In addition to varicose veins, there are a number of other diseases that can cause narrowing of the blood vessels in the legs. As a result, the vessels can narrow to a critical point and stop carrying nutrients to the tissues.
To restore normal blood flow, a phlebologist surgeon performs vascular bypass surgery. A shunt (part of a vessel) is inserted to bypass the damaged section of the vein, allowing blood flow to normalize in the tissue and return them to the necessary nutrition.
The method of shunt insertion depends on the area of vessel damage. Areas of vein damage:
- Femoral part. An incision is made in the groin area, the edge of the shunt is installed in the abdominal aorta, the second part of the shunt is approached to a healthy section of the vein on the thigh.
- Thigh and popliteal part. In this case, the groin area and the back of the knee are cut. The shunt connects a healthy vein in the thigh and an artery running under the knee.
- Femoral-tibial region. Here, one’s own vein is used by connecting the great saphenous vein to the arterial bloodstream. To do this, make a small incision in the groin and lower leg area.
- Method of floor bypass. If in the affected area all vessels have partial blood flow. Then the doctor, to normalize blood flow, introduces a shunt into healthy areas of several veins.
- Foot area. It is carried out to restore blood circulation to the toes. A portion of the great saphenous vein is used as a shunt.
There are two types of shunts:
- Biological (natural) shunts. The biological shunt is very durable: it can restrain the flow of arterial blood. In medicine, the introduction of a biological shunt is often carried out, since the native tissues of the body take root better. The material for making the shunt is taken from the patient's saphenous femoral veins.
- Mechanical or synthetic shunts. Used for extensive vascular lesions. Made from safe polymers. Used in bypass surgery of large vessels.
General information
Coronary artery bypass grafting is a surgical intervention during which a bypass route for blood supply to a certain area of the myocardium is created. Bypass surgery allows you to completely restore nutrition to the myocardium when the coronary artery is narrowed. The own veins of the leg or the radial artery are used as a shunt. Surgery can reduce the severity of coronary heart disease and improve the patient’s quality of life.
What is cardiac bypass surgery after a heart attack?
to stop the spread of myocardial infarction when it develops by performing cardiac bypass surgery within 6-15 hours after the cardiovascular event. Technically, the intervention is carried out in a standard manner, taking into account some features:
- execution as early as possible;
- aortocoronary connection recommended;
- access through the sternum on an idle heart and artificial circulation.
Where is vascular bypass performed?
Vascular bypass is an effective way to restore blood flow after advanced forms of varicose veins. If you have already been diagnosed with a severe form of varicose veins or you want to undergo vein diagnostics, then make an appointment at the Phlebological Center named after. Pirogov. Our doctors will help you restore blood circulation in the veins of your legs.
We are located at the address: Moscow, Gagarinsky Lane, 37/8 (metro station “Smolenskaya”, Arbatsko-Pokrovskaya line, metro station “Kropotkinskaya”).
We are open for you from Monday to Friday from 8:00 to 21:00, Saturday and Sunday from 9:00 to 18:00. Call +7.
Back to articles
Classification
Surgeons use various compounds depending on the location of the affected vessels and their number:
- coronary artery bypass grafting - connection to the aorta;
- mammacoronary bypass surgery - connection to the thoracic artery.
The difference between shunts is that they receive power from different vessels: from the internal mammary artery and the aorta.
Coronary artery bypass graft
A vessel is isolated from an arm or leg and connected to the aorta. The second end is sutured below the area of the narrowed coronary artery. This makes it possible to provide nutrition to the affected area of the myocardium directly from the aorta, which has a positive effect on metabolic processes in the myocardium and ensures its normal functioning. The patient's tolerance to physical activity improves and the severity of pain decreases.
Mammarocoronary bypass
A mammary coronary bypass connects the mammary (thoracic) arteries and the coronary vessels of the heart damaged by atherosclerosis. The anatomy of the location of the vessels makes it possible to connect the left internal thoracic artery with the left coronary artery, and the right one with the right coronary or interventricular artery.
Bimammary bypass surgery
It is performed for widespread damage to the coronary vessels. Surgical intervention is recommended if previously performed CABG is ineffective, with vein thrombosis (impossibility of using them), narrowing and blockage of the shunt, and narrowing of the radial arteries. Advantages of this method:
- wall strength;
- resistance to the formation of cholesterol plaques and blood clots;
- wide lumen of the thoracic artery.
