Early postoperative period
Wound care. Typically, postoperative sutures do not require removal, and the wound does not require special care. The doctor may recommend that you treat the wound with brilliant green for several days, in most cases this is enough. However, you need to protect the wound from injury, avoid rubbing the wound with clothing, and avoid hypothermia.
Shower. If sutures are not required or are removed, you can shower. Hot showers are not recommended. The wound is washed with warm water without using a washcloth. After washing, you need to blot the wound area with a towel, do not rub! After the wound has dried, you can treat it with brilliant green.
Mode. During the first month after surgery, a gentle regime is necessary. The wound must heal, and the body “get used” to the new features of the blood supply. Therefore, physical activity, baths, saunas, hypothermia are not recommended, and alcohol intake should be completely avoided.
Medicines. After the operation, you will be prescribed medications. Strictly follow the regimen and dosage. More information about medications will be discussed below.
Low blood pressure - is there a danger?
Experts are sure that low blood pressure adversely affects the general condition of the body. A person may experience dizziness, weakness, heaviness in the legs, frequent fatigue and “fogginess” in the head. However, this condition rarely turns out to be dangerous for the activity of a relatively healthy cardiovascular system.
Doctors recommend starting to worry only if hypotension systematically manifests against the background of the development of other heart diseases. In this case, the effect of low pressure on the heart is more likely.
According to cardiologists, a permanent (constant) state of hypotension in the presence of a diagnosed pathological condition of the heart can have a negative impact on the development of existing heart diseases, which include an enlargement of one of the ventricles of the heart, uneven stretching of a muscular organ, etc.
What to do to avoid repeated operations?
Most people know what a healthy lifestyle is, that smoking, overeating and lack of exercise are harmful to health. Following simple rules (see the article “Prevention of Atherosclerosis”), which should become a habit, will help not only to avoid repeated operations, but to maintain health for many years.
Lifestyle
An active lifestyle is very important, not only for the prevention of atherosclerosis, but for maintaining health in general.
It is important for post-surgery patients to choose the right type of exercise. This is primarily walking, doing housework, gardening, or climbing stairs. You can work out in the gym (physical therapy), swim. But it is important to remember that exercise associated with heavy sweating (when you sweat a lot) is undesirable. If they are unavoidable, always keep a water bottle with you.
Diet
It is necessary to form the habit of healthy eating. Changing your diet is essential to normalize your weight and reduce your cholesterol levels, which play a huge role in plaque formation.
Medications
Taking medications after arterial surgery is extremely important. This should become a daily habit. In order not to forget to take a pill, you can use, for example, a reminder on your phone.
The main medications that need to be taken after artery surgery are “blood-thinning” drugs (antiplatelet agents and anticoagulants). Taking these medications will help avoid thrombosis of the reconstruction area. Therefore, strictly follow the dosage regimen and dosage. Under no circumstances should you stop taking these medications on your own. However, taking “blood-thinning” drugs can provoke various bleedings (nasal bleeding, menstrual bleeding, bleeding gums, spontaneous formation of hematomas, and so on). If signs of bleeding appear, you should immediately consult a doctor. If you see another doctor, such as a dentist or gynecologist, be warned about taking “blood-thinning” medications.
To prevent further development of atherosclerosis, drugs are prescribed to lower cholesterol levels ().
Bath, sauna
The steam room is not recommended for patients after arterial surgery, especially in combination with alcohol. The fact is that in the steam room a person sweats and loses a lot of fluid, which leads to “thickening” of the blood and can provoke the formation of a blood clot, especially in the operation area. The same applies to any situations in which increased sweating occurs (physical activity, hot weather, etc.). If such situations are unavoidable, always keep a water bottle with you.
Alcohol
Excessive alcohol consumption is a risk factor for the development of thrombosis of various locations, even in a healthy person. As for the patient after arterial surgery, alcohol abuse greatly increases the risk of developing thrombosis of the arterial reconstruction zone. Most patients with atherosclerosis after artery surgery completely refuse to drink alcoholic beverages.
Visit doctor
Regular visits to the doctor and additional research methods (blood tests, ultrasound, etc.) will help avoid unfavorable situations.
Don't neglect your health.
Visit your doctor regularly and follow all his recommendations.
