Symptoms of cavernous angioma
The patient may have no symptoms, although headaches, seizures, or other focal symptoms, such as motor or sensory disturbances, are common. Most often, the occurrence of symptoms is associated with hemorrhages, which can occur both inside the cavernous angioma and in the surrounding brain tissue. Depending on the severity of the hemorrhage, conservative treatment or surgical intervention is used, which will be discussed below.
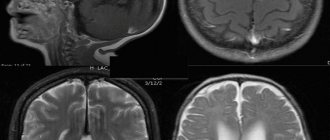
Cavernous angioma of the right frontal lobe. A CT scan without contrast enhancement shows a large heterogeneous mass in the right frontal lobe. The formation is characterized by high X-ray density in its central part and diffusely increased density in the periphery due to the presence of calcifications and small hemorrhages in the formation.
General symptoms of the disease
Newly formed cells exert pressure on neighboring ones.
The initial symptom of the disease is mild headaches and slight dizziness. The characteristic pathology begins to manifest itself as follows:
- Headaches of various types;
- Frequent dizziness accompanied by nausea;
- Epilepsy attacks;
- Paralysis of individual areas;
- Fainting;
- The vestibular apparatus malfunctions;
- Speech disruptions;
- Convulsive twitching;
- Distortion of information reading by taste buds;
- Changes in visual perception;
- Decreased mental activity;
- Noise hallucinations in the head;
- Disease of the venous system.
Vascular malformations of the brain
Types of vascular malformations differ based on their macroscopic and microscopic characteristics. Typically, intracranial vascular malformations are divided into the following 4 groups:
- Capillary malformations (or telangiectasias)
- Cavernous malformations (cavernous angiomas/hemangiomas)
- Venous malformations
- Malformations with arteriovenous shunts
According to the newer classification, 2 more categories have been added: arterial malformations (without the formation of an arteriovenous shunt) and mixed malformations.
Cavernomas can be found in any area of the brain because they can arise anywhere along the vascular bed. Intracranial extracerebral cavernous angiomas sometimes occur, but they are quite rare. Cavernous angiomas are also sometimes found in the spinal cord, most often in association with multiple vascular lesions of the brain.
Forecasts
If the pathology is not detected in a timely manner, it can cause serious complications:
- Rupture of blood vessels and hemorrhage in the brain.
- Disruption of blood flow.
- Acute deficiency of nutrients supplied to the brain.
With venous angioma, doctors give favorable prognoses, but here, too, the success of treatment depends on several factors:
- The patient's age.
- Location and size of the neoplasm.
- Absence or presence of hypertension.
With timely detection of the disease and proper treatment, the victim can hope for a favorable outcome. Postoperative rehabilitation takes several months, after which the person can return to a full life.
The term “benign tumor” does not mean “safe.” Any tumor in the head poses a potential threat to health. Therefore, it is necessary to pay attention to any warning signs of the disorder and monitor your condition. The sooner the operation is performed, the greater the victim’s chances of avoiding serious consequences.
Detection of cavernous angiomas
Despite the fact that cavernous angiomas are visualized using computed tomography (CT), this method is not the method of choice: the fact is that the identified signs in a CT study may correspond not only to cavernous angioma, but also, among other possible options, poorly differentiated tumor.
The sensitivity of magnetic resonance imaging (MRI) is much higher, due to its higher contrast resolution, as well as its greater ability to image flowing blood and its breakdown products. The combination of different MRI pulse sequences has largely solved the problem of misdiagnosis or under-detection of cavernous angiomas, since these lesions have quite specific features on MRI.
Get an MRI of the brain in St. Petersburg
CT and MRI can be used for follow-up of patients with already diagnosed cavernous angiomas, especially in cases where there is a risk of hemorrhage. Although the MR image of cavernous angiomas does not predict the occurrence of bleeding, MRI is the method of choice for long-term follow-up of patients with cavernous angiomas, as well as for the evaluation of family members of the patient who are at risk of having such malformations. In addition, MRI is extremely useful in planning surgical intervention, as it allows you to assess the size of the formation, its boundaries, and thus determine the type of operation and surgical approach.
With classical angiography, most cavernous malformations are not visualized, and even when signs are detected, they are extremely nonspecific. If the lesion develops in combination with other vascular malformations, which occurs in approximately 30% of patients with venous malformations, then its MR characteristics become much more complex and less specific. In such patients, angiography may be useful to further clarify the diagnosis.
What can provoke hemorrhage?
According to neurosurgeons, the risk of hemorrhage in the case of venous angioma is quite low. It is found in 0.22–0.34% of patients. But when analyzing information from pathologists, it turns out that among all vascular causes of death in patients, rupture of brain angiomas accounts for 60%.
Increase the risk of hemorrhage:
- arterial hypertension;
- physical activity (for women – labor);
- sudden bends, jumps;
- turning the head;
- minor head injuries (bruises);
- stressful situations.