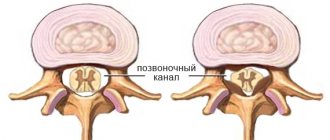
Minimally invasive coronary artery bypass grafting
Access to the coronary arteries is obtained through a small incision in the intercostal space to the left of the sternum. The chest is not opened. Healing occurs much faster, and the operation is considered less traumatic. The surgical intervention is performed without connection to a heart-lung machine, on a beating heart. Minimally invasive surgery is performed when 1 or 2 coronary branches on the anterior wall of the left ventricle are damaged. A significant drawback of this method is the inability to ensure complete restoration of coronary blood flow.
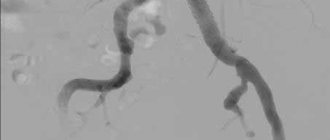
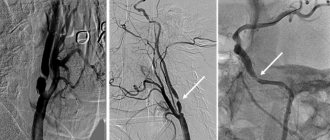
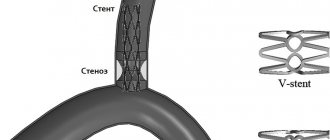
Coronary stenting of heart vessels
It is considered a gentle, minimally invasive, intravascular operation on the vessels of the heart, which consists of widening a narrowed artery by straightening the inserted stent. Stenting is usually carried out immediately after coronary angiography , which makes it possible to determine the extent of damage to the coronary artery and select the stent required in diameter and length.
Technique for stenting coronary arteries (with professional jargon)
“We install the introducer”
To get to the heart vessels, the doctor needs to get into the patient’s arterial system. For this purpose, one of the peripheral arteries is used - the femoral (in the groin) or the radial (on the forearm). Under local anesthesia, a puncture is made in the artery and an introducer is installed - a special tube, which is the “entry gate” for all the necessary instruments.
"Let's put a guide"
Then a special thin-walled tube about a meter long - a guiding catheter (“guide”) is passed through the patient’s arteries and stops, slightly short of the heart, in the aorta. It is from the aorta that the coronary arteries that supply the heart depart. The tips of the catheters are curved in such a way that it is convenient for the doctor to enter one of the coronary arteries, right or left. By controlling the catheter, the doctor “enters” one of the coronary arteries. Half the job is done.
“Starting a conductor”
But how to get to the point of maximum narrowing in the artery? To do this, we need a “rail” along which all our tools will “ride”. This rail is the coronary guidewire - a thin (0.014 inch = 0.35 mm) metal “lint” with a soft tip (so as not to “scratch” the artery during the operation). Sometimes it is quite difficult to place a guidewire behind the site of narrowing; the tortuosity of the artery, the angle of departure of the branches of the artery, or pronounced narrowing due to the presence of plaques interfere. You can take a “harder” or “slipperier” conductor. Well, or just a favorite, because every doctor has his own preferences. One way or another, the guide ends up behind the site of narrowing on the periphery of the artery that we want to stent.
"Ballooning"
The first instrument that gets to the site of narrowing of the artery is a coronary balloon with a diameter most often from 1 to 3.5 mm and a length of 10-20 mm. The balloon is put on the conductor and moves along it to the point of maximum narrowing where it inflates. The pressure inside the cylinder reaches 15-20 A
Next, along the conductor, to the place that was narrowed before the balloon was inflated, the same balloon is inserted, on the surface of which a stent is fixed in a folded state. The balloon is inflated, the stent is expanded and “pressed” into the artery wall. The stent does not always expand perfectly and then the final stage of the procedure is needed - postdilatation (in simple terms - re-inflation).
"Let's blow it out"
A rigid balloon is placed inside the implanted stent and inflated with high pressure (up to 25 atmospheres). Most often, after this, the stent straightens and adheres well to the walls of the artery.
Causes
CABG improves coronary blood flow, which reduces the severity of pain and reduces the number of angina attacks. After surgery, patients can better tolerate physical activity, improve performance, and improve their psychological state. Surgeries to reconstruct the cardiac vasculature reduce the risk of myocardial infarction .