Memo to a patient who has undergone coronary artery stenting
Atherosclerosis is a chronic progressive disease that leads to a decrease in blood flow in the supply area of the artery and oxygen starvation (ischemia) of the organ. Therefore, this disease is called coronary artery disease. If the coronary artery is narrowed, then symptoms of angina pectoris occur; if its lumen is completely blocked, then myocardial infarction occurs. This disease affects a large number of people around the world, incl. in our country. IHD is a leading cause of disability and death. Therefore, treatment of atherosclerosis and coronary heart disease is extremely necessary.
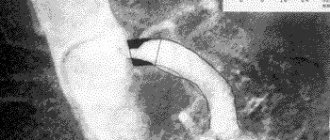
Damage to the coronary arteries can be suspected if characteristic chest pain appears during physical activity, changes during ECG and echocardiography. The most informative method for diagnosing damage to the arteries of the heart is coronary angiography. This study is carried out by puncturing the femoral or radial artery, passing a catheter through the hole to the vessels of the heart and injecting a contrast agent, one at a time, first into the right one. Then into the left coronary artery. The injected X-ray contrast agent, mixing with the blood, flows through the vessels, and at this time the X-ray machine is turned on and records the image in movie mode. After recording the entire series of images, the catheter is removed and the puncture site is pressed to stop bleeding. By assessing changes in the arteries, the X-ray endovascular surgeon can reliably say which treatment tactics can improve the patient’s quality of life - further drug therapy or invasive intervention (angioplasty with stenting or coronary artery bypass grafting).
Angioplasty and stenting of the heart arteries is currently the leading and most effective method of treating coronary heart disease due to a number of advantages:
- access does not require tissue incision and, accordingly, general anesthesia and associated complications;
- the patient communicates freely with the doctor during the entire procedure and usually does not experience any pain;
- The operation itself does not last long, and after it the person must remain in bed for 24 hours, and after a few days he can be discharged for outpatient treatment.
- This intervention can be performed several times throughout life as the disease progresses.
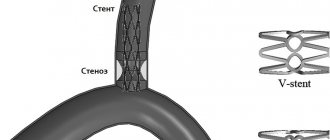
The essence of the technique is to expand the narrowed lumen of the vessel from the inside
a special balloon catheter, which is brought directly to the atherosclerotic plaque. By inflating a balloon selected to the size of the affected segment of the vessel, the plaque is crushed and the lumen of the artery is restored. To ensure that the artery segment remains dilated as long as possible, the arteries are strengthened by installing a special metal mesh tubular frame - a stent.
IMPORTANT! The effect of the intervention depends not only on what and how the stent is installed, but also on the patient’s further compliance with the following rules:
1. Strict blood pressure control
2. Quitting bad habits - smoking and alcohol
3. Regular exercise
With physical activity, blood supply to all organs and systems improves, the emotional state improves, weight decreases, and postoperative recovery accelerates.
4. Compliance with the principles of rational nutrition
- Limiting salt to 3-5 g/day (1 level teaspoon)
- Limiting animal fats (sour cream, fatty meats, poultry)
- Adequate dietary fiber intake
- Limiting cholesterol (offal, egg yolk)
- Consumption of vegetable oils (sunflower, olive, corn) - sources of omega-3 fatty acids
5. Learn to resist stress, avoid conflict situations and not create them
6. Strictly follow all prescriptions and recommendations of the doctor - regularly take medications and undergo prescribed examinations.
IMPORTANT! After stenting, the first step is to take medications that prevent the formation of blood clots: aspirin 75-100 mg/day. for life and clopidogrel 75 mg/day. at least 12 months.
IMPORTANT! You should also take statins, which significantly reduce mortality and the incidence of complications of coronary heart disease. In this case, the target values should be:
- total cholesterol less than 4.5 mmol\l
- low density lipoproteins less than 2.5 mmol/l
If symptoms of angina pectoris return, you should immediately consult a doctor.
It must be remembered that by strictly adhering to the recommendations, you can be sure of improving your quality of life for a long time.
Developed by the head of the RCC of the Central region Bolshovaya E.V.
Antiarrhythmic therapy before and after invasive treatments for atrial fibrillation.
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
- Tarasov Alexey Vladimirovich. "Antiarrhythmic therapy before and after invasive treatments for atrial fibrillation."
