Tortuosity of the carotid and vertebral arteries to their deformation, abnormal weaving or curvature.
As a rule, such phenomena are congenital. The heredity of the pathology lies in the predominance of elastic fibers over collagen, as a result of which the walls of the arteries wear out faster and begin to deform. Also, pathological tortuosity of the carotid arteries can develop as a result, for example, of long-term hypertension or atherosclerosis.
The definition of “pathological” refers to the threat that arterial tortuosity can pose to human health and life. Obstruction of blood supply due to pathological deformations of the carotid and vertebral arteries leads to the development of the threat of stroke .
Types of disease
The following types of pathological tortuosity of the carotid and vertebral arteries are distinguished:
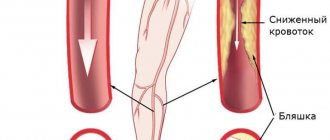
- lengthening of the artery . The most common is elongation of the internal carotid or vertebral artery, which leads to the formation of bends along the vessel. An elongated artery rarely causes concern and is often discovered only during random examination. With age, the elasticity of the arterial wall changes, and the bends of the artery can become kinks, with the development of cerebrovascular accidents;
- kinking - bending of an artery at an acute angle. Kinking can be congenital, but arterial hypertension or progressive atherosclerosis in the internal carotid artery can also contribute to the appearance of kinks. Kinking of the carotid artery is manifested by transient disturbances of cerebral circulation. With kinking of the vertebral artery, vertebral-basilar insufficiency develops (a reversible disorder of brain function caused by a lack of blood supply);
- coiling is the formation of a loop in the carotid or vertebral artery, leading to significant changes in blood flow in it. The nature of the bends during coiling can change depending on body position and blood pressure. The blood flow becomes chaotic, which leads to a decrease in blood pressure after the loop and, accordingly, to a decrease in blood supply to the brain.
Pathological tortuosity of the carotid arteries
January 6, 2016
One of the most poorly understood and mysterious diseases of the carotid and vertebral arteries is pathological tortuosity (kinking). In every third person who died from a stroke, pathological bends of the carotid or vertebral arteries were found. In 16-26% of the adult population, various variants of elongation and tortuosity of the carotid or vertebral arteries in the neck are detected. The cause of tortuosity is most often congenital, but often elongation of the artery develops with hypertension. For a long time, tortuosity may not produce any symptoms, but at some point the patient begins to experience transient cerebrovascular accidents. The angiosurgeons of our clinic are focused on developing the problem of pathological tortuosity of the carotid and vertebral arteries.
Types of pathological tortuosity of the carotid arteries
Lengthening the artery. The most common is elongation of the internal carotid or vertebral artery, which leads to the formation of smooth bends along the course of the vessel. An elongated artery is rarely a cause of concern and is usually discovered during random examination. Lengthening the artery is important for ENT doctors, since the artery wall may be abnormally close to the palatine tonsils and may be accidentally damaged during tonsillectomy. With age, the elasticity of the arterial wall changes and smooth bends of the artery can become kinks, with the development of a picture of cerebral circulation disorders. When arteries are lengthened without kinks, ultrasound examination of blood flow does not detect any disturbances. Kinking is a bend in an artery at an acute angle. Kinking can be congenital, when cerebral circulation disorders are detected from early childhood and develop over time from an elongated carotid artery. The formation of kinks is promoted by arterial hypertension and the progression of atherosclerosis in the internal carotid artery. Clinically, kinking of the internal carotid artery is manifested by transient disturbances of cerebral circulation. With kinking of the vertebral artery, vertebrobasilar insufficiency develops. Identification of kinking with brain symptoms raises the question of surgical correction of tortuosity. Coiling is the formation of a loop of an artery. Despite the smooth movement of the loop, changes in blood flow in it are very significant. The nature of the bends during coiling may change depending on body position and blood pressure. A chaotic nature of the blood flow is observed, which leads to a decrease in blood pressure after the loop and, accordingly, to a decrease in blood flow through the cerebral arteries. If a person has a well-developed circle of Willis on the lower surface of the brain, then he will never know about the existence of a loop or inflection. The appearance of symptoms of cerebral circulatory failure indicates disturbances in blood flow compensation and dictates the need for detailed examination and treatment.
Clinical manifestations
Manifestations of pathological tortuosity are varied, the most common are: - A picture of transient ischemic attacks in the blood supply of a tortuous artery with temporary paralysis of half the body or arm (hemiparesis), speech impairment, etc.); — Temporary blindness in one eye; - Noise in the head; - Dizziness; - Flashing before the eyes; — Headaches without clear localization; — Short-term loss of consciousness; — Falls without loss of consciousness; — Temporary imbalances; - Migraine-like attacks.
Treatment of pathological tortuosity
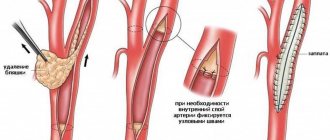
Pathological tortuosity is subject to surgical treatment. The artery straightens out, its excess is cut off, and patency is restored. The results of surgical treatment are good. Symptoms of cerebral vascular insufficiency completely resolve in 96% of patients. The risk of operations is less than 1%. Operations can be performed under local anesthesia. Drug treatment of pathological tortuosity is not effective, since the artery cannot straighten out from the drugs. It is important to clearly define the diagnosis of pathological tortuosity and prove its importance for cerebral circulation. Then the results of treatment will please both patients and their doctors.
