Stages of development of a heart attack with ST segment elevation
The most acute stage of STEMI
First, a high coronary T appears on the cardiogram. The high coronary T before ST elevation is present for a very short time, so it is not always possible to register it. Then there is an increase in the ST segment, which merges with a high T.
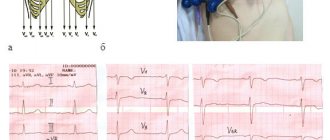
Scheme 2. ECG fragments in the most acute stage of STEMI
Acute stage STEMI
Lasts up to 2-3 days (sometimes up to 2 weeks). The beginning of the acute phase is considered to be the appearance of the Q wave, which reflects the formation of a zone of myocardial necrosis. As the acute phase develops, the Q wave deepens, and the ST segment begins to decline towards the isoline. The T wave becomes negative.
Scheme 3. ECG fragment in the acute stage of STEMI
Subacute stage of STEMI.
Lasts for several weeks. The ECG records a decrease in the ST segment to the level of the isoline. At the same time, a deep negative T wave is formed.
Scheme 4. ECG fragment in the subacute stage
Scar stage STEMI
Dead myocardial cells are replaced by connective tissue, which leads to the formation of a scar. The areas of the myocardium surrounding the scar undergo compensatory hypertrophy. The number of leads on the ECG in which changes associated with a heart attack are recorded is reduced. The Q wave may become less deep, and the T wave returns to the baseline. The formed picture of post-infarction cardiosclerosis on the ECG persists throughout the patient’s life.
Sometimes the ST segment does not reach the isoline and remains elevated almost throughout life. As a rule, the QRS complex takes on the QS form, which may indicate the formation of a cardiac aneurysm.
Scheme 5. ECG fragments with post-infarction changes
Diagram 5 on the left shows a fragment of a cardiogram indicating a myocardial infarction. On the right is a fragment of a cardiogram in which the ST segment has not reached isolia and a QS complex has formed, turning into increased ST. This picture is called a “frozen ECG” and indicates a post-infarction cardiac aneurysm.
Treatment
The symptoms that accompany myocardial infarction are very diverse. If myocardial infarction is suspected
The most reasonable action would be to immediately consult a doctor, rather than self-diagnosis or self-medication. In case of myocardial infarction, treatment should begin as early as possible; you must immediately call an ambulance team. Before the team arrives, it is recommended to take a sitting position, preferably on a chair with a backrest, or reclining. Tight, disturbing clothes are unbuttoned and the tie is loosened. It is necessary to immediately take nitroglycerin under the tongue. If the pain decreases within 5 minutes, repeat the dose. It is advisable to chew 300 mg of aspirin. It is important to chew the tablet, otherwise the aspirin will not work quickly enough. In case of cardiac arrest, cardiopulmonary resuscitation is started immediately. Its use greatly increases the patient's chances of survival. Patients with suspected myocardial infarction must be taken to the clinic. After confirmation of the diagnosis, treatment continues in the intensive care unit. You should not hesitate to call an ambulance, since the patient must be hospitalized in a hospital no later than 6 hours from the onset of a painful attack in order to avoid irreversible changes in the myocardium and possible early complications. If possible, a patient with myocardial infarction should be hospitalized in a hospital, where an urgent coronary angiography will be performed, as well as balloon angioplasty (opening of the vessel) and stenting (implantation of a metal frame) of the affected artery, that is, a set of measures that directly affects the cause of the vascular accident.
Scheme of inpatient drug treatment of myocardial infarction:
- Administration of strong painkillers. As a rule, narcotic drugs are used.
- Administration of drugs that reduce blood clotting and promote the resorption of blood clots.
- Intravenous administration of nitroglycerin.
- Intravenous administration of drugs that reduce myocardial oxygen demand.
- Lowers blood pressure and reduces the load on the heart.
- Oxygenation (supply of humidified oxygen).
- Continuous ECG monitoring and blood test control.
The multidisciplinary CELT clinic has created conditions for the most effective treatment of myocardial infarction and its consequences; there is everything necessary to combat this condition and possible complications.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Localization of infarction with ST elevation
Changes in cardiograms during a heart attack with ST segment elevation vary depending on which part of the heart the heart attack develops in. The location of the infarction can be determined by the ECG leads in which ST elevation is recorded and in which leads reciprocal ST depression appears. In this regard, remember which leads correspond to different parts of the myocardium. Look at diagram 6.
Scheme 6. Correspondence of cardiogram leads to different areas of the myocardium.
Schema source.
Diagram 7 below shows the location of large coronary arteries, the occlusion of which can lead to transmural infarction with appropriate localization.
Scheme 7. Large coronary arteries
| Localization of infarction | ST elevation leads | Leads with reciprocal ST depression |
| Interventricular septum | V1-V2 | |
| Front wall | V3-V4 | |
| Lateral wall of the left ventricle | I, aVL, V5-V6 | III, aVF |
| Bottom wall | II, III, aVF | I, aVL |
| Back wall | V7-V9 | V1-V3 (and high R in V1-V3) |
| Right ventricle | V1, III, II (STIII > STII), V3R - V5R | V2 |
The table above shows which leads show ST elevation or depression depending on the location of STEMI. In practice, ST elevation infarction usually affects more than one area. For example, an infarction of the interventricular septum is usually combined with an infarction of the anterior wall of the left ventricle. In this case, ST elevation will be not only in leads V1-V2, but also in V3-V4.
