Vascular surgeon of the City Clinical Hospital named after. S.S. Yudina talks about the benefits of stenting for atherosclerosis.
Why stenting is the optimal surgical solution to the problem within the framework of compulsory medical insurance, said the head of the department of X-ray surgery of the S.S. City Clinical Hospital. Yudin in Moscow Vitaly Mikhailovich Sysoev.
How is stenting different from coronary artery bypass grafting?
Stenting is a minimally invasive method for treating coronary heart disease. It is fundamentally different from bypass surgery in that it causes minimal trauma to the patient and has a short rehabilitation period.
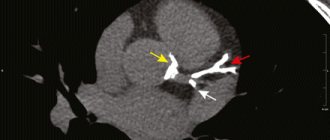
A stent is an implant in the form of a frame that is installed in a vessel. It usually consists of a metal base on which a special polymer containing a medicinal substance is applied. The stent itself is mounted on a balloon catheter, which is necessary to deliver this frame to the affected area of the artery. Drug coating on the stent is necessary to ensure that it works as long as possible, so that restenosis, or repeated narrowing of the vessel after implantation, does not occur. Medicines that are applied to the stent prevent the growth of the so-called inner lining of the capillary, thereby preventing this segment of the artery from narrowing.
Stenting belongs to the category of high-tech operations.
Repeated stenting
The patient’s most common question after stenting is how long the stents will function and whether repeat stenting is possible.
It should be noted that the vast majority of people who undergo this procedure do not have any complications and live with an implanted stent all their lives, since they are made from materials that can perform their intended function constantly, that is, for decades.
This occurs due to the fact that some time after the operation the stent begins to become overgrown with endothelial cells, becoming one with the arterial wall. But there are cases when stent restenosis occurs. More often this happens when a stent is installed at the location of a large atherosclerotic plaque or a large extent of vessel narrowing.
Recently, in order to prevent restenosis, specialists have begun to actively use drug-eluting stents, from which, after implantation into the coronary vessel for several weeks, a pharmacological drug is released that prevents excessive growth of the intima (inner lining) of the artery and the increase in atherosclerotic plaque. Taking into account modern capabilities, successful results of stenting are observed in 95% of patients who have undergone it.
The choice of a specific type of stent is determined by an x-ray endovascular surgeon based on diagnostic data obtained during a preliminary examination of patients, as well as concomitant pathology (for example, diabetes mellitus).
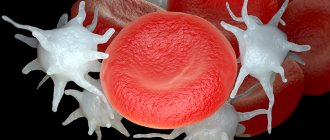
Non-drug drug therapy reduces the likelihood of restenosis: lifestyle changes, regular dynamic physical activity, quitting smoking, proper nutrition, taking drugs to prevent thrombosis (aspirin and clopidogrel) for a year, constant use of statins in adequate doses under the control of biochemistry and other drugs for the treatment of coronary heart disease.
Often the cause of deterioration is not restenosis of an already installed stent, but the progression of atherosclerosis in other coronary arteries with the development of severe stenosis. Therefore, after stenting, if you have new attacks of angina or decreased tolerance to physical activity, you need to consult a doctor for further examination: echocardiography, stress tests. If ischemia is confirmed, you will be offered a repeat coronary angiography.
Based on its results, it is determined which vessel is affected. If stent restenosis has developed, then there are 2 ways to get rid of it: the stent blocked by a thrombus is expanded with an air balloon inserted into it (angioplasty) or another stent is inserted inside the blocked stent. If stenoses are detected in other previously unaffected arteries, then stenting is performed.
How is stenting surgery performed?
Stenting, like coronary angiography, takes place under local anesthesia, which is very convenient for both the patient and the doctor: the person being operated on is conscious and can communicate.
The operation is performed through an injection into an artery in the arm or leg. Thus, a special catheter is delivered into the vessels of the heart, through which a contrast agent is injected so that the operating surgeon can determine which vessel is affected and what length and diameter of the stent must be selected in this case. After the doctor decides on the extent of the surgical intervention, he will need such special tools as a guidewire and the stent itself. A guidewire is a thin metal wire with a diameter of less than 1 millimeter, which is inserted behind the narrowed section of the artery in order to then deliver a balloon catheter to the affected area. Next, dilatation (inflation) of this balloon occurs - the stent expands, is pressed into the wall of the artery and remains in this position: it expands its lumen and restores patency.
After dilatation is completed, the doctor removes the balloon catheter, injects a contrast agent and makes sure that the stent is positioned correctly, the vessel is dilated and there are no complications. At the end of the operation, all instruments, except the stent itself, are removed from the body, and the patient is transferred from the cath lab to the department. Within 24 hours he may be home.