Symptoms
The symptoms of pathological tortuosity of the carotid and vertebral arteries are varied. The most common symptoms are:
- so-called transient ischemic attacks (temporary interruptions in blood supply), accompanied by temporary paralysis of the upper limbs, speech impairment, temporary blindness;
- noise in the head, dizziness;
- migraine attacks;
- impaired coordination of movements, falls without loss of consciousness;
- short fainting spells.
Vertebral artery syndrome (Barre-Lieu) - symptoms and treatment
For chronic neck pain, surgical and pharmacological treatment methods are used, as well as various methods of traction therapy —spinal traction with the help of special devices (blocks, belts, rings) [12].
The effectiveness of manual therapy methods - soft techniques, post-isometric relaxation, muscle stretching - is still being studied. To this end, two studies were conducted in 2015. A meta-analysis by Chinese scientists showed that manual techniques are less effective in eliminating pain than cervical spine traction [13]. However, a study by Canadian scientists found that manual therapy becomes more effective when combined with another method of active treatment for acute and chronic neck pain. Also, manual techniques cope better with chronic pain than massage, and more effectively combat acute and subacute neck pain than drug treatment. However, due to side effects from taking medications, manual therapy is preferable. In terms of effectiveness, manual techniques are similar to mobilization of the cervical spine, but mobilization as a separate intervention does not reduce pain [14].
As for the non-drug treatment method of acupuncture , a 2021 meta-analysis showed its effectiveness over sham acupuncture (acupuncture of non-acupuncture points) and inactive treatment [15].
An undoubted effective method of treating the syndrome is physical exercise . Their effectiveness in relieving acute and chronic pain is supported by a 2005 review. In this case, it is worth focusing on stretching the cervical region, shoulder girdle and chest. And the combination of exercises with mobilization and manual techniques on the cervical spine helps reduce pain in the short and long term [16].
Surgical methods include :
- puncture interbody fusion - combining and fixing several vertebrae to avoid their displacement;
- fenestration - partial removal of the arch of the intervertebral disc;
- autodermoplasty of intervertebral discs - replacement of the disc with one's own tissues.
During the operation, porous explants made of an alloy of titanium and nickel are implanted. Due to their porosity, bone tissue quickly grows in them. This makes the fixation strong and significantly reduces the patient’s period of incapacity for work and the neck being in a stationary position.
In addition to stabilizing operations of the cervical spine, other types of interventions are also performed:
- decompressive-stabilizing - removal of compression with subsequent fixation of the spine;
- decompressive-plastic (laminoplasty) - elimination of compression by enlarging the spinal canal while maintaining the integrity of the posterior elements of the vertebrae;
- decompressive operations - removal of the intervertebral disc or its arch, compressing the artery, etc. [9].
There is considerable experience in reconstruction of vertebral arteries . The following methods are used:
- transposition - displacement of the vertebral artery into the subclavian (common carotid);
- angioplasty - dilation of a vessel using an expanding balloon;
- Stenting is the expansion of a vessel by installing a stent.
If the first and second segments of the vertebral artery are simultaneously affected, bypass surgery is performed—creating a bypass at the level of the third segment [17].
What is non-straightness of the vertebral arteries?
The vertebral arteries stretch from the prevertebral to the intracranial region, passing through the canal of the transverse processes of the cervical portion of the spinal column. If a person has received any injury, has a curvature of the spine or other diseases, this also affects the vertebral artery - it becomes bent. Blood flow is disrupted, the occipital part of the brain does not receive enough nutrition and oxygen. Irregular tortuosity of the artery is called “non-straightness of the VA”. In most cases, both arteries are affected, but non-straightness of the left vertebral artery or non-straightness of the right vertebral artery may also occur. This happens after a serious injury or the growth of a bone callus.
When a person has a non-linear course of VA on both sides, it is easier to make a diagnosis, and clear symptoms of the disease appear. If this pathology develops only on one side, the body tries to cope with the problem itself by increasing blood flow in the other vertebral artery. In this case, there will be practically no symptoms of the disease, but if the patient was examined for another disease, the doctor may notice this deviation.