Alexey Vladimirovich Tarasov , Candidate of Medical Sciences:
– Good afternoon, dear colleagues. I want to discuss a very interesting, very relevant issue - management tactics before and after various invasive methods of treating atrial fibrillation. Today, the point of application of radiofrequency ablation for the treatment of atrial fibrillation is being discussed at all international Russian sites. But for some reason they very much forget how to manage patients after radiofrequency ablation, although there are more and more such patients. And sometimes we don’t know how to do this, what to do with these patients, because a number of quite serious debatable questions arise and even sometimes anti-advertising questions, because patients come after, for example, isolation of the mouth of the pulmonary veins, but with a number of unanswered questions. And how to conduct them, what we have today, what our experience is, I will try to present to you.
Today, the treatment of paroxysmal atrial fibrillation is, of course, antiarrhythmic therapy and some invasive treatment methods. The main invasive treatment for atrial fibrillation is catheter radiofrequency ablation of the pulmonary veins. Basically, antral ablation of the mouth of the pulmonary veins is now performed. The main indication for radiofrequency ablation of the pulmonary vein ostium is symptomatic paroxysmal atrial fibrillation that is resistant to at least two antiarrhythmic drugs. Currently, it is being discussed whether to use one antiarrhythmic drug or at least two antiarrhythmic drugs. But for now, you should give your patient at least two antiarrhythmic drugs; if they do not work, only then decide on the treatment of atrial fibrillation using the catheter ablation method.
It is also very important to note that such patients should be without organic pathology of the heart, because patients with organic pathology of the heart have other mechanisms, not necessarily ectopy from the mouths of the pulmonary veins, processes in the atrial tissue are already involved here, and in such patients radiofrequency ablation will either ineffective, or 50/50.
What do we have after radiofrequency ablation? The postoperative period can be divided into three periods. The first period is three months, called the early postoperative period, some call it the blind postoperative period. This is the most problematic period because both recurrences of old atrial fibrillation and recurrences of new atrial tachyarrhythmias occur, and I will explain why later. And in the third month we must decide what to do next. This is followed by an immediate postoperative period of three to twelve months of observation. And after twelve months - the late postoperative period.
What problems await us in the early postoperative period? First of all, the most unpleasant thing is that 15% of patients referred for invasive treatment of atrial fibrillation feel even worse in the first two to three months. And this is the question of so-called anti-advertising. The doctor who referred the patient for radiofrequency ablation therefore receives this patient after one or two weeks, and the patient tells him: “Doctor, I feel worse.” Indeed, 15% of patients experience some kind of deterioration after radiofrequency ablation. And this deterioration is due to the fact that 45% - 50% experience atrial tachyarrhythmias. And now we are already saying that if you take all these atrial tachyarrhythmias, atrial fibrillation returns in 50%, relapses, early relapses, and 50% new regular atrial tachycardias. And the most unpleasant thing is that it is new atrial tachycardias that constitute the difficulty in therapy, in diagnosis, because underneath they can lie left atrial flutter, atrial tachycardias - ectopic, which are very difficult to respond to drug therapy.
And here is an example of a cardiogram, which shows left atrial atrial flutter in the early postoperative period. Previously, we saw practically little left atrial flutter at all. And it was after radiofrequency ablation that these paroxysms began to appear, which sometimes cause us quite difficulties in choosing treatment tactics. And here is an example of such an unstable paroxysm of atrial tachycardia, which is continuously recurrent; sometimes they occur in such patients precisely in the early postoperative period.
What is the problem with the early postoperative period? First of all, these relapses are associated with an inflammatory reaction caused by thermal damage to the atrial tissue. We must also not forget about the autonomic nervous system. The fact is that the inner surface of the heart does not have pain receptors, but it has a very powerful autonomic nervous system, and this nervous system is excited. And, of course, as long as inflammation exists, sometimes new atrial tachycardias are launched. And we must not forget about the delayed effect of radiofrequency ablation - the indirect formation of the so-called scar barrier. Because as long as there is an area of inflammation, arrhythmia can be carried out, but when a scar is formed, of course, the protection of the insulation of the mouth of the pulmonary veins is already stronger here.