As part of compulsory medical insurance, the patient has access to coronary angiography, stenting of the heart vessels, arteries of the lower extremities and carotid arteries.
The role of coronary artery stenting in patients with stable coronary artery disease
Transcript of the author's program by Professor S.R. Gilyarevsky, broadcast on March 14, 2012.
Drapkina O.M.: - Good evening, dear colleagues! We continue meetings within the framework of the evidence-based cardiology program. And again with you is the author and presenter - Professor Sergei Rudzherovich Gilyarevsky, scientific director of the department of emergency cardiology of patients with myocardial infarction at the Scientific Institute named after. Sklifosovsky.
Gilyarevsky S.R.: - Good evening. Yes, the Institute of Emergency Medicine named after. Sklifosovsky. And, probably, Oksana Mikhailovna wanted to say that I am visiting your program today as a representative of emergency cardiology.
Drapkina O.M.: - No, I can’t say that, you’re at home. As a representative of emergency cardiology and why - because today we will talk specifically about a fragment of this emergency cardiology, namely, stents. Sergei Rudzherovich, you are always in store, somewhere looking for evidence of such sometimes sensational facts. What awaits us today? What are we going to talk about?
Gilyarevsky S.R.: — We will talk about the role of coronary artery stenting in patients with stable coronary heart disease. And, probably, for us, cardiologists in Russia, this is much easier to discuss than, say, for interventional cardiologists, since abroad there is no division between (as far as I know) interventional cardiologists and specialists in X-ray endovascular treatment methods, because in general, recently There has been a trend towards a more cautious determination of indications for coronary artery stenting. And in one of the programs, if you remember, we presented a case published in the Journal American Cardiology, where one patient had 67 stents implanted, and the patient had both coronary artery bypass surgery and then stenting simply in the coronary arteries , and in shunts. And, of course, this approach, which is a consequence of such a negative phenomenon, which is designated by the term “stenism.” Stentism is when the decision to implant a stent is made by the operator, although now all clinical guidelines say that the decision to stent in most cases or in some doubtful cases should be made taking into account the clinical manifestations of the disease.
Drapkina O.M.: - Who is the operator?
Gilyarevsky S.R.: — The operator is the person who directly installs the stent. Naturally, there is no need to stent everything that is narrowed. There are special methods that allow you to identify hemodynamically significant arteries. Of course, stress tests are also performed, but, unfortunately, stress tests are not always so sensitive, and sometimes not even so specific, as to refuse to perform coronary angiography. There are methods for assessing hemodynamic significance by determining the fractional reserve of blood flow of the coronary arteries, when they look at the difference between the aorta and the distal coronary artery. And if the difference in pressure is 20%, then the issue is resolved after stimulation with aminazine and vasodilators, then a decision is made about stenting the coronary artery.
But again, this still needs to be approached individually. And the complexity of the evidence-based history in this area lies in the fact that the first studies, a meta-analysis of which indicated a positive effect of angioplasty on prognosis compared to drug therapy, were performed when, firstly, there was no stenting of the coronary arteries, it was only angioplasty, on the one hand. This could reduce the effectiveness of the intervention. On the other hand, there was no drug therapy like what we have now. Those. the patients took anti-ischemic drugs, and ACE inhibitors, and that’s it. There were no statins that fundamentally changed the course of coronary heart disease. And therefore, the results of a meta-analysis, which was published not so long ago in the journal Archives of Internal Medicine, are of interest, in which they tried to analyze what effect coronary artery stenting has, i.e. angioplasty with stenting on the course of coronary heart disease compared with optimal drug therapy. Those. stenting with therapy and one optimal therapy.
During the course of this analysis, 8 randomized clinical trials were included in this analysis, and if you see, such famous studies as the COURAGE trial, the OAT trial, the BARI 2D trial. In the course of, say, the COURAGE study, if we recall, patients with coronary heart disease were compared with either standard therapy, which included very powerful lipid-lowering therapy regimens, i.e. there, patients received statins and most patients received ezetimibe, and the level of low-density lipoprotein cholesterol actually decreased to the levels that are given in the recommendations.