Tortuosity of the main arteries of the head as a risk factor for cerebral ischemia
The relevance of studying cerebrovascular diseases is explained by their very wide prevalence, while 2/3 of ischemic strokes (IS) are associated with damage to extracranial arteries, primarily of atherosclerotic origin. However, until now, not all experts pay due attention to the role of anomalies and deformations of the carotid (CA) and vertebral arteries (VA) in the genesis of acute cerebral ischemia. The lengthening and tortuosity of the arteries are the result of their adaptation to the pathological conditions of regional circulation. A well-known fact is the combination of complete occlusion of the carotid artery on one side with the expansion and tortuosity of the opposite side, through which the blood flow increases significantly and at the same time the load on the walls of the vessel increases, which over time leads to its bending. Arterial hypertension has a greater influence on the formation of tortuosity, which accelerates the process of vessel deformation in the form of its tortuosity. In diseases leading to shortening of the cervical spine, a “relative” lengthening of the carotid and vertebral arteries occurs. Tortuosity can be congenital, often combined with other vascular anomalies (such patients have various variants of mesenchymal dysplasia - false chord of the left ventricle, mitral valve prolapse, Kimmerle anomaly, varicose veins, myopia, flat feet, etc.). When turning the head, in cases of tortuosity of the arteries, due to their kinks, the development of IS is possible, occurring according to the hemodynamic type (formation of septal stenosis at the site of kinks with a reduction in blood flow distal to the stenosis). Thrombotic genesis of acute ischemia is also possible due to the formation of wall thrombi in places of long-existing kinks and loops with the development of arterio-arterial embolism. A number of experts are of the opinion that various types of tortuosity are observed in any vascular pathology of the brain, and only under special conditions can they lead to IS. Some researchers recognize the presence of tortuosity of the brachiocephalic arteries (BCA) as an independent factor in the development of IS. A minority denies the role of configurational anomalies in the genesis of cerebrovascular symptoms. Several years ago, on the basis of three neurological departments of Clinical Hospital No. 1, the hospital’s neurologists, together with angiosurgeons, conducted a study that made it possible to assess the characteristics of cerebral blood flow in patients who had suffered IS against the background of tortuosity of the cerebral artery; to determine the signs indicating the pathological nature of the tortuosity, to clarify the selection criteria for patients with tortuosity of the MAG for reconstructive operations, the task of which is to restore normal main blood flow. Using large clinical material (592 patients), we have shown that there is selectivity in the effect of different types of tortuosity on cerebral hemodynamics. The results of the study showed that in 89% of patients who suffered a stroke and transient ischemic attack, tortuosity of the main arteries of the head was detected, of which hemodynamically significant in 27%. MAG tortuosity predominated in the age group under 40 years and over 70 years, mainly in women. They were significantly more common in the vertebral arteries. The criterion for hemodynamically significant tortuosity of the extracranial part of the vessel was taken to be an increase in linear velocity (LVR) at the internal radius of tortuosity by more than 2 times from the LSV values before the tortuosity, as well as the presence of turbulent blood flow in the area of tortuosity. According to MRI, the following types of tortuosity were identified: “C” or “S”-shaped tortuosity, looping - coiling, bending of the vessel at an acute angle with the formation of septal stenosis - kinking. Neurological manifestations in patients with ICA tortuosity: syncope, often complaints of tinnitus, sleep disturbances, attention disorders, pain in the eyeballs. Clinically, TIAs were manifested by transient visual disturbances such as hemianopsia, photopsia, monocular blindness, hemiparesis and monoparesis, speech disorders such as aphasia (sensory, motor), and sensory disorders of the hemitype. Patients in this group often had cerebroasthenic manifestations, vestibulopathy, and psycho-vegetative syndrome. Patients with VA tortuosity are characterized by fainting, headaches of occipital localization, dizziness, and hearing disorders that arise or worsen when the position of the head changes. TIAs predominated; ISs occurred in patients with TIAs in the vertebrobasilar region and were manifested by a combination of transient motor disorders; paresthesia of half the face and (or) torso, limbs; visual disorders (homonymous hemianopia, diplopia); attacks of dizziness (often accompanied by nausea, less often - vomiting); speech disorders such as dysarthria; ataxia, instability. The most common tortuosity of the VA was found in the V1 and V3 segments, which makes reconstructive operations accessible. In most cases, ischemic foci were detected in the blood supply area of the altered vessel. However, in 16%, the localization of the stroke was in the area of blood supply to the intact vessel ipsilaterally or in the contralateral hemisphere. In cases where the ischemic focus did not correspond to the zone of vascularization of the altered vessel, anomalies in the structure of the circle of Willis were detected. Patients with hemodynamically significant tortuosity, a history of TIA, and the absence of focal changes in the brain substance on neuroimaging underwent PET to assess the level of metabolism. In the majority, foci of metabolic depression were identified, which represent the volume of future cerebral infarction. Foci of decreased metabolism were localized in the ipsilateral hemisphere with a normal structure of the circle of Willis and in the contralateral hemisphere with a disconnected circle of Willis. Features of changes in cerebral blood flow during hemodynamically significant tortuosity are local hemodynamic disturbances in the area of tortuosity in the form of turbulence. The most pronounced local hemodynamic disturbances in tortuosity are in the form of kinking and coiling. Changes in head position provoke the occurrence of septal stenosis, leading to a reduction in blood flow distal to the tortuosity. Interhemispheric asymmetry of the LSC is characteristic, with its increase on the tortuosity side. In most cases, there are anomalies in the structure of the circle of Willis, and therefore there is no possibility of adequate functioning of the collaterals. Clinical features of ischemic brain lesions with pathological tortuosity of the cerebral artery are the predominance of transient ischemic attacks and strokes of the “small” type with moderate neurological deficit and rapid recovery of functions, as well as the occurrence of cerebrovascular symptoms when the position of the head changes. In the anamnesis of patients with pathological tortuosity, syncope and fainting are common. The results obtained made it possible to determine the criteria for pathological tortuosity of the MAG - this is a hemodynamically significant tortuosity, manifested by symptoms of cerebral circulatory disorders in the given or opposite vascular basin, which depends on the structural features of the circle of Willis, provided there is no significant atherosclerotic lesion of the tortuous vessel. 80% of patients with MAG tortuosity suffered from hypertension, and in 30% of cases the diagnosis of hypertension was first established after the onset of stroke symptoms, i.e. arterial hypertension remained latent for a long time. The most effective measure of secondary prevention of pathological tortuosity of the MAG is surgical treatment. The main indication for surgical treatment should be the recognition of tortuosity as pathological.
