Adrenergic blockers (adrenolytics) are medications that block adrenergic receptors of various types in organs and tissues, preventing the implementation of the effects of natural biologically active substances - the mediator norepinephrine and the adrenal hormone adrenaline.
Norepinephrine is a transmitter of impulses in the peripheral nervous system, regulating the functioning of many internal organs and systems (in particular, the heart, blood vessels, bronchi, uterus, pancreas, urinary system, etc.). Adrenaline is similar in structure and function to norepinephrine and is a hormone of the inner (brain) layer of the adrenal cortex.
Norepinephrine and adrenaline realize their effects through interaction with special structural components of cells - receptors, namely adrenergic receptors. Depending on their location and functions, adrenergic receptors are classified into alpha (α)- and beta (β)-adrenergic receptors.
α-Adrenergic receptors are located mainly in blood vessels, the iris of the eye, and the urinary tract. The effects of α-adrenergic receptor stimulation include constriction of blood vessels (and consequently increased blood pressure), pupil dilation, and urinary retention.
β-Adrenergic receptors are localized primarily in the heart (β1-adrenergic receptors), as well as in the bronchi and uterus (β2-adrenergic receptors). When they are stimulated, an increase in the strength and frequency of heart contractions, dilation of the bronchi and relaxation of the uterus are observed.
There is a separate class of drugs that can stimulate adrenergic receptors (adrenergic agonists, adrenergic stimulants), and a group of drugs that can block adrenergic receptors (adrenergic blockers, adrenergic steroids).
Depending on the degree of selectivity, adrenergic blockers are divided into α-adrenergic blockers, β-adrenergic blockers, as well as α- and β-adrenergic blockers. Let us consider in detail drugs that block α-adrenergic receptors.
Indications for use
α-blocker drugs are used for chronic persistent increases in blood pressure - hypertension (essential arterial hypertension).
Also, α-blockers are indicated for the diagnosis and preoperative treatment of a tumor of the adrenal medulla that produces adrenaline - pheochromocytoma.
α-blockers are also used for peripheral vascular spasms (Raynaud's disease and syndrome).
In addition, selective α1-blockers (tamsulosin, alfuzosin, doxazosin) are used in the treatment of benign prostatic hyperplasia - prostate adenoma.
Nicergoline is used for cerebral circulation disorders due to narrowing of cerebral vessels by atherosclerotic plaques, thrombus, as well as for spasms of cerebral vessels - transient ischemic attacks.
Dihydroergotamine is used in the complex treatment of migraine attacks.
Alpha-blockers in the treatment of cognitive and vascular disorders of the brain
M.F. Ivanova, S.K. Yevtushenko, Donetsk National Medical University. M. Gorky, Institute of Emergency and Reconstructive Surgery named after. VC. Gusak Academy of Medical Sciences of Ukraine, Donetsk
Cerebrovascular pathology occupies one of the leading places in the structure of morbidity and mortality of the population of developed countries. The prevalence of strokes and transient ischemic attacks, according to various sources, ranges from 500 to 800 per 100 thousand population, and this figure has a clear upward trend in recent years [1, 2, 5]. In Ukraine, about 110-125 thousand strokes are registered annually, while mortality rates from this pathology are 2.5 times higher than similar indicators in Western countries [2]. Chronic cerebrovascular insufficiency, leading to the development of cognitive impairment, is of significant importance, especially in old age. In turn, vascular and cognitive impairments significantly affect work ability and social adaptation.
Due to the wide range of pharmacological effects on the central and peripheral nervous system, drugs belonging to the group of alpha-blockers are used to treat vascular and cognitive disorders of the brain.
Let us recall that in adrenergic synapses the transmission of excitation is carried out through the mediator norepinephrine. Within peripheral innervation, norepinephrine takes part in the transmission of impulses from adrenergic (sympathetic) nerves to effector cells.
In response to nerve impulses, norepinephrine is released into the synaptic cleft and its subsequent interaction with adrenergic receptors of the postsynaptic membrane. Adrenergic receptors are located in the central nervous system and on the membranes of effector cells innervated by postganglionic sympathetic nerves [3].
