Coronavirus is a disease that affects not only the lungs but also human blood vessels. Unfortunately, not every patient survives the COVID-19 infection without complications to the lungs and cardiovascular system. Having studied the features of SARS-CoV2 and discovered multiple blood clots, damage to the internal vascular endothelium, signs of myocarditis, as well as damage to other internal organs in dead patients, International medical organizations, including WHO experts, have recognized that the new coronavirus infection occurs with the occurrence of sepsis, blood poisoning.
In this article we will tell you how coronavirus affects blood vessels, what you need to pay attention to, and how to reduce the risk of vascular accidents.
Symptoms of atherosclerosis of neck vessels
The first manifestations of the disease can occur at an early age. They are expressed in the appearance of lipid stains in the vessels, from which atherosclerotic plaques subsequently develop. In the early stages of atherosclerosis, plaques do not interfere with blood flow in any way and the disease does not manifest itself clinically. Over time, atherosclerotic plaques narrow the lumen of blood vessels, which causes circulatory problems. The occurrence of atherosclerotic stenosis leads to a stable deterioration in blood flow.
Symptoms of atherosclerosis depend on the location of the process. Signs of atherosclerosis of the vessels of the head are transient ischemic attacks or stroke. With atherosclerotic narrowing of the coronary arteries, myocardial ischemia occurs, manifested by an attack of angina. Atherosclerosis of the coronary vessels of the heart in the elderly leads to myocardial infarction or sudden death. However, even complete occlusion (blockage) of an artery with plaque does not always result in a heart attack. Repeated ischemia may promote the development of collateral circulation, which mitigates the effects of occlusion.
Atherosclerosis of the arteries of the lower extremities causes ischemia and the development of intermittent claudication. The atherosclerotic process in the renal arteries leads to the development of persistent arterial hypertension. Damage to the mesenteric arteries is manifested by symptoms of intestinal ischemia.
Symptoms of atherosclerosis of neck vessels:
- headache;
- memory impairment;
- periodic dizziness;
- emotional lability;
- visual impairment;
- speech problems.
In the later stages, small tears appear on the surface of the plaques, platelet adhesion is observed, and blood clots form, which can completely block the lumen of the vessel, leading to myocardial infarction or stroke.
Cerebral circulation disorders in cervical osteochondrosis
Osteochondrosis is a degenerative-dystrophic disease of cartilage tissue that develops as a result of impaired metabolism of glycosaminoglycans. It can begin in almost any articular joint of the body, but most often it affects the intervertebral discs of the most mobile segments of the spinal column - the cervical and lumbar.
Since the intervertebral joints do not contain blood vessels, their nutrition and water supply occurs in a diffuse manner (by exchange with nearby soft tissues). With age, metabolic processes in the body slow down significantly or are disrupted, which leads to gradual dehydration and destruction of cartilage fibers, and, consequently, subsidence and thinning of the intervertebral discs.
Deformed joints are no longer able to fully perform their shock-absorbing functions, and with certain physical activities, pinching of nerve roots and blood vessels, pain, limited mobility and other complications occur. For the cervical spine these are headaches, dizziness, cerebrovascular accidents, hearing and vision disorders, etc.
Pathogenesis of the disease
Chronic pain syndrome, inflammation, spasms and discomfort when moving the head cause a response from the body, as a result of which growths of bone marginal plates (osteophytes) are formed. With sudden physical exertion or awkward movements, intervertebral hernias or protrusions may occur, when the dense shell of the disc cracks, releasing a gelatinous substance (nucleus pulposus). Quite often, it is osteophytes or hernial protrusions that compress the spinal blood vessels or nerve endings.
The cervical segment of the spine is designed in such a way that almost all the vital highways of the body that feed the brain lie in it, but it is supported and protected only by a very thin muscular corset.
As a rule, vascular pathologies are based on two main factors: compression of the vertebral or basilar arteries, as well as damage to the vasomotor (vasomotor) center located in the medulla oblongata. It is damage to the latter that causes dysfunction of the innervation of all smooth muscles of blood vessels (including the spinal cord and brain), which is fraught with sudden changes in blood pressure, hypoxia, ischemia, stroke, etc.