The problems of treatment and prevention of cerebrovascular diseases remain among the most pressing, since cerebral circulatory disorders continue to occupy a leading position among the causes of persistent disability and mortality throughout the world. Vascular diseases of the brain are the main cause of ischemic stroke. It has been proven that lesions of the extracranial parts of the internal carotid (ICA) and vertebral arteries in 65-70% of cases lead to ischemic disorders of cerebral circulation. Pathological deformations (PD) of the ICA are one of the most common diseases of the brachiocephalic vessels, second only to atherosclerosis in frequency. ICA PDs lead to cerebral circulatory disorders of varying severity [1–6]. The overall incidence of ICA PD among the adult population, according to the results of angiographic and pathomorphological studies, varies from 10 to 40%. In children with manifestations of brain failure, this pathology occurs in 14-30% [2, 7, 8].
The etiology and pathogenesis of ICA PD are not fully understood. Most authors believe that their origin may be congenital or acquired. Evidence of the congenital origin of PD of the ICA is the presence of deformations of the carotid arteries in childhood and young age, frequent bilateral lesions, a combination of lesions of the carotid arteries with other manifestations of systemic connective tissue dysplasia [9-11] - Marfan and Elars-Danlos syndromes [12], coarctation of the aorta, vascular hypoplasia [13-16]. The causes of acquired PD are considered to be weakening of the elastic frame of the artery wall, atherosclerosis, age-related changes in the cervical spine, hypertension, diabetes mellitus, and obesity [1, 2, 5, 17, 18].
Congenital PD of the ICA
occupy 1st place among the causes of cerebrovascular accidents in childhood. According to Yu.V. Smirnova [8], ICA PDs occur in 26.9% of children with neurological symptoms. M.A. Lobov et al. [7] identify PD as one of the main causes of vasopathic headaches in childhood, recording them in 1/3 of cases. The incidence of PD in boys and girls is comparable.
Initial manifestations of cerebrovascular insufficiency usually occur in children 4-6 years old. These include delayed speech development, late formation of self-care skills, impaired adaptation in a team, hyperexcitability and irritability. Later, at 5-6 years of age, headaches appear. The described symptoms are nonspecific and can mask vascular anomalies of the carotid arteries, so ultrasound examination of the neck vessels is mandatory in the presence of such a clinic. Acute cerebrovascular accidents in children occur quite rarely: transient cerebrovascular accidents - in 4.3% of cases, ischemic stroke with the development of focal lesions of the brain substance is observed even less often - in 2.1% [7, 8, 10, 15-17] . A feature of the clinical picture of PD in children is epileptic seizures (in 19.3% of cases).
The predominant types of ICA PD are couling, C- and S-shaped tortuosity (20-30%). This is explained by intrauterine development disorders [1, 13, 18-20]. Back in 1925, A. Kelly [21] believed that loops are formed at the 5-6th week of embryo development. The ICA originates from the third branchial arch and the dorsal aorta, at the junction of which a distinct bend is formed, which appears in a 5-week embryo. In the process of further development of the fetus, due to the lowering of the heart into the chest cavity and its vertical rotation along the axis, the carotid artery straightens. If this straightening or turning is incomplete, this leads to the formation of bends, loops, and kinks of varying degrees of severity. Another contributing factor to the deformities may be the more pronounced growth of the arteries of the aortic arch compared to the growth of the neck. This is confirmed by the presence of tortuosity of the ICA in embryos and children at the level of the glossopharyngeal nerve [13, 19]. The frequency of such anomalies in newborns ranges from 5 to 10% [2, 10, 11].
There are no data in the literature on the etiological factors leading to disembryogenesis and the development of congenital vascular deformations. It should be noted that bends and loops can also be found in the cerebral, coronary, retinal and vertebral arteries, but they are more often acquired. Bends of the coronary arteries are associated with hypertension and myocardial infarction, retinal arteries with retinopathy in malignant hypertension and diabetes mellitus, capillaries of the muscles and heart with arterial hypertension and diabetes mellitus, and veins with varicose veins [22].
B. Callewaert et al. [23] describe a special “arterial tortuosis syndrome”. This is a congenital disease with an autosomal recessive mode of inheritance (defect of the SLC2A10
), which is characterized by tortuosity, elongation and the formation of aneurysms of large arteries due to disruption of the structure of the elastic fibers of the media of the vascular wall. The combination of tortuosity and arterial aneurysms is the main feature of Loeys-Dietz syndrome, a congenital disease with a mutation in the TGF β receptor. In this case, the aneurysm is primary and becomes the background for the development of tortuosity.