Cavernous angioma or tumor?
Brain scanning using CT and MRI in most cases allows one to clearly distinguish a cavernoma from other brain formations, including tumors of varying degrees of malignancy. However, in some cases, differentiation of these formations represents a diagnostic problem, the solution of which requires extensive experience. In this regard, the ability to attract a highly qualified diagnostician is critical. In addition, high-quality interpretation of CT and MRI images provides a solution to other diagnostic problems: exclusion of surrounding cerebral edema, identification of the severity of hemorrhage, description of details affecting the operability of the cavernoma. If you are in doubt about the diagnosis, you should consult a radiologist from a leading center specializing in brain pathology. A second opinion from such a diagnostician can be very valuable in the differential diagnosis of angiomas and other pathological conditions.
Reasons for the appearance of education
The exact causes of cerebral angioma are not yet known, but experts identify the main provoking factors that contribute to its development:
- Pathological course of pregnancy.
- Abnormal development of the internal organs of the fetus.
- Infectious lesions.
- The presence of severe diseases (for example, cirrhosis of the liver).
- Malignant tumors in other organs.
Newborns are more likely to suffer from blood flow disorders due to the fact that their circulatory system is not yet perfect.
Brain angioma is formed when healthy brain vessels divide into small arteries and capillaries, forming one continuous vein. As a result, the abnormally formed vein disrupts blood circulation, taking blood from intact veins and arteries. Thus, brain tissue does not receive enough nutrients, which negatively affects their functioning. 95% of cases of the disease are congenital and only 5% are acquired.
Cavernous angiomas on CT
When using visualization methods, it is useful to separate the cavity into 3 components. These include (1) a peripheral pseudocapsule, consisting of glial tissue impregnated with hemosiderin, (2) an irregularly structured intermediate connective tissue separating the cavities, and (3) a central vascular part, consisting of vascular cavities with slow blood flow.
On CT images without contrast enhancement, a cavernoma appears as a focal formation of an oval or nodular shape, characterized by slightly or moderately increased X-ray density and does not have a volumetric effect on the surrounding parenchyma. Areas of calcification and hemosiderin deposition in the walls of fibrous septa, along with stagnation of blood in the cavities, contribute to increased x-ray density on non-contrast-enhanced images. On CT images, calcifications are detected in approximately 33% of all cavernomas. If the formation is old, then it may contain central non-contrasting areas of reduced density, which corresponds to cysts from resorbed hematomas.
Contrast enhancement can be minimal or maximal, although 70-94% of cavernous malformations are weakly or moderately enhanced after intravenous contrast. In most cases, good contrast is the result of increased blood flow in the vascular component of the mass. The heterogeneous “speckled” enhancement is caused by intravascular fibrous septa, and the low-density rim along the periphery is caused by a pseudocapsule of glial tissue surrounding the formation.
Mass effect is not typical for cavernomas, unless they are associated with recent hemorrhage. On CT images without contrast enhancement, cavernomas may not be detected at all. In hemorrhages and the formation of intracerebral hematoma, cavernomas are visualized as areas of focal signal enhancement in the area adjacent to the hematoma.
Any hemorrhage detected on CT in a relatively young patient should be carefully investigated, and cavernous angioma should always be considered as a possible cause. When evaluating a patient with a seizure disorder, cavernous angioma should also be considered as a likely etiological factor, especially if the patient is between 20 and 40 years of age.
Cavernous malformations identified by CT may also include other rare vascular malformations (thrombosis of arteriovenous malformation, capillary telangiectasia), glioma (poorly differentiated astrocytoma or oligodendroglioma), and metastatic melanoma.
Prevention
We can only talk about secondary prevention for patients with an already established diagnosis, since primary prevention does not exist. Recommended:
- control blood pressure;
- stop smoking and do not indulge in alcohol;
- women should be careful when choosing contraceptives, oral hormonal drugs contribute to circulatory problems;
- take painkillers and antipyretics only after consulting a doctor; all tablets containing Aspirin increase the risk of hemorrhage;
- avoid severe stress and physical tension;
- organize a good rest.
Cavernous angiomas on MRI
Cavernous angiomas represent about 1% of all intracranial vascular lesions and 15% of cerebrovascular malformations. With the development and introduction of MRI, cavernous angiomas have become the most commonly detected vascular malformations of the brain. In early studies on autopsy material, the frequency of their occurrence was 0.02-0.53%. Using MRI, the incidence of formations similar to cavernous hemangiomas was 0.39-0.9%, and the detection of previously unidentified asymptomatic formations using MRI increased their incidence to 0.45-0.9%.
Get an MRI of the brain in St. Petersburg
On MRI, parenchymal cavernous angiomas are represented by a characteristic “popcorn”-type formation, clearly defined, with a smooth border. The internal part is represented by multiple foci of signal of varying intensity, which correspond to hemorrhages at different stages of resolution.