Against this background, stenting did not lead to a statistically significant improvement in prognosis. The well-known BARI 2D studies have been performed in diabetic patients with inducible ischemia or angina and found similar results. You can see on this slide what the characteristics of the patients were: the average age is about 60 years, as always in such studies, patients with coronary heart disease were mostly men. Diabetes mellitus was presented differently - you see, from 14 to 100% of the BARI 2D study had previously suffered a heart attack, in some studies all patients, in particular in the OAT study, which assessed the effectiveness of coronary artery angioplasty in the majority with stenting in patients at long-term terms after acute myocardial infarction, relatively long-term, 3-28 days after the development of symptoms of myocardial infarction. And the number of vessels that were tampered with was not so large. On average, this is an intervention on one or two, mostly on one vessel. And this, too, probably influenced the results of the study, including the meta-analysis, since it is well known that with single-vessel lesions, drug therapy is...
Drapkina O.M.: - Undoubtedly better.
Gilyarevsky S.R.: - Yes. But, nevertheless, such a meta-analysis was performed, and in this slide, indeed, it confirms that the therapy was very good. Patients received both antiplatelet agents and a beta blocker, most of the patients received ACE inhibitors (in most studies there was still a high frequency of use) and the use of statins from 45 to 100%. It is very important that this is a modern stage. The data that was obtained earlier concerned the previous stages, when the therapy was not so effective. Now this is what happened against the backdrop of such highly effective therapy. Here's what happened. As you can see, coronary artery stenting in patients with stable coronary artery disease did not lead to a decrease in overall mortality compared with optimal drug therapy.
The next indicator is the incidence of non-fatal myocardial infarction. And here (at first glance, these data may seem paradoxical) there is a clear tendency to increase the risk of developing non-fatal myocardial infarction with stenting compared... i.e. clear advantage of optimal drug therapy. Why? They explain it this way. Firstly, intervention on the coronary artery, stenting of the coronary artery - after all, the participation of patients is accompanied by embolization of the distal sections. This can lead to the development of myocardial infarction. Of course, this myocardial infarction usually does not have the same clinical significance as spontaneous myocardial infarction, and diagnostic approaches have also been very different. Some authors believed that any increase in troponin levels after intervention is a consequence of clinically significant necrosis, but now it has become clear that this is not so, that troponin increases quite often and that it is better to focus in this situation, oddly enough, on the concentration of CPK. And it is believed that if after the intervention the concentration of creatine phosphokinase increases 5 times, the MB fraction increases 5 times or more compared to the upper limit of normal, then this already indicates a clinically significant heart attack associated with the intervention.
Drapkina O.M.: — I want to say about the troponin test. Its specificity is within the first 3 hours, sensitivity is 33%.
Gilyarevsky S.R.: - Yes, special sensitivity. If it is coronary heart disease, and you know that the patient had ischemia and there is an increase in the concentration of troponin in the blood over time, then this is still a fairly specific method. If there is no dynamics, then, of course, an increase in troponin levels may occur in patients with renal failure or heart failure. But there should be no dynamics there.
Drapkina O.M.: - It’s no coincidence that the latest recommendations are already included twice, because the first ones are these...
Gilyarevsky S.R.: - Even now it is proposed to take such an algorithm with an interval of 3 hours upon admission. And if there is dynamics and at least one indicator exceeds 99%, then we can already talk about a diagnosis of a heart attack.
Drapkina O.M.: - But the biggest one is day 4.
Gilyarevsky S.R.: - Still, yes. But in this case, increasing the level of troponin is not enough... it is too sensitive, because slight damage to the myocardium can occur and embolization in areas, destroyed plaques, this happens. Therefore, in order for the diagnosis of “heart attack” in this case to truly reflect the clinical situation, they began to focus on MB, CK, if it increases 5 times compared to the upper limit of normal, then yes. If we go back to the slides and try to explain these results further. Why does coronary artery stenting in patients with stable coronary heart disease not reduce the risk of developing a heart attack? Yes, because, paradoxically, the affected area of the artery that causes the development of angina pectoris, as a rule, does not cause the development of a heart attack, because angina pectoris develops where there is a dense, usually large, hemodynamically significant plaque, and it does not is torn. And myocardial infarction occurs precisely in those areas of the coronary arteries that do not cause the development of myocardial ischemia. Even if the patient has stable angina, his heart attack does not develop due to the area that causes ischemia, so when you restore the patency of the artery in the area that causes the development of ischemia and, accordingly, angina, then you relieve the patient from angina, but you do not influence in any way those areas that later cause the development of myocardial infarction.