Yu.V. Smirnova [11] proved that the trait of tortuous ICA can be inherited in an autosomal dominant or autosomal recessive manner. An association has been established for the A80807T polymorphism of the transcription factor 8p4
with pathological tortuosity of the carotid arteries. The probability of having PD ICA in A80807/A80807 homozygotes is 1.64 times higher compared to carriers of the other two genotypes (A80807/T80807, T80807/T80807).
M.A. Lobov et al. [10, 24] also indicate the hereditary determination of ICA PD in children. According to them, the frequency of familial cases is 50%. Segregation analysis of these cases demonstrates that ICA PD can be either isolated or a manifestation of hereditary syndromic connective tissue pathology. The segregation frequency is 45% [24]. Researchers regard hypoplasia, aplasia and anomalies in the position of arteries as nonspecific signs of dysembryogenesis and classify them as precerebral angiodysplasias.
In recent years, the role of congenital connective tissue deficiency in the formation of ICA PD has been discussed. Clinical observations of a combination of elongation and deformation of the carotid and vertebral arteries with phenotypic signs of hereditary connective tissue pathology, Elars-Danlos, Marfan, Sturge-Weber syndromes are presented [5, 9, 12, 15]. At the same time, combinations of ICA PD with the above syndromes are described in isolated cases. It should be noted that there is a higher incidence (60%) of minor forms of connective tissue dysplasia in children with PD ICA, such as joint hypermobility, skin hyperextensibility, muscle hypotonia, poor posture, flat feet, mitral valve prolapse, abnormal chordae, abnormal growth and development of teeth. However, the degree of “phenotypic intensity” of the signs does not reach the severity corresponding to the established criteria for diagnosing connective tissue pathology syndrome [24]. Therefore, the question of whether ICA PD in children can be considered a manifestation of connective tissue dysplasia syndrome remains open.
The pathomorphological signs described by P.O. support the dysembryogenetic theory of the origin of the ICA PD. Kazanchyan et al. [1], including degenerative changes in elastic fibers, compensatory hyperelastosis, multiplication of the internal elastic membrane, development of mucoid edema, proliferation of smooth muscle cells.
The most acceptable hypothesis for the pathogenesis of carotid artery anomalies is the appearance of defects in the structure of elastin and collagen due to an endogenous or genetically determined increase in the activity of degradative enzymes - collagenase and elastase [20, 25-27]. It is advisable to emphasize that the same changes in the structure of elastin and collagen are considered the main pathogenetic factor in the development of vascular pathology - both congenital and acquired.
A possible reason for the development of ICA PD in children may be birth trauma or overstretching of the neck structures during childbirth. It is known that collagen fibers under conditions of uniaxial tension are the main factor preventing deformation. Collagen concentration correlates positively with tensile strength and negatively with maximum elongation. The experiment proved that when collagen is removed from the vascular wall, the tensile strength and rigidity decrease, and when elastin is removed, the wall strength and relative deformation decrease. The significant content of elastin in the wall of the carotid artery determines its greater elasticity reserves compared to the vertebral artery. O.V. Kalmin [28] proposed a hypothesis about the sequence of damage to neck structures during hyperextension, hyperflexion and longitudinal stretching during childbirth. Nerve trunks have relatively low extensibility and the least rigidity, and the wall of the common carotid artery (CCA), on the contrary, has the greatest extensibility and the least rigidity. With hyperextension, the phrenic nerve is at greatest risk of injury, followed by the vagus nerve, and damage to the carotid artery wall is unlikely. With hyperflexion, the spinal cord can be damaged first, and only after the spinal ligaments are torn, massive damage to the arterial walls will occur. With longitudinal stretching of the neck, the main part of the deforming load will fall on the vertebral trunk and its ligaments, then the nerve trunks, the vertebral artery and, lastly, the carotid artery. The greatest reserve of lengthening - 33.8%, without disturbing the structure and functions of the neck structures, is found in the OCA. Based on the above, it follows that damage to the CCA during childbirth is unlikely [1, 18]. At the same time, the ICA remains outside the attention of researchers. During longitudinal stretching during childbirth, the greatest load, in our opinion, occurs at the site where the carotid artery enters the skull, which can lead to the development of deformities.
The question of the advisability of surgical intervention for ICA PD in children remains open. There is evidence that in some children, during the process of growth, the straightness of the course of the vessel is restored, and in some patients, the deformity remains with the leveling of local hemodynamic disturbances [1, 8]. It should be taken into account that generalized epileptic seizures, which often occur with anomalies of the carotid arteries, are a contraindication to surgery [6, 8, 11]. Conservative therapy is still considered the priority direction for treating children [7, 15, 17]. If it is ineffective, neurological symptoms increase and the rate of cerebral blood flow decreases, surgical intervention is necessary. Reconstructive elimination of deformity leads to a reduction in the manifestations of chronic brain failure in the immediate postoperative period in all patients [2, 4]. At the same time, among the literature data, we did not find any scientific studies assessing the impact of surgical or conservative treatment of children with ICA PD on their quality of life in the postoperative period.
