again for repetition (an important task for diagnosing the localization of ischemia during myocardial infarction): LAD/RIVA , LCx supplies the left chamber with blood from the front and side, and RCA from the back. The left atrium is supplied with blood by LCx, RCA . Partition - RSA from LAD . Right camera at the back - RCA , at the front - RCA, LAD . Right atrium - RCA .
It should also be recalled about the dominance of the blood supply to the myocardium. In the so-called right heart, which occurs in 70% of people, the posterior descending artery (PDA) arises from the right coronary artery. In left-sided hearts (10% of people), the circumflex artery (LCx) reaches the level of the posterior interventricular groove and forms the posterior descending artery (PDA). In the even rarer, so-called mixed codominant type (20% of people), there are two posterior ventricular branches (RIVP/RIP) arising from the right coronary and circumflex arteries.
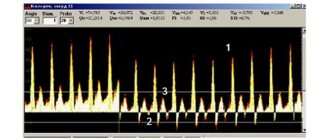
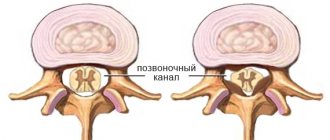
To understand the principle of operation of the ECG, it is necessary to repeat the structure of the conduction system of the heart. The sinoatrial node is located in the wall of the right atrium, its impulses travel to the atrioventricular node (also located in the wall of the right atrium). Next, the impulse propagates along the fibers of the His bundle, which is divided in the interventricular septum into two legs - right and left (sometimes called the legs of Tavara). The signal reaches the endocardium via Purkinje fibers. Sometimes there are additional pathways for the transmission of excitation, as, for example, through Kent fibers. Such pathways are often located between the atria and ventricles and bypass the atrioventricular node. Because of this, the myocardial muscles often contract prematurely, which becomes noticeable on the ECG, and such patients are predisposed to tachycardia (WPW syndrome).
An electrocardiogram is nothing more than a recording of the propagated electrical potentials of the heart, recorded by electrodes on the limbs and chest wall. The ECG includes three standard Einthoven leads (I, II, III), and three enhanced Goldberg leads (aVR, aVL, aVF). Attaching six more chest electrodes according to Wilson (V1-V6) allows you to record the spread of excitation along the heart wall in a horizontal projection. Depending on the changes in these leads, even at the prehospital stage, using an ECG, it is possible to suggest the localization of the infarction and a possible “problem” artery.
For example, with a heart attack of the right side of the heart (the back wall), the right ventricle is often particularly severely affected. Most often this occurs due to a blood clot in the RCA. The right side of the heart is unable to contract properly, resulting in decreased preload of the left chamber of the heart because it reduces the volume of blood transported to the left atrium. The heart tries to compensate for the reduced cardiac output by increasing the contraction rate. With a heart attack of the left side of the heart, the main complication is cardiogenic shock.
Especially for our subscribers, we have made a table that shows ECG changes depending on the location of possible damage to the coronary arteries.
It is also worth repeating the classification of acute coronary syndromes:
- Unstable angina without troponin elevation . This form is classified according to Braunwald into 3 classes depending on the severity of clinical signs:
I - recent chest pain (less than 2 months, more than 3 times a day); II - pain behind the sternum at rest (at least once in the past month, but not within the last 48 hours); III - chest pain at rest (at least once in the last 48 hours). Unstable angina is classified into 3 groups according to the causes of occurrence: A - secondary unstable angina (myocardial infarction, anemia, fever, hypotension, tachyarrhythmia, thyrotoxicosis, respiratory failure); B - primary unstable angina; C - unstable angina after a heart attack (at least 2 weeks after a heart attack).
- Myocardial infarction without ST segment elevation (NSTEMI) with an increase in the concentration of cardiac troponin in the blood.
- ST segment elevation myocardial infarction
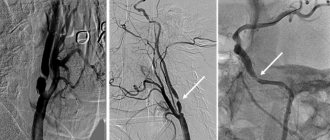
PBCA and stenting
Sones, back in 1959, described a method that allows one to assess the condition of individual coronary vessels. Judkins modified the described method in 1967. It is this method of studying the coronary vessels that is still used today. The first transluminal balloon coronary angioplasty (TBCA) was performed on September 16, 1977 in Zurich in Switzerland. Since then, the number of ACS patients undergoing TBCA has increased from 10 to 65%. According to the latest data, recently published in The Lancet, deaths due to cardiovascular disease in 2010 fell by a quarter compared with 1950, when 400 out of 100,000 cases were fatal. The first patient was a 38-year-old male smoker who presented with LAD stenosis. After the operation, the man lived another 37 years.