Let's consider STEMI options with different localizations.
Interventricular septal infarction
As mentioned above, isolated septal infarction is a rare occurrence (usually septal and anterior wall infarction). Septal infarction develops as a result of occlusion of the left anterior descending artery (LAD). The cardiogram records ST elevation in leads V1-V2.
Scheme 8. Infarction of the interventricular septum
ECG 2. Myocardial infarction of the interventricular septum
ECG source.
On ECG 2, an infarction of the interventricular septum is indicated by pathological Q waves in leads V1-V2 and moderate ST elevation in the same leads. Judging by the ST height and the presence of Q waves, this is a subacute stage of infarction. In addition, in this case there is diffuse ST segment depression in leads I, II, V4-V6 in combination with ST elevation in aVR. This indicates subendocardial myocardial ischemia.
Risk factors
Myocardial infarction can develop rapidly without any external influences or be the result of a long illness. Some people are more likely to have a heart attack.
At risk:
- smokers;
- hypertensive patients;
- diabetics;
- overweight patients;
- people with lipid metabolism disorders;
- people with physical inactivity and leading a sedentary lifestyle;
- athletes during preparation for competitions;
- patients with depression or those in a state of chronic stress;
- patients with renal failure;
- those suffering from psoriasis and arthritis;
- people who have already had a heart attack before;
- the presence of mental disorders accompanied by mania, anxiety, hyperactivity;
- people over the age of 55 (men) and 65 (women) years.
The difference between age-related risks for men and women is explained by significant differences in lifestyle, physical activity and health habits. As a rule, men who undergo medical examination and lead a healthy lifestyle reduce their risk indicators to those of women.
Moreover, for men, the risk of an early heart attack is several times higher, and a woman is protected at the hormonal level before menopause - estrogens provide high elasticity of blood vessels and reduce the risk of fatal myocardial damage.
Anterior wall infarction
ST elevation infarction in the anterior wall region develops as a result of occlusion of the left anterior descending artery (LAD). The cardiogram records ST elevation in leads V3-V4. A reciprocal decrease in ST occurs in the inferior leads: III, aVF. Subsequently, pathological Q is formed in V3-V4.
Scheme 9. Infarction of the anterior wall
An infarction of the anterior wall, as a rule, is not isolated and is most often combined with an infarction of the interventricular septum and/or an infarction of the lateral wall of the left ventricle. This is determined by the fact that the interventricular septum and lateral wall are also supplied by the left anterior descending artery (LAD).
ECG 3. Infarction of the septum, anterior wall and partly the lateral wall of the left ventricle
ECG source.
On ECG 3, ST elevation in leads V1-V4, as well as deep Q waves in V1-V2, indicate infarction in the area of the interventricular septum (ST elevation in V1-V2) and the anterior wall of the left ventricle (ST elevation in V3-V4). There are tall coronary T waves in V2-V4. There is also slight ST elevation in leads I, aVL and V5, which may indicate extension of the infarction to the lateral wall of the left ventricle.
There is a reciprocal decrease in ST in lead III. These are signs of the acute phase of myocardial infarction with ST elevation.
ECG 4. Infarction of the anterior and lateral walls of the left ventricle
ECG source.
On ECG 4 there is ST elevation in leads V2-V6, I, aVL. Elevation in V3-V4 with maximum elevation in V3 indicates an infarction of the anterior wall, and ST elevation V5-V6, I, aVL indicates an infarction of the lateral wall of the left ventricle. In III and aVF there is reciprocal ST depression.
ECG 5. Extensive infarction of the interventricular septum, anterior and lateral walls of the left ventricle. “Tombstoning” pattern
ECG 5 shows massive ST segment elevation in leads V1-V6, I, aVL, reciprocal ST decrease in leads III and aVF. This morphological pattern on the cardiogram is called the “tombstoning” pattern and indicates occlusion of the proximal LAD. A prognostically unfavorable option with a high probability of damage to a large part of the myocardium with a sharp decrease in cardiac contractility and the development of cardiogenic shock.
Causes of the disease
- Myocardial infarction almost always develops against the background of atherosclerosis of the heart vessels, the so-called. coronary arteries. When the integrity of an atherosclerotic plaque is disrupted, a blood clot forms in the lumen of the vessel, which leads to a sudden cessation of blood flow in the artery of the heart and myocardial infarction.
- Very rarely, an acute disruption of the blood supply to the heart muscle can occur during prolonged spasm of the coronary arteries, for example, during physical or psycho-emotional overload.
At CELT you can consult a cardiologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Left ventricular lateral wall infarction
Left ventricular lateral wall infarction with ST elevation, as discussed above, is usually associated with anterior wall infarction. In addition, it can be combined with infarction of the lower or posterior wall. It develops as a result of occlusion of the left anterior descending artery (LAD) and/or the circumflex coronary artery (LCX).