But early recurrences of atrial fibrillation or new atrial tachyarrhythmias are not such a standard that radiofrequency ablation is ineffective. 60% of patients with early relapses of atrial tachycardia then had clear, stable sinus rhythm, and the procedure was considered effective. Therefore, one cannot assume that if a patient has early relapses of atrial fibrillation or some other atrial tachycardia, this is an ineffective procedure. But in those patients in whom we have complete effectiveness of radiofrequency ablation both in the early and late postoperative period, we will already talk about the absolute effectiveness of radiofrequency ablation. Therefore, there is such terminology as absolute effectiveness and early effectiveness. We are talking about early effectiveness if no attacks occur in the first three months.
What examination methods should be performed in such patients? Collecting anamnesis, identifying symptomatic attacks of arrhythmia. Of course, after radiofrequency ablation, patients are more attentive to themselves and make complaints. Often they may complain of increased heart rate, or even some pain in the heart area. The patient needs to have a 12-lead ECG to determine both cardiac conduction disturbances and arrhythmia disturbances. It is necessary to conduct 1-7 days of Holter ECG monitoring to detect asymptomatic arrhythmias. We recommend Holter monitoring after a month, two, three to evaluate further treatment tactics.
Now there are also such methods as an implantable subcutaneous cardiac monitor, loop cardiac monitors, ECG, which allow monitoring the cardiogram for up to three years. And at each visit, the doctor can take readings and evaluate asymptomatic recurrences of atrial fibrillation.
What are the tactics for managing patients after radiofrequency ablation in the early period? We must decide on antiarrhythmic therapy, the need for antiarrhythmic therapy, and antithrombotic therapy - this is very important, I will say this at the end. And we can use non-drug treatments during the blind period. Transesophageal electrical stimulation is now very actively used to restore new tachycardias, for example, left atrial flutter. And it has recovery efficiency during transesophageal stimulation. If the patient is hemodynamically compromised, we must perform electrocardioversion.
What is the issue of antiarrhythmic therapy in the early postoperative period? Now it is not clear whether these patients need to restore the rhythm or try to maintain sinus rhythm. Because there is no clear concrete data yet on which choice of tactics is better than “ri? The 2007 consensus on catheter-based and surgical ablation of atrial fibrillation considered only amiodarone for management to maintain sinus rhythm. But I absolutely disagree, because we take patients who are quite young, we take patients without organic pathology. And then after radiofrequency ablation, putting him on amiodarone - a toxic drug is absolutely unjustified. Therefore, the 2012 consensus suggests a more expanded list of antiarrhythmic drugs: flecainide, propafenone, sotalol, dofetilide, or dronedarone. But so far there are no clear specific recommendations.
Management tactics are precisely in the third month, when the blind period ends. In the third month, we must clearly understand what to do next with this patient, whether it is necessary to perform repeated radiofrequency ablation. The fact is that repeated radiofrequency ablation is performed quite often (according to many authors, up to 20% to 40%) - in our clinic up to 40%, and this is an absolutely normal tactic for managing patients. But only after the third month, when the inflammation has passed, should we say whether repeat radiofrequency ablation is necessary or not. If we analyze late relapses of atrial tachyarrhythmias, if the patient underwent only one radiofrequency ablation, late relapses occur in 11% - 29% of cases. If the patient has undergone at least two radiofrequency ablations, unfortunately, late relapses still occur (according to different authors, from 7% to 24% of cases).
What are the causes of late relapses of atrial tachyarrhythmias? First of all, this is the resumption of radiofrequency ablation in the area of the mouth of the pulmonary veins, when our isolation began to transmit an impulse. And more often than not, what occurs is the presence of triggers located outside the pulmonary veins. We often refer patients to isolation of the mouth of the pulmonary veins, which cannot be said to be neglected, but when time is running out. And from the source of the mouth of the pulmonary veins, the ectopia descends onto the atrial tissue. We isolated only the mouth of the pulmonary veins, but we cannot isolate all the atria, so, of course, these triggers begin to fire and begin to give late relapses. But I can immediately say that late relapses can be treated quite well with our modern antiarrhythmic therapy.
I would like to present our interesting research, which began back in 2009 at the Moscow Regional Cardiology Center and was further continued at the State Scientific Research Center for PM. This was a pilot project. We examined 134 patients who underwent antral isolation of the mouth of the pulmonary veins. And here are the results we got. Early relapses of atrial tachycardia up to three months occurred in almost 50% of cases. But only about 30% of these patients came to repeat radiofrequency ablation.