Indications for shunt installation:
- critical narrowing of the coronary arteries;
- angina pectoris grade 3 and 4 (attacks occur during normal physical activity and at rest);
- aneurysm due to coronary sclerosis ;
- inability to perform stenting;
- narrowing of the coronary arteries in combination with post-infarction aneurysm and structural defects of the heart .
Preoperative preparation
Before surgery, a complete examination of all vascular beds is necessary. If ulcers or erosions of the stomach are detected, preliminary treatment is carried out. The oral cavity must be sanitized. Clarification of the picture of vascular damage is achieved using computed angiography (MSCT). If significant lesions of the carotid or coronary arteries are identified, the issue of preferential revascularization of these areas before surgery on the aorta is decided. Before surgery, it is necessary to correct all existing disturbances in protein and electrolyte metabolism and increase the level of hemoglobin in the blood. On the eve of the operation, it is necessary to cleanse the intestines with a special preparation and enemas. Dinner the night before surgery should be very light. The surgical field (abdomen, thighs) is carefully removed from hair. The patient is given sedatives to relieve anxiety before surgery.
Symptoms
After surgery, patients are admitted to the intensive care unit, where urinary tract catheterization and artificial ventilation are performed. Painkillers are administered and antibiotics . Heart function is assessed on a monitor in the form of electrocardiography. After stabilization of the patient’s condition, the patient is transferred to independent feeding and breathing. The range of movements increases gradually, step by step.
At first, patients are bothered by chest pain, which is due to the specifics of the operation being performed, because it is open to the public. As the sternum grows together, the pain subsides. Also, discomfort is observed in the area where the vein was taken. All symptoms are temporary and the patient gradually returns to his usual lifestyle.
When is stenting performed?
Stenting is done when the lumen of the arteries is narrowed by more than half. This is an effective operation that is performed even in the presence of concomitant chronic diseases and infectious processes in the body. Initially, when deciding on surgical intervention, the question of stenting is almost always raised. If it cannot be done, then bypass surgery is performed.
Tests and diagnostics
Complete information about the state of the vascular system of the heart is obtained after coronary angiography and multislice computed tomography. Both research methods make it possible to assess the degree of damage to the coronary vessels and determine further treatment tactics.
MRI of the heart and coronary vessels
Magnetic resonance imaging is considered a non-invasive diagnostic test, which is based on the nuclear magnetic resonance method. MSCT allows you to obtain a clear image of the heart and assess the condition of the coronary vessels. Absolute contraindications:
- the presence of clamps, staples and metal implants;
- the presence of an insulin pump, pacemaker, ferramagnetic implant and other electronic systems.
The price of the study ranges from 15 to 35 thousand rubles. Compared to the magnetic resonance imaging method, cardiac CT is more informative in terms of assessing the condition of the vascular system of the heart.
Additional examination methods:
- coagulogram;
- biochemical and general blood test;
- Ultrasound of the abdominal organs;
- lipid spectrum;
- chest x-ray;
- Ultrasound scanning of the lower extremities;
- ECG;
- EchoCG;
- Analysis of urine.
Progress of aortofemoral bypass surgery
In our clinic, the preferred surgical approach is the Rob retroperitoneal incision; it has significant advantages compared to traditional laparotomy (access through the abdominal cavity). With the Rob approach, the lumbar nerves are not damaged and the intestines are not injured. This allows patients to begin feeding the very next day after surgery, and within a day they can already get out of bed.
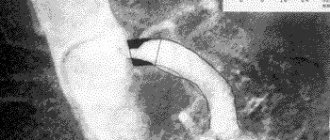
After isolating the abdominal aorta, the degree of its damage by the atherosclerotic process is assessed. The operation involves isolating the aorta above the lesion through an incision on the side wall of the abdomen and the femoral arteries in the upper thighs. An artificial vessel made of an inert plastic material that does not cause a reaction in the surrounding tissue is sewn into a plaque-free area of the aorta. Then the branches of this vascular prosthesis are brought out to the femoral arteries and sutured into lesion-free areas. In this way, the blocked area is bypassed and the blood easily enters the legs.
Treatment
Drug therapy is aimed at:
- maintaining normal blood pressure and pulse levels;
- prevention of thrombosis;
- lowering cholesterol , leveling the lipid spectrum;
- improvement of trophism and nutrition of the heart muscle.