Isolated lateral wall infarction is less common and is associated with occlusion of the small branches of the LAD or the marginal branch of the LCX.
Scheme 10. Infarction of the lateral wall of the left ventricle
On the cardiogram with a lateral wall infarction, ST elevation is recorded in leads I, aVL, V5-V6. If ST elevation is only in leads I, aVL, but not in leads V5-V6, they speak of a high lateral infarction. A reciprocal decrease occurs in leads III, aVF.
Examples of lateral wall infarction combined with anterior wall infarction were shown above (see ECG 3-5).
ECG 6. High lateral left ventricular infarction
ECG source.
ECG 6 shows ST elevation in leads I and aVL, as well as reciprocal depression in leads III, aVF. There is no ST elevation in leads V5-V6. These are signs of high lateral left ventricular infarction.
Infarction of the inferior wall
Inferior wall infarction with ST elevation in most cases (up to 80%) develops as a result of occlusion of the right coronary artery (RCA). In this case, the infarction of the lower wall can be isolated or combined with a right ventricular infarction.
Scheme 11. Infarction of the inferior wall
Less commonly, inferior wall infarction may be caused by occlusion of the left circumflex artery (LCX). This option can lead to the development of infarction of the lower and posterior wall, which has a worse prognosis due to the larger area of myocardial damage.
In rare cases, it is possible to develop a lower infarction with distal occlusion of the left anterior descending artery (LAD). This leads to a combination of infarction of the anterior and inferior walls.
In case of infarction of the lower wall, elevation of the ST segment and the subsequent formation of a pathological Q wave in leads II, III, aVF are recorded on the cardiogram. Reciprocal ST depression occurs in lead aVL and (not always) in lead I.
ECG 7. Inferior wall infarction with ST elevation
ECG source.
ECG 7 shows ST elevation and Q waves in leads II, III, aVF. At the same time, there is reciprocal ST depression in leads I and aVL. These changes indicate STEMI of the inferior wall of the left ventricle.
Posterior wall infarction
An infarction of the posterior wall, as a rule, develops in combination with an infarction of the lower or lateral wall of the left ventricle. Isolated posterior wall infarction occurs in no more than 10% of cases. However, isolated posterior wall infarction is not always recognized in a timely manner, since it develops infrequently and there is no ST segment elevation on a standard 12-lead cardiogram. To confirm this diagnosis, it is necessary to use additional posterior leads: V7-V9. Posterior wall infarction can be suspected from a 12-lead ECG based on the following signs:
- ST segment depression in leads V1-V3. This ST depression is reciprocal to ST elevation in the accessory posterior leads (V7-V9).
- Tall and usually widened R waves in leads V1-V3.
- The R/S ratio in V2 is greater than 1.
- Positive T wave in leads V1-V3.
ECG 8. Infarction of the posterior and inferior wall of the left ventricle with ST elevation
ECG source.
On ECG 8, ST segment depression, as well as a tall and wide R wave in leads V2-V3, indicate infarction in the posterior wall of the left ventricle. To confirm this diagnosis, a cardiogram was recorded using additional leads V7-V9, where ST elevation was recorded. In addition, in leads III, aVF, slight elevation of the ST segment was also recorded, which indicates involvement of the lower wall of the left ventricle in the process.
ECG 9. Infarction with ST elevation of the lateral and posterior wall of the left ventricle
ECG source.
On ECG 9, ST elevation in leads I, aVL, V5-V6 and reciprocal ST depression in leads III, aVF reflect infarction of the lateral wall of the left ventricle. In addition, there is a decrease in ST in leads V1-V3, which, in combination with high R waves in these same leads, may indicate posterior wall damage. Thus, in this case there is an infarction of the lateral and posterior wall of the left ventricle. To confirm posterior wall infarction, an ECG should be recorded in additional posterior leads (V7-V9).
RECOMMENDATIONS FOR LFK
Classes at the hospital stage must be conducted by a physical therapy instructor. Although the complex for this group of patients is very gentle, the load still depends on the patient’s condition. Severe degrees require complete rest during the first week. With moderately severe patients, the instructor begins classes on the 2nd – 3rd day.
On the 4th – 5th day the patient is allowed to sit for some time on the bed with his legs dangling. From the 7th day you can take your first steps near the bed. After a couple of weeks, the doctor will allow the patient to “walk” around the ward. Go out into the hallway - from the 3rd week. With the help of an instructor, you can try to climb several steps. The number of steps and meters covered is growing every day (up to 500 - 1000 m). The patient is under the supervision of doctors or relatives, because his condition needs to be constantly assessed - by heart rate (heart rate - pulse) and blood pressure level. For reliability, these indicators are checked before the walk (half an hour) and after (half an hour).
If the treatment proceeds without complications, the patient, after an inpatient course, is sent to a cardiological sanatorium somewhere in the suburbs. There is no need for such a patient to travel long distances. There, as part of a 4-week rehabilitation course, he will receive:
- Drug treatment.
- Help from a psychotherapist.
- Diet food.
- Dosed physical activity.