Acquired pathological deformations of the ICA occupy 2nd place among the causes of ischemic cerebrovascular accidents, second only to atherosclerosis [1, 4-6, 18, 20, 22, 25]. ICA PDs occur predominantly in patients over 60 years of age. It is believed that kinking is detected in 5-16% of patients, more often in men [1, 4, 29, 30], although there are reports of predominant lesions in women, which is explained by damage to the elastic framework of blood vessels associated with hormonal changes [31-33] . L. Del Corso et al. [34] based on a study of 469 patients with PD (tortuosity, kinking and bending) confirm the high incidence of lesions among women. E. Ballotta et al. [35] believe that in women, asymptomatic carotid kinking progresses with age and becomes symptomatic after 60 years. R. Zanetti et al. [6] indicates that in adults, changes in the length and shape of the carotid arteries most often appear in the sixth decade of life, with a male to female ratio of 4:1. Perhaps such disagreements are associated with the presence of concomitant pathologies in patients - atherosclerosis, hypertension, diabetes mellitus, hyperlipidemia, hormonal changes, as well as the influence of toxic substances and smoking.
The clinical picture is characterized by cerebrovascular accidents. The most common symptoms are dizziness, cochlear, sensory and cognitive impairment, and ischemic retinopathy. Symptoms of cerebral ischemia in the hemisphere on the side of the ICA tortuosity occur in 26% of patients, cerebral manifestations in 41.75%, and their combination in 27.5%. There is evidence that the clinical picture depends on the type of ICA PD. C- and S-deformations most often occur asymptomatically - about 70% of cases; kinking, loop- and spiral-shaped tortuosity have pronounced clinical symptoms - in more than 80% of cases [18, 35, 36]. The development of symptoms also depends on the severity of the angle in the kinking segment - the sharper the angle, the more severe the lesions. When the angle is less than 45°, all patients experience severe brain symptoms requiring surgical intervention [18, 19, 36].
Among the types of ICA PD, kinking, elongation, and kinks are most often described, which is associated with the peculiarities of the origin of acquired deformities. So, Z.K. Mackevicius et al. [37] identify a group of causes of ICA PD, dividing them into 2 subgroups. The first is a bend at the site of the carotid artery in the area where the atherosclerotic plaque ends, the second is bends and deformations based on age-related destructive changes in the muscular-elastic frame of the arterial wall. Arterial hypertension that appears with age contributes to the worsening of PD, since vascular deformations become a functional device to reduce the pulse wave and ensure uniformity of blood flow [4, 19, 25]. However, P.A. Pauliukas and E.M. Barkauskas [29] believe that in these cases hypertension is secondary, has a reflex nature and develops in response to cerebral ischemia. As hemodynamic studies show, when kinks and loops of brachiocephalic vessels are eliminated, systemic blood pressure decreases [5, 9, 18, 25].
According to N.V. Vereshchagin and A.N. Koltover [20], hypertension is the primary cause of ICA PD. In response to increased pressure in the walls of the carotid arteries, adaptive changes occur in the form of focal and circular muscular-elastic thickening of the intima, sclerosis of the inner and middle membranes with destruction of the elastic frame. As sclerotic changes develop, the muscular and elastic elements of the arteries are lost, their tone is lost, resulting in the formation of pathological tortuosity and kinks of these vessels with pronounced septal stenosis against the background of arterial hypertension. The latter, by limiting blood flow, can act as an independent pathogenetic factor in cerebrovascular accidents. Hypertension, according to J. White et al. [27], leads to stretching of the smooth muscle cells of the vessel media, loss of elastin and fragmentation of elastomers. The progression of these processes causes pathological lengthening of the vessel. Data from P. Pancera et al. [38] demonstrate a clear predominance of hypertension in patients with kinking compared with individuals without vascular anomalies. However, D. Radak et al. [39] believe that there is still no clear understanding of the pathogenetic relationship between known vascular risk factors and the development of kinking.
The main reason for the development of acquired ICA PD in patients over 60 years of age is atherosclerosis. The question remains open: what comes first, atherosclerosis or PD? There is no consensus among researchers on this matter. Some believe that atherosclerosis leads to the development of destructive changes in the elastic framework of the vessel and, together with arterial hypertension, contributes to the development of deformations, such as elongation and kinking [4-6, 19, 20, 22, 31, 32, 37, 40-42]. Other authors call atherosclerosis an aggravating disease in ICA PD. Disruption of local hemodynamics in the bending zone of a deformed vessel leads to intimal injury, damage to the endothelium and the initiation of the pathological process [1, 5, 20, 29, 34, 38]. Based on this, early atherosclerosis should develop in the carotid arteries, clinically and angiographically manifested before the age of 40 years, which is not confirmed by literature data [2, 19, 37, 40, 41]. Other researchers have proven that when bending, a pressure difference is created at the outer and inner radius, leading to the development of turbulence in hemodynamic flows and, as a consequence, the growth of endothelium and connective tissue in the vessel. At the same time, signs of proliferative sclerotic remodeling are found in the vessel due to activation of the immune system - high apoptotic activity of smooth muscle cells and the development of chronic inflammation in the tortuosity zone [42]. At the same time, in a series of morphological studies there is no data on inflammation and the presence of vasculitis [20, 37, 38, 43].