This is why drug therapy that targets atherosclerosis as a systemic process and leads to plaque stabilization reduces the risk of heart attack. So there is actually no paradox here, and this, of course, needs to be remembered. Still, the need for unplanned revascularization - the trend was slightly better in the group of patients who had coronary arteries stented... Well, either acute or due to worsening angina pectoris is also possible... Therefore, not all patients here were acute, i.e. revascularization was not only for acute coronary syndrome. But even here you can see how statistically it is better, but there is no statistically significant difference. Those. This graph shows that the confidence interval border still crosses unity. This means that the difference overall is not statistically significant. Well, such an indicator as persistent angina pectoris during observation. It is obvious here that there were positive dynamics in the stenting group. It is clear that stenting still relieves angina, but still does not achieve it, although this was a meta-analysis that included more than 7 thousand patients, i.e. statistical power was quite high. But, nevertheless, there were no statistically significant differences in this indicator. Thus, the authors concluded that to date, the initial tactics of coronary stenting in stable coronary heart disease have no advantage over optimal drug therapy.
Drapkina O.M.: — Most importantly, it should be optimal.
Gilyarevsky S.R.: — The main thing is that therapy should be optimal. Those. optimal therapy is antiplatelet agents, ACE inhibitors, statins and, of course, anti-ischemic therapy, this is understandable. Thus, these data suggest that it is necessary to more carefully approach the issue of stenting the coronary arteries and still, as an initial tactic, if this is a stable course of coronary heart disease, we still use optimal drug therapy, and only in In cases where it does not help, we raise the question of performing stenting. This in no way applies to an acute situation. In acute coronary syndromes, it has been precisely proven that stenting the coronary artery, which led to the development of acute coronary syndrome, myocardial infarction, that its stenting leads to an improved prognosis. And the numbers themselves speak about this. For example, mortality from acute myocardial infarction has decreased from 20% to 5%, and much of the credit lies in the methods of mechanical revascularization. But as for chronic patients, the prognosis of such patients depends largely on the stability of plaques in the coronary arteries as a whole, and not at all on...
Drapkina O.M.: - Sergei Rudzherovich, let’s remind you again at the end of the program. You said optimal therapy. And with a stable course of angina pectoris, the target levels of our main indicators are still the same: lipids, blood pressure, glucose.
Gilyarevsky S.R.: - This is downright difficult, because when it comes to blood pressure levels, then, probably, here the optimal pressure can be considered within the range of 140/80 mm Hg. Art. At least in the large TNT study, where there were 10 thousand patients with coronary heart disease...
Drapkina O.M.: - No higher than...
Gilyarevsky S.R.: — Most likely, not lower, because during this study (and there were all patients with stable coronary artery disease, there were 10 thousand of them), the lowest risk of complications was at a pressure level of 140/81 mm Hg. Art. Therefore, the more severe the coronary atherosclerosis, the more careful the reduction should be, especially for diastolic pressure. If, of course, you perform myocardial revascularization, then these numbers may be lower. But if there is a hemodynamically significant stenosis, it is better to approach carefully. As for the level of glycosylated hemoglobin, today after the ACCORD study it is less than 7. Well, again, if this is the initial stage of diabetes mellitus, then maybe it’s possible here... If this is a transition from prediabetes to diabetes, then, of course , in such patients one should strive for lower numbers. And this, by the way, is also in clinical recommendations that some patients may have less.
But if it is long-standing diabetes mellitus, within 10 years, of course, less than 7 and approach it very carefully, since this can worsen the prognosis, as was the case in the ACCORD study. As for lipids, everything is more or less clear. We can say that European recommendations are even stricter. And the European recommendations say that in any patient with coronary heart disease it is necessary to reduce the concentration of low-density lipoprotein cholesterol to less than 1.8 mmol/l, and this is the main indicator, because the level of triglycerides and the level of high-density lipoprotein cholesterol are still additional indicators. To date, there are no results from clinical studies that would prove that a decrease in these indicators, triglycerides, and an increase in high-density lipoprotein cholesterol leads to an improved prognosis, so we focus on low-density lipoprotein cholesterol and, following European recommendations, and now Russian ones, less than 1.8 mmol/l.
Drapkina O.M.: - Dear colleagues, we again encourage you to write and communicate with us. We are waiting for your suggestions on the topics of our future meetings.
Gilyarevsky S.R.: — And we wish everyone to look for evidence to validate our clinical practice.
Drapkina O.M.: - Thank you.
Gilyarevsky S.R.: - Goodbye. Thank you.
Are there complications after stenting?
Possible, but they are extremely rare. The most common ones include an allergy to the contrast agent, injury to the arterial wall when installing a stent, a hematoma at the injection site, and the formation of a blood clot in the area of the stent.
To prevent all this from happening, the patient must strictly take special blood thinners, which are prescribed to him even before the operation.
If pain occurs in the area of the heart or at the site of surgical access (where there was an injection into the artery), you must immediately contact the clinic where the operation was performed, and the problem will be eliminated.