With PBCA, a balloon catheter is inserted using a guidewire up to the site of stenosis. The balloon inflates and thereby “flats” atherosclerotic plaques, stretching the vascular wall. Minor intimal injuries during balloon inflation often have no consequences, but sometimes it is in these places that tissue proliferation later begins, which in 30–40% of cases leads to restenosis and relapses over the next three months. The frequency of emergency operations to create bypasses is less than 0.5%. By implanting a stent, the vascular wall is stabilized. There was also a primary stenting technique - implantation of a stent without previous dilatation of the vessels with a balloon, but now it is used extremely rarely and only in the initial stages of narrowing the lumen of the vessel. Studies in recent years have shown that with significant narrowing of the lumen of the vessel, such patients experienced myocardial ischemia in the first hours after angioplasty, which required immediate re-surgical intervention or re-dilatation. This complication occurs due to plaque detachment from the endothelium. Exposure of the surface of smooth muscle cells leads to thrombosis due to the release of collagen molecules and tissue factors that trigger the blood clotting cascade. To avoid the development of blood clots and restenosis, angioplasty is now most often combined with the implantation of stents at the site of stenosis.
The first stent implantation was performed by Sigwart in 1987. Then the stents were mounted directly on the balloon by the doctor himself. Now the entire structure is included, which has reduced the risk of stent loss in the bloodstream if it is not sufficiently fixed.
Links[edit]
- ^ abcd Aggeli, Konstantina; Mavrogeni, Sofia; Tousoulis, Dimitris (2018-01-01), Tousoulis, Dimitris (ed.), "Chapter 3.5.1 - Noninvasive Imaging Techniques in Coronary Artery Disease", Coronary Artery Disease
, Academic Press, pp. 337–358, doi: 10.1016 / b978-0-12-811908-2.00017-9, ISBN 978-0-12-811908-2, access date 11/20/2020 - ^ abcdef Pappano, Achilles J.; Gil Wier, Withrow (01/01/2013), Pappano, Achilles J.; Geer Wie, Withrow (eds.), "11 - Coronary Circulation", Cardiovascular Physiology (tenth edition)
, Philadelphia: Elsevier, pp. 223-236. DOI: 10.1016/b978-0-323-08697-4.00011-3, ISBN 978-0-323-08697-4, accessed November 20, 2020 - ^ ab Sivananthan, M. (2018-01-01), "Coronary Anatomy", in Vasan, Ramachandran S.; Sawyer, Douglas W. (ed.), Encyclopedia of Cardiovascular Research and Medicine
, Oxford: Elsevier, pp. 691-699. DOI: 10.1016/b978-0-12-809657-4.99738-2, ISBN 978-0-12-805154-2, accessed November 20, 2020 - ^ ab Schipper, Paul; Sukumar, Mithran; Mayberry, John C. (2008-01-01), Asensio, JUAN A.; TRUNKEY, DONALD D. (ed.), Relevant Surgical Anatomy of the Thorax and Mediastinum, Current Therapy of Trauma and Surgical Critical Care
, Philadelphia: Mosby, pp. 227–251, doi: 10.1016/b978-0-323-04418-9.50037-0, ISBN 978-0-323-04418-9, accessed November 20, 2020 - Antonopoulos, Alexios S.; Sias, Gerasim; Antoniades, Charalambos; Tousoulis, Dimitris (2018-01-01), Tousoulis, Dimitris (ed.), "Chapter 2.1 - Functional Anatomy", Coronary Artery Disease
, Academic Press, pp. 121–126, doi:10.1016/b978-0-12- 811908-2.00008-8, ISBN 978-0-12-811908-2, access date 11/20/2020 - ^ abc Villa, AD; Sammut, E; Nair, A; Rajani, R. Bonamini, R; Chiribiri, A (28 June 2021). "Overview of Coronary Artery Anomalies: Normal and Abnormal". World Journal of Radiology
.
8
(6): 537–55. DOI: 10.4329/wjr.v8.i6.537. PMC 4919754. PMID 27358682. - ^ a b c Keeney, S; Bis, K. G.; Weaver, L. (June 2007). "Normal and variant anatomy of the coronary arteries and veins on high-resolution CT angiography." A.J.R. American Journal of Radiology
.
188
(6):1665–74. DOI: 10.2214/AJR.06.1295. PMID 17515392. - Shahood, James S.; Ambalavanan, Manoj; Thivakaran, Vijay S. (2020). Cardiac predominance. StatPearls Publishing. PMID 30725892.
- Angelini, P. (July 15, 2014). "New imaging of coronary artery anomalies to assess their prevalence, causes of clinical symptoms, and risk of sudden cardiac death". Circulation: Cardiovascular Imaging
.
7
(4):747–754. DOI: 10.1161/CIRCIMAGING.113.000278. PMID 25027456.