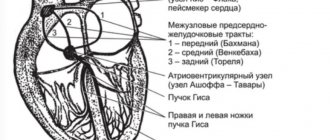
The adrenergic receptors existing in the body have unequal sensitivity to chemical compounds. The formation of a drug-receptor complex with some substances causes an increase (excitation), while with others it causes a decrease (inhibition) in the activity of the innervated tissue or organ. To explain these differences in the reactions of different tissues, in 1948 Ahlquist proposed the theory of the existence of two types of receptors: alpha and beta. Typically, stimulation of alpha receptors causes excitation effects, and stimulation of beta receptors is accompanied by inhibitory effects. Although in general alpha receptors are excitatory receptors, and beta receptors are inhibitory receptors, there are certain exceptions to this rule. Thus, in the heart, in the myocardium, the predominant beta-adrenergic receptors are stimulating. Excitation of beta receptors of the heart increases the speed and strength of myocardial contractions, accompanied by an increase in automaticity and conductivity in the AV node. In the gastrointestinal tract, both alpha and beta receptors are inhibitory. Their stimulation causes relaxation of the smooth muscles of the intestines.
Drugs that have the ability to shield (close) postsynaptic alpha-adrenergic receptors from contact with a mediator (norepinephrine) or adrenergic agonists circulating in the blood (endogenous adrenaline, drugs) are divided into selective alpha-1-adrenergic blockers (alfuzosin, prazosin, doxazosin, tamsulosin, terazosin, etc.) and non-selective, blocking both alpha-1 and alpha-2 adrenergic receptors (phentolamine, trodiphene, ergot alkaloids and their derivatives, nicergoline, proroxane, butyroxane, etc.). Drugs of this group prevent the passage of vasoconstrictor impulses through adrenergic synapses and thereby cause dilation of arterioles and precapillaries [1, 3].
The alpha-adrenergic blocking agent nicergoline is a synthetic derivative of ergot alkaloids (ergot (lat. Claviceps) is a genus of microscopic fungi of the ergot family (Clavicipitaceae) from the order of marsupials (Hypocreales), parasitizing on some cereals, including rye and wheat) with an attached bromine-substituted nicotinic acid residue (nicotinic acid, or niacin, vitamin PP, vitamin B3 - a water-soluble vitamin involved in many oxidative reactions of living cells). It has a vasodilating effect (including in relation to cerebral arteries). Improves microcirculation. The contained nicotinic acid residue has a direct myotropic antispasmodic effect on the muscular lining of resistive vessels, increases their permeability to glucose (neutralizing the opposite effect of the ergoline ring), which is most clearly manifested in the vessels of the brain and extremities. Increases cerebral, pulmonary and renal blood flow. Reduces the tone of central vessels, increases arterial blood flow, increases the delivery of oxygen and glucose. Improves blood supply to the extremities, especially in cases of peripheral circulation disorders caused by functional arteriopathy. In therapeutic doses it does not affect blood pressure; in patients with arterial hypertension it can cause a gradual moderate decrease in blood pressure.
Nicergoline is registered in more than 50 countries and has been used for more than 30 years in the treatment of cognitive, affective, and behavioral disorders in older people [11]. During the period of use of the drug, the rationality of its use has increased. Initially, nicergoline was considered as a vasoactive substance and was prescribed mainly for cerebrovascular disorders. Further studies showed that the pharmacological profile of nicergoline was more complex, and the drug began to be used in various forms of dementia, including Alzheimer's disease [8, 11].
Important in the action of nicergoline are its studied neurotransmitter effects. Nicergoline affects cholinergic processes in the brain. The weakening of cholinergic neuromediation is currently considered as a leading link in the development of age-related impairments of memory, cognitive functions, and in the pathogenesis of various neurodegenerative diseases of the brain [1, 9].
Nicergoline increases the synthesis of acetylcholine by activating choline acetyltransferase, increases the release of acetylcholine from presynaptic terminals, reduces the breakdown of acetylcholine by inhibiting acetylcholinesterase, normalizes the content of postsynaptic M-cholinergic receptors in various parts of the central nervous system, stimulates receptor-effector reactions by activating the phosphoinositide cascade [1, 10].