It is important that it is atherosclerosis in PD that increases the risk of stroke several times. This combination is observed in 40-70% of patients with cerebrovascular accidents [1, 4, 19, 22, 31, 34, 38, 41, 43].
Fibromuscular dysplasia is considered one of the important causes of the development of ICA PD. There are no exact data on the incidence of dysplasia in PD ICA. It is believed that fibromuscular dysplasia and PD of the ICA occur more often in middle-aged people, although there is data on patients over 60 years of age. The mechanism of development of deformations of the carotid arteries in this disease is unknown. Fibromuscular dysplasia is a non-atherosclerotic and non-inflammatory arterial disease with predominant involvement of the renal arteries and ICA, developing predominantly in young women. The predominant pathomorphological variant of carotid artery lesions in fibromuscular dysplasia without PD is medial fibroplasia. It is characterized by fibrosis with partial or total damage to the media, complete or partial loss of elastic fibers. This leads to the formation of multiple aneurysms, as a result of which the vessel resembles a “string of beads.” In addition to the development of aneurysms, vascular dissection, occlusion of the vascular lumen, and vascular ruptures are possible. It can be assumed that the commonality of the pathological process in fibromuscular dysplasia and PD of the ICA—the loss of the elastic framework of the vessel—is probably a significant factor for the development of pathological bends in fibromuscular dysplasia [44–47].
Age-related changes in the vertebrae of the cervical spine are considered an important factor in the development of acquired ICA PD. Vertebrogenic compression contributes to hemodynamic disturbances and the development of ICA PD. In patients with tortuosity, there is a forward displacement of the head, smoothing of the cervical lordosis, kyphosis in the thoracic region, and pronounced tension in the sternocleidomastoid, scalene muscles, and muscles located above and below the hyoid bone. Shortening of the muscles of the anterior surface of the neck and deformation of the fascia lead to extravasal effects on the carotid and vertebral arteries [18, 48]. Thus, mechanical deformations of the fascia against the background of disorders in the cervical spine can be considered as one of the reasons for the formation of arterial deformities. R. Wirbel et al. [49] proved that hyperextensional and rotational effects on the cervical spine, which occur during manual therapy sessions and sports, such as wrestling, can lead to damage to the vertebrobasilar vessels. A number of authors believe that although most injuries to the vessels of the neck occur for no apparent reason to the patient, minor trauma to the cervical spine is detected in 80% of cases [50]. With significant displacements of the vertebrae or their parts, sharp changes in the normal course of blood vessels are detected, while twisting, compaction and overstretching of the vertebral and carotid arteries are macroscopically observed.
Other causes of ICA PD include diabetes mellitus, hyperlipidemia and other vascular risk factors [2, 5, 6, 20, 34, 38, 41].
Possible factors contributing to the development of ICA PD include smoking, taking contraceptives, and toxic influences [5]. According to the new theory of D.D. Zerbino [51, 52], heavy metals damage the muscular-elastic framework of arteries and lead to the development of arteriosclerosis and arterial hypertension [51]. It has been proven that the toxic effects of cadmium lead to massive elastolysis of the media due to the activation of elastases and the development of aortic aneurysms. It is known that heavy metals contained in cigarettes cause irreversible changes in the coronary arteries, leading to the development of atherosclerosis and myocardial infarction in patients under 40 years of age. Smoking and many years of professional contact with toxic substances are important reasons for the development of vascular pathology in middle age.
Some authors mention vasculitis among the possible causes of the development of ICA PD in young patients [20, 37, 43]. Z.K. Matskevichus and P.A. Pauliukas [37] describe angiitis vasa vasorum
, which is explained by ischemic damage
to the vasa vasorum
with the development of inflammation and subsequent severe sclerosis.
The mechanism of development of ICA PD in patients aged 40–50 years remains unclear. The prevailing opinion in the literature is that they are a consequence of impaired embryogenesis [2, 5, 22, 32, 35, 43]. Based on the above, it follows that congenital deformities in children are characterized by loop-shaped deviations (cowling), C- and S-shaped tortuosities, and for patients over 60 years old - kinking, elongations and kinks. Whether it is possible to transition from one type of PD to another remains unexplored.
Yu.V. Rodin et al. [53], using mathematical modeling methods, a hypothetical assessment of the development of S-shaped tortuosity was given - any bend, under certain conditions, tends to an angular bend. The results obtained are also valid for other types of crimp, since they typically contain S-shaped crimp. At the same time, this hypothesis completely refutes the possibility of the transition of one type of tortuosity to another and requires further research.
The pathomorphological picture of ICA PD is characterized by pronounced sclerotic changes in the vessel wall, destruction of the elastic frame, and proliferation of connective tissue around the vessel [13, 20, 37, 38]. Since such changes contribute to stable irreversible deformities that increase with age, the question of whether changes in the configuration of deformities is possible remains open.