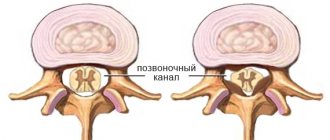
A decrease in the tone of the blood vessels of the brain, as well as the whole body, causes thickening of their walls or stenosis of the lumen of the canal, which can provoke disturbances in blood microcirculation, and, consequently, a slowdown in metabolic processes. In some cases, restoration or compensation of blood circulation occurs due to developed networks of collaterals, but they are not always durable.
Stages of disease development
The development of circulatory disorders in the system of vertebrobasilar arteries in osteochondrosis of the cervical spine can be conditionally divided into the following stages:
- Initial or stage of development of dyscirculatory encephalopathy (slowly progressive and/or diffuse damage to blood vessels, small arteries and arterioles of the brain). The patient is worried about dizziness, headaches, decreased attention and memory, difficulty maintaining balance, sleep disorders, fatigue, dysfunction of the organs of vision and hearing. There is a loss of cognitive, spastic, vestibular and autonomic functions.
- Subcompensation or the stage of pronounced neurological disorders, when the symptoms of the disease gradually increase and the patient’s well-being worsens. This is expressed in disorders of thinking and the ability to control subtle sequential movements, slower speech and chewing, deepening of the voice, constant changes in blood pressure, apathy, emotionally depressed state, etc.
- Late stage (decompensation) or stage of development of irreversible disorders in the central nervous system. At this stage, the patient practically becomes disabled, as he loses the ability to care for himself. He develops vascular dementia (dementia), affective disorders, parkinsonism, hypokinesia, involuntary laughter or crying, and quite often there is no ability to control urination and defecation.
Diagnosis and treatment of circulatory disorders in cervical osteochondrosis
A preliminary diagnosis is made during the initial examination of the patient by a neurologist and after collecting the clinical picture. The level of damage to the intervertebral discs is determined after an X-ray of the spinal column. Compression or damage to blood vessels, vascular beds, and nerve endings can be seen on an MRI or CT scan.
Pathologies of the spinal cord or brain are diagnosed using myelography with the introduction of a contrast agent. Dopplerography and ultrasound examination of cerebral vessels makes it possible to determine the patency of the channels and the speed of passage of blood fluid through them.
Treatment of cerebral circulatory disorders with cervical osteochondrosis depends on the location of the pathology, the severity of the lesion and the causes of the disease. First of all, conservative therapy is aimed at improving the patient’s condition (restoring and improving metabolic processes in the body and activating the regeneration processes of damaged cartilage tissue). For these purposes, the following are used: exercise therapy, massage sessions and physiotherapeutic procedures, adequate physical activity, and various water procedures.
Surgical methods of treatment are used quite rarely and only in cases where the patient’s condition sharply worsens or there is a threat to the normal functioning of internal organs.
Special drug therapy, in addition to drugs that relieve pain, muscle spasms, inflammation and swelling of soft tissues in the treatment of classic osteochondrosis, consists of:
- vasoactive drugs that activate cerebral circulation and dilate blood vessels;
- neuroleptics and antidepressants that have a sedative, calming effect, reducing the degree of cognitive (dizziness, vomiting, sweating, etc.) manifestations;
- nootropic agents that improve metabolic processes in the brain, memory, perception, thinking, speech abilities;
- diuretics and antioxidants, which help reduce swelling and activate the body's regeneration processes;
- B vitamins, calcium supplements or other vitamin complexes that improve the condition of the central nervous system and the patient’s entire body.
At home, the patient is advised to reconsider his lifestyle, give up bad habits, devote more time to active recreation and activities, and try to control his weight.
It is advisable to do morning exercises every day, water procedures, special physical exercises, attend sports clubs or take daily long walks at a fast pace.
Follow a daily routine, alternating appropriate periods of stress and relaxation, eat properly and rationally. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
How to treat cerebral vascular atherosclerosis
Treatment of dyslipidemia begins with non-drug measures. Doctors recommend lifestyle changes - quit smoking, control weight, exercise, eat right (limit foods high in cholesterol). The diet for atherosclerosis of the blood vessels of the legs includes the consumption of whole grains, a sufficient amount of vegetables, fruits, fish, and seafood.