Nicergoline has a direct protective effect on the formation of beta-amyloid, the main histological substrate of Alzheimer's disease, by activating the translocation of the protein kinase C enzyme [6, 11].
Nicergoline also has a variety of neuroprotective properties: stimulates the reuptake of glutamate and prevents the development of glutamate-mediated neurotoxic effects during hypoxia, has an anti-apoptotic effect, exhibits antioxidant effects, stimulates the formation of nerve growth factor (neurotrophic effect), which promotes the preservation of cholinergic neurons, regulates calcium metabolism in nervous tissue [1, 11]. Another component of the nootropic and vasotropic action of nicergoline is the stimulation of brain-specific nitric oxide synthase [1]. According to modern concepts, nitric oxide not only has vasoregulatory properties in relation to cerebral vessels, but is also involved in the processes of learning and memory [11]. The drug has an antiplatelet effect, inhibiting the aggregation of platelets and red blood cells and thus preventing the development of a thrombotic reaction.
Thus, the pharmacological spectrum of action of nicergoline is characterized by the following effects:
- nootropic;
- vasotropic;
- neurotransmitter;
- neuroprotective;
- metabolic;
- antiplatelet [4].
The unique effects of nicergoline are the foundation of its clinical use, which has expanded significantly in recent years.
The pharmacodynamic properties of nicergoline are based on its ability to influence cellular metabolism - increase the utilization of glucose and oxygen, increase the content of ATP, proteins and the synthesis of nucleic acids. The drug improves cerebral circulation, protects the brain from damage under conditions of hypoxia and ischemia. It has a positive effect on neural transmission, increasing the intensity of dopamine and norepinephrine metabolism, and increases the level of cAMP [6].
Digital analysis of EEG data indicates a positive effect of nicergoline on the bioelectrical activity of the brain and its adaptive capabilities. Nicergoline has a positive effect on cognitive function, improves memory, psychomotor activity, prevents affective disorders and somatic dysfunctions (fatigue, anorexia, dizziness).
At a daily dose of 30-60 mg, nicergoline improves the clinical condition of dementia syndrome over a 3-6 month observation period. The therapeutic effect increases gradually and becomes clinically significant after approximately 3 months. treatment. In patients with a positive response to treatment with nicergoline, improvement in dementia syndrome becomes pronounced by the 6th month. treatment [7].
Nicergoline is quickly and almost completely absorbed from the digestive tract. Subject to significant first pass effects through the liver. When taken orally at a dose of 70 mcg/kg, the concentration in blood plasma is 100-200 ng/ml. Nicergoline is able to bind to plasma albumin; the degree of binding to it is approximately 4 times lower than the ability of the drug to bind to the glycoprotein. The percentage of binding remains relatively constant at physiological plasma protein concentrations, even when the concentration of nicergoline is elevated (87% at low concentrations of nicergoline and 82% at high concentrations) [6]. Since the concentration of the glycoprotein in the blood plasma of elderly patients under pathological conditions, such as acute inflammatory processes, malignant tumors, or in cases of stress may increase, there is reason to believe that the effective concentration of the active ingredient in these conditions may be reduced. Nicergoline is almost completely metabolized by hydrolysis of the ester linkage and N-demethylation. The active metabolites that are formed are conjugated with glucuronic acid.
About 80% of nicergoline metabolites are excreted by the kidneys, 10% are excreted in feces. The half-life of nicergoline is 2.5 hours, the half-life of the main metabolite 10-methoxy-dihydrolysergol (MDL) is 12-17 hours, and the second metabolite 1-methyl-10-methoxy-dihydrolysergol (1-MMDL) is 2 to 4 hours Indications for the use of nicergoline are: acute and chronic cerebral circulatory failure (including cerebral atherosclerosis, transient cerebrovascular accidents, thrombosis and embolism of cerebral vessels); migraine; Raynaud's syndrome; arterial hypertension (as an adjuvant); used as a supportive agent for elderly people with cerebroorganic psychosyndrome with the following main symptoms: decreased concentration, weakened memory, disorientation, sleep disorders, Alzheimer's disease, Parkinson's disease, vascular and mixed dementia.