Surgical intervention is recognized as the most effective treatment method for acquired ICA PD. The indication for surgery is considered to be a hemodynamically significant PD of the ICA, commensurate with circulatory disorders characteristic of stenoses of 70% or more, regardless of the presence of neurological symptoms and/or hemodynamically significant atherosclerotic stenosis, as well as embologenic plaques that stenose the lumen of more than 50%, and plaques with pronounced surface and parietal thrombosis. The high effectiveness of surgical intervention in patients with symptomatic ICA deformities is known, while the question of the appropriateness of surgical intervention in patients with asymptomatic deformities remains open [1, 3, 4, 6, 19, 29, 35, 36, 42, 54].
In conclusion, we would like to mention that a comparative analysis of the literature on congenital and acquired ICA PDs showed that they have many distinctive features not only in origin and pathogenesis, but also in clinical presentation, treatment and prognosis. It is appropriate to assume that congenital and acquired ICA PD are two different diseases, the relationship between which has not been proven.
This review of the literature demonstrates the relevance of studying this disease, the presence of unresolved and controversial issues not only in the genesis, but also in the treatment tactics of patient management, and the need for a comprehensive clinical and pathomorphological study of this important vascular pathology.
"Kinking" syndrome of extracranial arteries of the brain
Back to program
Yunusov Kh. A., Sultanov D. D., Sadriev O. N.
RNCSSSH;
Purpose of the study. To study the results of reconstructive operations for pathological tortuosity of the carotid and vertebral arteries. Material and research methods. In the Department of Vascular Surgery of the Russian Research Center for Cardiovascular Surgery for the period 1995 – 2013. were treated with a diagnosis of “kinking” of the internal carotid artery in 27 patients and vertebral arteries in 12 patients. There were 26 men, 13 women. The average age was 41+4.2 years. The patients underwent a complex of research methods: ultrasound, duplex scanning, angiography. To determine the brain's tolerance to compression, the Matas test was performed. Research results. 85% of patients had a long history of hypertension. Among patients with “kinking” of the internal carotid artery (ICA), a history of stroke occurred in 4 patients, transient ischemia in 12, asymptomatic in 11. Kinking of the vertebral artery in all patients was manifested by a clinical picture of vertebrobasilar insufficiency, including in 4 – episodes of transient ischemic attack. According to angiography, according to angiography, various variants of “kinking” of the ICA were encountered: looping – 7, S-tortuosity – 15, tortuosity with one knee – 5. In 14 cases, “kinking” was combined with stenosis. High location of the “kinking” was noted in 5 cases. The tortuosity of the vertebral arteries in all cases had an S-shaped bend. Patients with “kinking” of the internal carotid artery were operated on under local or a combination of regional anesthesia. During kinking of the vertebral artery, general endotracheal anesthesia was used in all cases. The type of reconstruction depended on the shape and length of the “kinking”. In case of looping of the ICA, resection of the changed part of the ICA was performed with an end-to-end anastomosis (7); in other forms, the “kinking” was redressed with the imposition of an anastomosis in the area of the opening of the ICA. In 2 cases, the distal end of the resected ICA was anastomosed with the external carotid artery. Redressal of the “kinking” of the vertebral artery with reimplantation into the subclavian artery was performed in 8 cases. In 4 cases, due to excess length, the vertebral artery was implanted into the carotid artery. After surgery, in 1 case (2.5%) an ischemic stroke developed as a result of thrombosis of the anastomosis, in which the ICA was anastomosed with the external carotid artery. Conclusions. Thus, reconstructive operations for “kinking” syndrome of the great arteries of the brain are effective in preventing ischemic brain damage.
How to treat?
If you have non-straightness of the vertebral arteries, treatment depends on the severity of the symptoms. In the early stages, conservative treatment can also help. It is necessary to figure out what caused the pathology and first cure the underlying disease. If the cause of this pathology is a spasm of the cervical muscles, it needs to be removed. Physical therapy or massage may help. Conservative treatment did not help? Then the doctor prescribes surgery.
Drug treatment
The doctor also decides which medications to prescribe, but most often drugs that improve venous outflow, painkillers, pills that lower blood pressure, etc. are prescribed. Such treatment cannot solve the problem itself, i.e. correct changes in the vessel, but it improves the patient’s well-being.
Surgical
The operation is prescribed if the doctor fears that the patient will have an ischemic stroke. The surgeon decides what exactly needs to be done. Sometimes he shortens and straightens the artery, sometimes he performs prosthetics or stenting.
Causes of pathology
Why might a person develop this disease? Non-straightness of the course of the vertebral arteries between the transverse processes and in other areas (there are several sections of the VA: prevertebral, cervical, cervico-occipital, intracranial) appears due to a number of diseases:
- cervical osteochondrosis;
- congenital anomalies;
- injuries in which the cervical spine was damaged;
- hypothermia, which causes muscle spasm, which affects the location of the artery;
- tumor;
- Bekhterev's disease;
- scarring of tissue after surgery.
These are the main reasons, but there may be others.