Medicines
The main drugs prescribed after stenting and bypass surgery:
- Brilinta;
- Plavix;
- Bisoprolol;
- Lisinopril;
- ThromboASS;
- Atorvastatin;
- Preducted.
Rehabilitation
The recovery period is long. You cannot wash for two weeks after bypass surgery, as the wounds are extensive and there is a risk of secondary infection. Daily dressings, treatment with antiseptics. You will need to wear a chest bandage for six months to prevent the stitches on your sternum from coming apart.
Average rehabilitation is about three months. During this period, blood and blood flow will normalize, and the sternum will heal. An assessment test for the possibility of a full life is a stress test (for example, bicycle ergometry).
Prevention and rehabilitation after heart surgery
Surgical intervention does not eliminate the true cause of the disease - atherosclerotic changes in blood vessels, but only eliminates the consequences. For prevention, a change in diet and lifestyle is recommended. The rehabilitation period is somewhat different after bypass surgery and after stenting of the coronary vessels.
Coronary artery bypass surgery, basic recommendations for the prevention of complications after surgery and for a speedy recovery in the postoperative period:
- complete cessation of smoking and consumption of alcohol-containing products;
- dietary food with a reduced content of animal fats;
- maintaining normal blood pressure numbers;
- gradual increase in physical activity;
- wearing special compression hosiery (tights, stockings);
- control over heart rate;
- preventive drug therapy;
- daily walks in the fresh air;
- regular monitoring by your doctor.
Basic recommendations that must be followed immediately after CABG surgery:
- daily walking for at least 20 minutes with a gradual increase in duration to 1 hour;
- take time for breathing exercises, meditation and complete relaxation of the body;
- gradual loss of excess weight due to nutritional correction and moderate physical activity;
- replace meat products (lamb, pork, duck) with fish;
- completely eliminate offal, butter meat and fried foods;
- reduce salt intake;
- replace baked goods and sweets with honey and dried fruits;
- fight excess weight.
After heart bypass surgery, do gymnastics yourself at home, avoiding excessive overload and lifting weights. Light exercises after CABG help keep the back muscles in good shape.
After stenting the heart vessels, there are slightly fewer restrictions, due to the fact that the chest is not opened, which allows patients from the first days to gradually increase physical activity and train the heart muscle, without allowing it to relax and become lazy. Bypass surgery involves a longer recovery period.
Features of the operation at the Innovative Vascular Center
Although aortobifemoral bypass surgery is one of the most common vascular operations and is performed in many vascular departments, our clinic uses certain approaches to improve the immediate and long-term results of the operation, especially in complex cases.
The main problem when performing ABBG remains the traumatic approach and associated early postoperative problems. In our clinic, a retroperitoneal approach is used to perform aortofemoral bypass surgery, without opening the abdominal cavity. This allows operations to be performed under epidural anesthesia without general anesthesia and ensures a comfortable postoperative period.
To perform repeated operations on the aorta in case of suppuration of vascular prostheses or thrombosis, our surgeons can use access to the thoracic aorta using an extended left-sided lateral approach. This approach made it possible to perform operations on patients who were refused by all other clinics.
Another important feature of surgical treatment in our clinic is the possibility of angiography during surgery. We definitely conduct a contrast study after aortofemoral bypass surgery in order to assess the hemodynamic correctness of the vascular reconstruction and identify possible problems. This approach increases the possibility of performing the operation and improves immediate results.
The use of intraoperative angiography makes it possible to operate on patients with severe calcification of the abdominal aorta, which does not allow the use of conventional methods of vessel clamping. To control bleeding, we use inflating a special balloon in the aorta, which allows us to block the blood flow while the vascular graft is sutured to the aorta. The balloon is passed through an access on the arm. The same technique allows us to successfully operate on ruptured abdominal aortic aneurysms.
The results of aortofemoral bypass surgery in our clinic are very good. Treatment success is achieved in 97% of patients with damage to the aortoiliac segment.
Diet after bypass surgery
The main factor that negatively affects the condition of the vascular wall and blood supply to the myocardium is excessive cholesterol in the blood. This is why it is so important to give up animal fats and diversify your diet with foods that remove cholesterol from the body and prevent its deposition on the walls of blood vessels.