In patients with impaired renal function (serum creatinine level above 200 mg/ml), the dose should be reduced. Since the therapeutic effect increases gradually, it is recommended to take the drug for a long time (at least 3 months), but at least every 6 months. the need for further treatment with the drug should be assessed.
Contraindications to the use of Nicerium® are hypersensitivity to nicergoline, ergot alkaloids or other components of the drug; previous myocardial infarction; bleeding; risk of collapse; orthostatic reactions; simultaneous treatment with adrenergic agonists; period of pregnancy and lactation, childhood.
The side effects of nicergoline are very limited, usually mild or moderate and are mainly associated with its adrenergic blocking properties: hypotension, dizziness, feeling of heat and flushing; sleep disturbances and gastrointestinal disorders are possible (can be eliminated by taking the drug with meals). In most cases, the described effects either disappear spontaneously or after reducing the dose of the drug and do not require its discontinuation during the course of treatment.
Since nicergoline inhibits platelet aggregation and reduces blood viscosity, while taking the drug, coagulogram parameters should be monitored more often when used simultaneously with other drugs that affect blood clotting. Nicergoline may enhance the effect of antihypertensive drugs.
Nicergoline is the active ingredient of the drug Nicerium® manufactured by Salutas Pharma GmbH, a company of Hexal AG; Rotterdorf Pharma GmbH for Hexal AG, Germany. To date, two types of tablet forms of the drug are registered in Ukraine: sugar-coated tablets, 5 mg each, 50 tablets per package. (registration certificate No. UA/0477/02/01 from 07/20/2006 to 07/20/2011), sugar-coated tablets, 10 mg each, 50 tablets per pack. (registration certificate No. UA/0477/02/02 from 07/20/2006 to 07/20/2011), and Nicerium® 30 Uno capsules 30 mg, 30 capsules in a package (registration certificate No. UA/0477/01/01 from 01/19/2004 until January 19, 2009). When taken orally, tablets and capsules should be swallowed whole with sufficient liquid (for example, water) before meals. The usual daily dose is 20-30 mg of nicergoline, the drug can be taken once or divided into several daily doses. If the desired therapeutic effect is not achieved with this dose, the daily dose can be increased to 60 mg of nicergoline. After a noticeable improvement in the patient's condition, the dose of the drug may be reduced.
In conclusion, it should be noted that today the issue of effective treatment of vascular and cognitive disorders of the brain remains relevant. In this regard, thanks to a wide range of pharmacological effects, the alpha-adrenergic blocking agent nicergoline allows optimizing the strategy and tactics of treating patients with this pathology.
Literature 1. Burchinsky S.G. Vasotropic pharmacotherapy: new aspects // Journal. pract. doctor - 2001. - No. 6. - P. 57-60. 2. Vinichuk S.M. Brain stroke. - K., 1998. - 52 p. 3. Elagin R.I. Adrenergic drugs. Alpha adrenergic blockers // Consilium Provisorum. - 2003. - No. 7. - P. 39-43. 4. Ishchenko M.M., Shkrobot S.I. The effect of nicergoline on systemic and cerebral hemodynamics in patients with dyscirculatory encephalopathy and atherosclerotic lesions of large cerebral vessels // Likarska pravo. - 1992. - No. 10. - P. 100-102. 5. Kistler J.F., Ropper A.-H., Martin J.B. Vascular diseases of the brain // Internal diseases. Book 10. - M.: Medicine, 1997. - P. 44-106. 6. Bellotti V., Januzzo MG, Moro E. et al. Plasma pharmacokinetics of nicergoline metabolites in healthy volunteers // Eur. J. Clin. Pharmacol. - 1989. - Vol. 36 (Suppl.). - R. 150. 7. Bes A., Orgogozo JM, Poncet M. et al. A 24-month, double-blind, placebo-controlled pilot study of the efficacy and safety of nicergoline 60 mg per day in eldery hypertensive patients with leucoaraiosis // Eur. J. Neurol. - 1999. - Vol. 6(3). — P. 313-322. 8. Fioravanti M., Flicker L. Efficacy of nicergoline in dementia and other age-associated forms of cognitive impairment (Cochrane Review) // The Cochrane Library, Issue 2. - Oxford: Update Software, 2002. 9. Hock C. Biochemistry aspects of dementia // Dialogues Clin. Neurosci. - 2003. - Vol. 5. - P. 27-34. 10. Ogawa N., Asanuma M., Hirata H. et al. Cholinergic deficits in aged rat brain are corrected with nicergoline // Arch. Gerontol. Geriatr. - 1993. - Vol. 16. - P. 103-110. 11. Winblad B., Carfagna N., Bonura L. et al. Nicergoline in dementia. A review of its pharmacological properties and therapeutic potential // CNS Drugs. - 2000. - Vol. 14. - P. 267-287.