If there is no effect from non-drug measures, antihyperlipidemic drugs are prescribed. The main drugs for the treatment of atherosclerosis are statins. Their use significantly improves the prognosis of life of patients with atherosclerosis. Studies have shown that drug therapy helps reduce low-density lipoprotein (LDL) cholesterol by 20% and total cholesterol by 26%. Mortality with regular use of statins is reduced by 22%.
Atherosclerosis is a systemic disease; despite different pools, it is treated pathogenetically in the same way - Statins, GI sequestrants (if statins are ineffective or contraindicated). And also symptomatically, depending on the area of the lesion and the severity of atherosclerotic stenosis of the atreria. For critical stenoses, surgical intervention is recommended, the type of which is determined by surgeons together with cardiologists
Read more about how to treat cerebral vascular atherosclerosis on our website.
Related services: Cardiac Check-up Diagnosis of heart rhythm disorders by ECG monitoring
Vascular headache
It is important to understand that the term “vascular headache” is not an official designation for any disease. However, patients often hear from their doctors about “vascular” pain.
In our country, “vascular pain” refers to vegetative dystonia, migraine, headache due to high blood pressure and impaired venous outflow. At the same time, “vegetative dystonia” in itself is also not a correct diagnosis, but in practice this diagnosis is made and various neurological problems are blamed on it.
The bad thing is that, using such a general term, the doctor himself often does not delve into the details. As a result, an inaccurate diagnosis leads to the choice of incorrect treatment.
Primary and secondary pain
Although the diagnosis “vascular headaches” is not entirely correct, no one disputes that blood vessels are often involved in the development of headaches. However, a violation of vascular tone or damage is NEVER the only cause of a headache, but only one of the stages in the development of a painful episode! The appearance of pain is always the result of a complex cascade of reactions from all body systems (cardiovascular, endocrine, nervous and others).
Diagnosis of vasculitis
The earlier the examination is carried out, the diagnosis is established and treatment is started, the greater the chances of avoiding damage to vital organs and disruption of their functions.
If necessary, consultations with a vascular surgeon, therapist, ophthalmologist, neurologist, otolaryngologist, etc. are scheduled.
The diagnosis is made based on a number of data:
- physical examination;
- laboratory tests.
Tests for vasculitis (see also rheumatological examination)
The following tests are required:
- general blood test (usually an increase in ESR is noticed);
- biochemical blood test (protein fractions, etc.);
- immunological tests (gamma globulin, C-reactive protein, rheumatoid factor, ANCA, etc.);
- blood for HBsAg if viral hepatitis is suspected.
In addition, instrumental methods such as:
- Doppler ultrasound;
- radiography;
- angiography (examination of blood vessels using X-ray contrast agents);
- CT scan.
1 General blood test
2 Doppler ultrasound
3 Plasmapheresis procedure
Who is at high risk?
If the following unfavorable factors are present in the patient's medical history, severe vascular complications of coronavirus are most likely, especially in combination with pneumonia:
- Chronic diseases of the cardiovascular system (myocarditis, hypertension, atherosclerotic plaques);
- Concomitant blood clotting diseases;
- History of strokes, heart attacks and other vascular accidents;
- Post-existing cytokine storm;
- Genetic thrombophilia, hidden predisposition to thrombosis;
- Hereditary predisposition to hyperhomocysteinemia, increased levels of homocysteine in the blood;
- Previous acute respiratory distress syndrome (ARDS);
- Treatment in the intensive care unit;
- Chronic diseases of the endocrine system affecting blood clotting;
- Antiphospholipid syndrome;
- Overweight;
- High cholesterol;
- Increased hemoglobin;
- Chronic rheumatic diseases;
- Pancreatitis;
- Leukemia;
- Hepatitis;
- Diabetes;
- Renal, cardiac, respiratory failure.
Even after recovery, especially if the patient was seriously ill, such patients are not immune from hidden problems with blood vessels that may appear in the future.