The diet should contain sufficient quantities of vegetables, herbs, fish dishes, and chicken without fat. It is better to choose dairy products with a reduced fat content. It is recommended to consume vegetable oil as a source of fat - 2 tablespoons per day.
Pain relief during aortofemoral bypass surgery
In our clinic, surgery is usually performed under epidural anesthesia. A special catheter is installed in the back, through which an anesthetic drug is supplied. Complete pain relief and muscle relaxation for retroperitoneal access are achieved. For the purpose of sedation (calming), the patient is given mild sedatives. During operations on the thoracic aorta, general anesthesia is used. The anesthesiologist continuously monitors blood pressure and oxygen saturation. For adequate administration of drugs, a subclavian venous catheter is installed in the patient. The bladder is drained with a catheter to monitor kidney function.
Consequences and complications
Complications can develop if the patient has concomitant pathology:
- diabetes;
- pathology of the renal system;
- diseases of the pulmonary system.
Most often, after surgery, bleeding occurs in the anastomotic area and rhythm disturbances are recorded. Possible complications:
- acute circulatory disorder in the brain and myocardium;
- thrombosis of the venous bed;
- renal failure;
- local complications in the form of wound infection and the formation of postoperative keloid scars;
- closure or narrowing of the shunt.
Preparation for coronary artery bypass surgery
At the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, before performing coronary artery bypass surgery, the doctor draws up a preoperative examination plan. It includes laboratory tests and instrumental studies:
- general blood test, urine test;
- blood biochemistry;
- expanded coagulogram;
- ADP platelet aggregation;
- blood type and Rh factor;
- markers of infections: HIV, hepatitis B, hepatitis C, syphilis;
- Pro-BNP, SRP;
- ECG;
- Echo-CG;
- X-ray examination;
- EGDS (maximum duration – 1 month). An exception is patients with lesions of the left artery trunk;
- Ultrasound scanning of the brachiocephalic arteries (maximum duration – 3 months);
- Ultrasound scanning of the arteries of the lower extremities (maximum duration – 3 months);
- Ultrasound scanning of the veins of the lower extremities (maximum duration – 7 days);
- FVD (maximum duration – 7 days);
- Ultrasound of internal organs;
- coronary angiography.
If there is a concomitant pathology, additional tests may be prescribed:
- History of stroke - CT scan of the brain.
- thyroid diseases - TSH, T4, T3 (maximum duration - 30 days). Consult an endocrinologist if there are changes in the hormonal profile.
- diabetes mellitus - glycemic curve (maximum duration - 7 days). Consultation with an endocrinologist for glycemia more than 10 mmol/l.
- Gout - uric acid (maximum duration - 1 month). If the value exceeds 420 µmol/l, consult a therapist and select therapy.
- consultation with a dentist, urologist, gynecologist.
The day before surgery, the patient is examined by a surgeon and an anesthesiologist. On the eve of CABG, it is recommended to have a light dinner no later than 12 hours before surgery, not to eat or drink the night before, and to stop taking medications. A cleansing enema is given at night. In the morning the patient takes a shower.
After signing the informed consent, the patient is given premedication - medications are administered that will reduce emotional tension and help calm down. After 40-60 minutes, the patient is taken to the operating room.
At the cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, you can take all the tests and undergo studies recommended by your doctor before the operation. The structure of our center allows you to quickly go through the preparatory preoperative stage and get the results in hand. Having our own laboratory, we are responsible for the accuracy of tests and the quality of clinical and laboratory studies.
Prediction of how long you can live after surgery
If blood flow in the coronary arteries is completely restored after coronary bypass surgery and the patient takes all prescribed therapy, then the prognosis is considered favorable.
Restoring adequate blood supply to the myocardium can relieve the patient from pain associated with myocardial ischemia, reduce the number of angina attacks, and improve exercise tolerance.
Long-term results of surgical intervention:
- restoration of working capacity;
- reducing the risk of developing myocardial infarction;
- reducing the risk of sudden death from acute coronary syndrome;
- improving exercise tolerance;
- increase in life expectancy;
- medications are taken only for prophylactic purposes.
How long do you live after heart bypass surgery?