The next very important point. In 30% of patients, regular atrial tachycardias predominated, that is, there were quite a lot of regular atrial tachycardias, which sometimes baffled our doctors on how to treat them. And most often left atrial flutter prevailed. And in 20% of cases there were relapses of atrial fibrillation.
These patients were observed for up to 12 months, but we were more interested in the blind period, because we selected different patient management tactics, and one group of patients did not take antiarrhythmic drugs at all. We have now begun to include patients with revili implantation (00:15:58) to exclude asymptomatic relapses of atrial fibrillation, and we already have 39 such patients with implanted monitoring devices, but the study has not been completed, so I cannot tell you the final data.
I would like to say so far based on the results obtained. 36% of patients continue to take antiarrhythmic drugs even after the early postoperative period. And here there is such a thing as the clinical effectiveness of radiofrequency ablation. That is, we reduce the number of attacks of atrial fibrillation by 75%, the patient feels better than before radiofrequency ablation. But radiofrequency ablation does not completely eliminate these attacks. But together with taking antiarrhythmic drugs, the patient is satisfied with this, and attacks are quite rare - two or three times a year, and this suits us.
Today, the most effective antiarrhythmic drug in the postoperative period after three months and after radiofrequency ablation is a class 1C drug - propafenone. But this is greater in patients with recurrent atrial fibrillation. If patients develop new regular atrial tachycardias, then propafenone is often combined with verapamil, or verapamil alone - in such patients it showed good results.
At the end of the presentation, I want to show a few slides about the problems of thromboembolic complications in such patients. It cannot be said that radiofrequency ablation is an absolutely safe procedure, and in 0.6% thromboembolic or cardiogenic strokes occur, and in 1% of cases these are transient ischemic attacks. But today the most discussed issue is the emergence of “silent” ischemic strokes. And some authors write that up to 35% of such patients have “silent” ischemic strokes. What could be the reason for the appearance of such a large number? Not only with thromboembolic problems, but one must understand that the specifics of the radiofrequency ablation procedure and the appearance of air emboli can also make a serious contribution to the definition of “silent” ischemic strokes.
What is the problem of blood clots and thromboembolic complications? 1) This is a large area of damage to the atrial endothelium. 2) Installation of a transseptal introducer and electrode catheters. 3) Atrial stunning is a very important point. This is approximately how during cardioversion the atria are stunned, and all the conditions are created for the formation of blood clots. And this risk of thromboembolic complications directly depends on the score on the CHA2DS2-VASc scale.
And here is an example borrowed from an American journal, an article came out a couple of months ago, where the transesophageal echo data is clearly presented, and we see soft blood clots on the transseptal septum. And the second picture shows charred elements at the end of the electrode after removal from the transseptal septum, which can cause both minor and serious brain disorders. But this is on the one hand, on the other hand you need to understand that there is a problem of thromboembolic complications, but there is also a problem of bleeding. And such a problem as pericardial tamponade occurs from 0.8% to 6% depending on different sources. Vascular complications occur in 0% to 13%. Therefore, on the one hand, we must still prepare the patient with anticoagulants, but on the other hand, understand that there is a risk of bleeding.
Today there is the following tactics. Preparing patients for radiofrequency ablation should be the same as for electrical cardioversion. For patients with atrial fibrillation for more than 48 hours, if we do radiofrequency ablation, it is definitely necessary to do a transesophageal echo, because thrombosis of the left atrial appendage is a contraindication for this procedure. 4-6 hours after radiofrequency ablation, we should start either warfarin or new oral anticoagulants. And, of course, today the use of new oral anticoagulants during radiofrequency ablation is very much discussed. But so far there is no clear data on which of the new oral anticoagulants actually benefits. Cancellation of anticoagulant therapy should be carried out in the second or third month (according to European data in the second month, in the third month - according to Russian recommendations). But if the patient has at least one point on the CHA2DS2-VASc scale. we must continue to place this patient on anticoagulation therapy because we cannot clearly say that this patient will not have late recurrences of atrial fibrillation. With this I want to finish my report. Thank you for your attention.