pharmachologic effect
α-Adrenergic blockers block α-adrenergic receptors in blood vessels, which leads to their dilation and, as a result, a decrease in blood pressure, as well as normalization of peripheral circulation; in addition, by blocking α-adrenergic receptors in the urinary tract, α-blockers facilitate urination in patients with benign prostatic hyperplasia.
Nicergoline dilates blood vessels in the brain, improves cerebral blood flow, increasing blood flow to ischemic (suffering from a lack of oxygen) areas of the brain.
Dihydroergotamine tones the blood vessels of the brain, eliminates acute migraine attacks.
Basic rules for using alpha blockers
You can take the medicine only as prescribed by your doctor. The specialist prescribes the drug based on the cause of the pathology and the general condition of the patient’s body.
Rules for using alpha blockers:
- During treatment you need to avoid spicy, fatty, fried and smoked foods;
- take tablets during or immediately after meals;
- Monitor daily changes in blood pressure and heart rate per minute. This is necessary to assess the effect of therapy on the condition.
When visiting the dentist or before planning surgery, you should tell your doctor about alpha-blocker treatment and the type of medication you are taking.
Basics of treatment with α-blockers
α-Adrenergic blockers are classified as prescription drugs - drugs are dispensed from pharmacies only with a doctor's prescription. Treatment with α-blockers is also carried out under the supervision of a physician.
α-blocker drugs (with the exception of nicergoline, tamsulosin and alfuzosin) significantly dilate blood vessels and lower blood pressure, which can lead to the development of orthostatic hypotension - a sharp drop in pressure, dizziness and loss of consciousness when changing body position (for example, when getting out of bed or standing up). from a sitting position). This effect is especially pronounced when taking the drug for the first time. To avoid the development of orthostatic hypotension after taking α-blockers, you should lie down for 20-30 minutes without getting up suddenly.
Types of drugs
Below is a table of alpha blockers to help you better find the information you need. The table contains lists of drugs, the name of the active substance and commercial names of drugs based on the active component.
Alpha blocker medications
| Group | Active substance | Commercial names of products |
| Alpha-1-blocker drugs | Alfuzosin |
|
| Doxazosin |
| |
| Prazosin |
| |
| Silodosin |
| |
| Terazosin |
| |
| Urapidil |
| |
| Alpha-2 blockers | Yohimbine |
|
| Alpha-1,2-blockers | Dihydroergotoxin |
|
| Proroksan |
| |
| Phentolamine |
|
The dose and duration of drug use are determined by the severity of the disease, the patient’s age and the presence or absence of chronic pathologies.
Classification of funds
To combat the main symptoms of hypertension, it is necessary to block certain classes of nerve endings:
- alpha-1 receptors of vascular smooth muscle fibers;
- alpha-2 receptors of the vasomotor center and the nerve cell conducting the impulse.
To treat arterial hypertension, inhibition of adrenolytic drugs on the corresponding receptors is used. In this case, a significant decrease in norepinephrine occurs, and this normalizes blood pressure. There are 2 broad groups of drugs based on the type of effect on receptors:
- Adrenolytics of selective action. They selectively block only alpha-1 receptors.
- Non-selective adrenolytics. Prevents dilation of blood vessels and receptors of the motor center.