The average lifespan of a shunt is 10 years. To assess the viability of the shunt, coronary angiography is performed, based on the results of which a decision is made on the need for repeated surgical treatment. A full course of rehabilitation after cardiac surgery allows you to maximize the service life of the installed shunt.
Reviews from patients who have undergone bypass surgery are mostly positive. After the operation, the heart undergoes remodeling; during this period, patients note a deterioration in their health, and it seems to them that the operation was unsuccessful. However, after a while, after a complete restructuring of the blood supply to the myocardium, the patients’ well-being significantly improves, exercise tolerance increases, and chest pain goes away. In the long term, reviews are mostly positive.
A gentle surgical option to restore adequate blood supply to the myocardium is cardiac stenting. The essence of the operation is to insert a special stent into the coronary vessel, which, after deployment, completely opens the lumen of the affected artery and restores blood flow. The rehabilitation period after stenting surgery is much shorter than with bypass surgery, because The intervention is not performed on an open heart, but a stent is inserted through the groin or through the arm.
Contraindications
Coronary artery bypass grafting (CABG) may not be performed on patients even if there are indications for surgery. This may be due to the presence of contraindications. These are diseases and conditions of the body that make surgery too dangerous or unsuccessful.
Main contraindications for cardiac CABG:
- Reduced left ventricular ejection fraction by up to 30%
- Congestive heart failure
- Impaired blood flow in all coronary arteries
- Severe concomitant diseases
In case of circulatory disorders in all coronary arteries, preference is given to laser myocardial revascularization or cell therapy.
Indications for surgical treatment of coronary vessels
Coronary artery bypass surgery - the formation of bypass blood flow in stenotic vessels - is performed according to specific indications:
- narrowing of the left coronary artery by more than 50%;
- resistance to therapeutic methods for treating angina pectoris;
- violation of myocardial contraction;
- extensive area of ischemia;
- atherosclerotic damage to several vessels;
- arterial damage in patients with concomitant pathologies;
- narrowing of coronary vessels more than 70%.
Risks of using an IR device
Vascular bypass with open access and cardiac arrest is associated with the risk of developing the following complications:
- possibility of bleeding;
- necrosis of a portion of the heart muscle;
- incomplete fusion of the thoracic incision;
- renal failure;
- venous thromboembolism;
- cerebral artery stroke;
- amnesia (memory loss);
- large scars on the chest;
- pronounced pain symptom.
After the operation, until the postoperative wound has completely healed, you should not take a bath, use gels, or rub in the suture area. You should not take a hot shower or use lotions.
Price
Since 2021, coronary artery bypass surgery is included in the system of state guarantees, that is, it is carried out under the compulsory medical insurance policy. The condition is a primary referral from a local doctor. Surgical intervention is performed in all government medical organizations at the appropriate level. If it is not possible to perform CABG at the regional level, referrals to federal medical centers are used.
If a patient wants to undergo coronary artery bypass surgery in a specific private clinic or abroad, he is not entitled to compensation for treatment. The average cost of an operation in Moscow is 120,000 rubles, St. Petersburg – 85,000 rubles, Kazan – 32,500 rubles.
Let us emphasize once again that bypass surgery is performed on an open heart, which requires special equipment, highly qualified doctors and a specialized hospital.
Heart bypass surgery in German clinics: examination plan
The study of the functional state of the myocardium consists of the following procedures:
- examination by a cardiac surgeon (drawing up treatment tactics, explaining the essence of the operation);
- electrocardiographic (ECG) recording of heart condition;
- determination of heart function under load conditions (ECG recording after bicycle ergometry);
- daily monitoring of myocardial function (Holter monitoring);
- Ultrasound of the heart;
- Doppler examination of peripheral vessels;
- 24-hour blood pressure monitoring.
Then coronary angiography is performed, which determines the condition of each vessel of the heart muscle. In German clinics, coronary angiography is most often performed with simultaneous vascular bypass surgery. In Russia, these manipulations are carried out sequentially, which requires repeated surgical intervention on the body.
Coronary angiography is performed by inserting a plastic tube with a camera into the damaged vessel. The level of patency of the coronary artery is visually determined on the monitor. The procedure can be performed with simultaneous medical manipulations. Detection of ischemic myocardial disease is an indication for heart bypass surgery.