MRI signs of cavernous angioma. Large cavernous angiomas of the right frontal lobe and left occipital lobe on T1-weighted axial section. These two heterogeneous space-occupying lesions have a central mesh structure with alternating areas of high and low signal intensity, surrounded by a hypointense rim of hemosiderin.
A fresh hematoma containing deoxyhemoglobin is isointense on T1-weighted images and significantly hypointense on T2-weighted images. A subacute hematoma containing extracellular methemoglobin is hyperintense on both T1- and T2-weighted images due to the paramagnetic effect exerted by methemoglobin.
Intermediate fibrous elements are characterized by a weakly hypointense signal on T1- and T2-weighted images, since they contain calcifications and hemosiderin. The heterogeneous interior of the mass is surrounded by a hemosiderin rim, which has low intensity on T1-weighted images. The hypointensity of this rim becomes more pronounced, resembling a halo, on T2-weighted and gradient-echo images due to the higher sensitivity of these sequences to changes in the magnetic field.
Axial gradient-echo MR images provide better visualization of large cavernous angiomas in the right frontal and left occipital lobes. The hemosiderin rim appears as a halo due to the increased magnetic susceptibility of hemosiderin.
Smaller cavernomas appear as low-intensity nodules on T1- and T2-weighted images.
Small lesions are better visualized on gradient echo images due to the increased sensitivity to changes in the magnetic field that is inherent in such pulse sequences. It has also been shown that in sequential gradient echo images, small punctate formations are better visualized with longer echo times; these data suggest that such formations contain paramagnetic substances.
Gradient-echo MR imaging shows multiple bilateral small, punctate and round, low-intensity lesions in the periventricular and subcortical white matter. The largest lesion is visualized in the periventricular white matter of the frontal lobe anterior to the anterior (frontal) horn of the left lateral ventricle near the genu of the corpus callosum. Multiple smaller lesions are visible anterior and posterior to it.
On time-of-flight angiography images, methemoglobin in the center of a cavernous malformation may resemble moving blood. However, on a subsequent phase-contrast MR angiogram obtained with a low blood flow speed setting during encoding (10-20 cm/s), blood flow or pathological vascularization is not visualized, which makes it possible to exclude vascular lesions.
Typically, cavernous angiomas do not have a bulking effect on adjacent tissue or cause edema, and they do not have a feeding artery or draining vein unless they are associated with other similar vascular malformations. Cavernous angiomas are often associated with venous malformations, which are characterized by the presence of a draining vein. In such mixed cases, standard angiography may be useful.
T2-weighted image of a cavernoma of the pons.
Cavernous malformations detected on MRI include other occult vascular malformations (AVM/aneurysm thrombosis, capillary telangiectasia), hemorrhage in a primary or secondary tumor (metastasis of melanoma, choriocarcinoma, thyroid or kidney cancer), amyloid angiopathy, treated or primary infection (toxoplasmosis or cysticercosis), multiple hemorrhages associated with damage to the blood system (disseminated intravascular coagulation, leukemia), as well as the consequences of diffuse axonal damage.
Treatment
There are cases when angioma resolves on its own. But often it is necessary to resort to radical methods of treatment, since other methods are ineffective. For example, medications can help relieve painful symptoms, but they cannot untangle the vascular tangle. For this, patients are prescribed painkillers, antihypertensives, and sedatives.
The operation is not performed when diagnosing a small tumor that does not threaten human life, as well as for people with venous angioma, which is characterized by a low risk of choroid plexus rupture.
If the tumor is large and rapidly growing, the following is carried out:
- Traditional way. Removal using a method in which the choroid plexuses are excised.
- Radiosurgical method. Removal of the tumor by blocking the vessels that formed the tangle. In this case, blood will not enter their cavity.
- Sclerotherapy . This method involves blocking the vessels using special catheters through which sclerosing drugs are administered.
- Angioplasty . Allows you to restore the vascular lumen by reconstructing veins and arteries. To restore cerebral circulation and expand the lumen, special metal meshes and balloons are implanted into the affected arteries.
- Liquid embolization . Involves the introduction of a substance into the problem vessels, disconnecting them from the general blood flow. Over time, the damaged vessel is replaced by connective tissue.
- Embolization . This method of treatment allows you to clog and “disconnect” blood vessels from the general circulation by introducing a special spiral.
The choice of one or another method of operation depends on the clinical manifestations, location, size of the tumor, age, and general condition of the patient. Modern specialists try to use minimally invasive treatment methods, as they minimally injure surrounding healthy tissue and significantly reduce the rehabilitation period. Radiosurgical methods using a Gamma Knife or Cyber Knife destroy pathology by exposing it to radio wave beams of radiation.