Non-selective blockers are not intended for long-term use. For the treatment of hypertension, alpha blockers of this group are used only to relieve attacks.
Possible side effects
Alpha blockers are effective medications for the treatment of hypertension. In some cases, taking them can cause side effects:
- malaise, darkening of the eyes, heaviness in the head, lightheadedness;
- nausea reflex;
- nervousness, irritability;
- decreased sex drive;
- sleep disorders;
- discomfort in the abdominal area;
- increased sweating;
- tremor;
- sudden development of circulatory failure;
- malfunction of the digestive system;
- pathological increase in the lumen of blood vessels, which can cause fluid stagnation, migraine, and increased heart rate.
When starting to take alpha blockers for hypertension, there is a high risk of side effects.
Drugs containing the active ingredients prazosin and terazosin have a diuretic effect and also reduce the amount of iron-containing protein in the blood.
Important! A pronounced effect of taking alpha blockers for hypertension is observed upon first use. After a long period of use, the effectiveness of the drug decreases markedly.
How does prostate hyperplasia manifest?
prostate hyperplasia
Not all patients immediately experience lower urinary tract symptoms. Typically, urinary incontinence occurs gradually as the urethra narrows and lengthens under pressure from the prostate gland, preventing the normal flow of urine from the bladder.
Men notice the following signs of deteriorating health:
- the outflow of urine weakens;
- it becomes more difficult to start urinating;
- I have to get up several times at night to urinate.
These men may have recurrent urinary tract infections and develop kidney failure.
Sometimes patients do not pay attention to altered urination, and after a cold or drinking alcohol they end up in a medical facility due to acute urinary retention. Simultaneously with stopping urination, severe pain occurs in the lower abdomen. Relief for the patient comes only from emptying the bladder using a catheter.
Treatment of patients with hyperplasia depends on subjective symptoms, such as irritation and obstruction, and objective symptoms, such as intravesical obstruction detected by urodynamic examination.
Symptoms of irritation include residual urine after urination, forced urination, and dysuria. Delayed onset of urination, decreased urination, and loss of fluid after urination are symptoms of obstruction.
Several groups of drugs are used to treat pathology:
- α1 blockers are non-selective, such as doxazosin, and uroselective, such as tamsulosin.
- α-reductase inhibitors (finasteride and dutasteride);
- plant extracts, for example, pumpkin seed extracts, nettle root extracts.
α1 blockers are the predominant group of drugs for the treatment of lower urinary tract symptoms in many countries. For example, in the US, more than 90% of medications prescribed to treat hyperplasia symptoms consist of α1 blockers
Beta blockers: list of drugs
Drugs belonging to the group of beta blockers differ in their selectivity, ability to cross the BBB and duration of action. For example, long-acting drugs that can be taken once a day to achieve the expected effect are:
- betaxolol;
- bisoprolol;
- nebivolol
The following beta blockers are called cardioselective:
- propranolol;
- carvedilol;
- pindolol.
In this case, drugs with relative cardioselectivity include:
- atenolol;
- betaxolol;
- bisoprolol;
- metoprolol;
- nebivolol
Two of them are long-acting medications. Atenolol does not penetrate the blood-brain barrier well.
Types of beta blockers
All drugs from the group of beta blockers can be divided into two types:
- selective;
- non-selective.
Selectivity is determined by the effect on two types of beta-adrenergic receptors. Beta1-adrenergic receptors are located in the heart, and beta2-adrenergic receptors are located mainly in the peripheral vessels and bronchi. The selectivity of a drug indicates the percentage of its effect on the first or second type of receptors. Non-selective, respectively, affect all adrenergic receptors, without seeing the difference between them
In addition, beta blockers are divided into groups based on their ability to dissolve in water or fat. This is indicated by two indicators: hydrophilicity and lipophilicity. Water-soluble drugs have low permeability through the blood-brain barrier, due to which they almost do not cause sleep disturbances or cause nightmares. But such drugs require monitoring the condition of the kidneys, because when the function of the filtering organ decreases, the substance can accumulate. For kidney disease, the dose of beta blockers may need to be adjusted downwards.