- Types of dysplasia
- Degrees of dysplasia
- Diagnosis of the disease
- Treatment of dysplasia
- Recovery period
Dysplasia is a violation of the structure of body tissues, with a simplification of their structure, deformation of cells and their components. Congenital dysplasias caused by genetic causes, as a rule, have diverse manifestations, often multiple and in different systems.
Dysplasia of the mucous membranes has a local connection to a specific organ, such as the stomach, intestines, cervix. Unlike all other dysplasias, this type of pathology is not inherited and is not associated with a global genetic failure, but is caused by the vital activity of pathological microflora.
Introduction
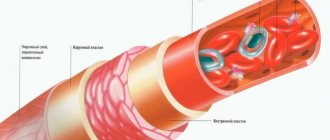
Venous dysplasia is a malformation of veins, which is based on a violation of the formation of the vascular wall during the differentiation of peripheral vessels [1].
In 18.2% of cases, angiodysplasia develops on the head and neck [2]. This localization changes the patient’s appearance and often leads to disturbances in physiological functions (chewing, swallowing and speech) and the psycho-emotional sphere [3].
In recent years, the surgical method [4] and scleroobliteration with 70% and 96% ethyl alcohol solution have become the most widespread in the treatment of angiodysplasia [3, 5, 6]. When the lesion is localized in the soft tissues of the head and neck, sclerotherapy with alcohol is performed in the operating room under intubation anesthesia, followed by transfer of the patient to the intensive care unit for prolonged artificial ventilation. Such management tactics are due to the fact that when sclerosing with alcohols, real dosing of necrosis is impossible both in depth and area. In case of insufficient isolation of the source of exposure, the alcohol solution may enter the vascular bed or burn the skin or mucous membrane located next to the tumor [2, 7].
The possibility of developing such serious complications during sclerotherapy with alcohol has led to the introduction of new drugs into the practice of sclerotherapy [8, 9, 10]. As a rule, for lesions of medium or small volume, residual cavities after surgery, polidocanol or sodium tetradecyl sulfate is used. Preference in the choice of these drugs is determined by greater safety, manifested in a significantly smaller number of skin necrosis and damage to nearby nerve structures. They are used in the compression scleroobliteration mode using microfoam.
The development and introduction into clinical practice of the endovasal laser obliteration technique made it possible to use this technique both for the elimination of dysplastic veins (a variant of endovasal exposure) and in the variant of puncture intervention for venous-cavernous angiomatosis.
Recently, to increase the effectiveness of treatment, attempts have been made to combine several methods [2]. The following clinical observation helped us verify the correctness of this approach.
Diagnosis of the disease
Mucosal dysplasia does not hurt, does not interfere with life - it has no symptoms.
The simplest way to detect pathology of the cervical mucosa was invented by Papanicolaou in the 1940s and consisted of taking scrapings of surface cells . Today, modified instruments are used to collect more material. Examination of cells under a microscope - cytology allows us to determine the next diagnostic stage - colposcopy.
Extended colposcopy - examination of tissues under high magnification from five to 30 times, with additional enhancement of the “picture” with special solutions, which helps in choosing the optimal place for taking a piece of tissue - a biopsy of the area of dysplasia. Pieces of mucous membrane measuring at least 3 millimeters are sent for microscopy - histology. A biopsy is excluded in case of inflammation and infections, but only temporarily.
Further, with morphological confirmation of dysplasia the mucous membrane of the cervical canal is scraped to identify its changes; in a woman, dysplasia can be localized in the glandular crypts - the pits of the mucosa and the epithelial transition zone can move higher. Curettage visualizes the pathological substrate hidden from the eye.
Clinical case
The clinical case is demonstrated with the informed consent of the patient and written consent is submitted to the editor.
The patient, born in 1987, applied to the vascular surgery department of the Road Clinical Hospital, St. Petersburg, on May 17, 2010, with complaints of the presence of two formations on the right half of the face, deforming its shape.
Suffering from birth, notes slow growth of formations over the last 4 years (Fig. 1).
Rice. 1. Photo of the patient before treatment
One of the medical institutions in St. Petersburg performed a CT scan of the head, the results of which confirmed the presence of an area of angiomatosis in the area of the zygomatic arch and a solid hypervascular structure in the projection of the fat pad of the right cheek.
Medical care was refused with the recommendation of dynamic medical observation. Two years later, due to the further growth of the formations, the patient turned to the Department of Maxillofacial Surgery of the North-Western State University named after I.I. Mechnikov, St. Petersburg. Considering the progressive growth of education and a significant deterioration in the patient’s quality of life, an inpatient examination with staged surgical treatment was recommended at the angiosurgery department of the Road Clinical Hospital.
Upon admission, the condition was satisfactory. A comprehensive examination did not reveal any abnormalities in the internal organs and systems.
Local status. In the projection of the right zygomatic arch in the thickness of the subcutaneous tissue there is a formation of 4x4 cm, round in shape, soft-elastic consistency, with smooth contours, painless, the skin above it is of normal structure and color; in the depths of the subcutaneous tissue of the right cheek there is a similar formation of 5x5 cm, the skin of the cheek is of normal structure and color.
Ultrasound examination (Logiq Book XP device, color Doppler mapping mode, sensor with an operating frequency of 6.8 MHz) of the tissues of the zygomatic arch revealed areas of angiomatosis with different-sized vascular cavities with low- and medium-speed blood flow in the latter (Fig. 2).
Rice. 2. Ultrasound scan of angiomatous tissues
According to the results of a puncture biopsy of the cheek lesion, no evidence for the presence of a malignant process was revealed.
In June 2010, the following were performed: 1 session of foam-form sclerotherapy with 2% and 1 session with a 3% fiber-vein solution at an interval of 10 days. Both sessions without any clinical effect. From July 2010 to September 2010, four sessions of puncture endovasal laser coagulation (EVLC) of angiomatosis of the zygomatic region and two sessions of EVLC of hypervascular tissue of the cheek on the right were performed with a time interval of 10-14 days. In September 2010, laser ablation of a vascular neoplasm in the zygomatic region was supplemented with two procedures of foam-form sclerotherapy with a 3% fibrovein solution. All procedures with good immediate clinical and ultrasound effect (Fig. 3).
Rice. 3. Photograph of the patient after sclerotherapy and EVLT of angiomatous tissues
This formation significantly decreased in size; according to duplex angioscanning, blood flow in it was not recorded.
However, in the area of Bichat bodies, the formation retained its volume. In order to correct the shape of the face with radical removal of the solid structure of the cheek, together with plastic surgeons of the Department of Maxillofacial Surgery of the North-Western State University named after I.I. Mechnikov, a decision was made to perform an open combined intervention.
On 03/09/11, in the department of angiosurgery of the Road Clinical Hospital, an operation was performed: unilateral face-lifting with SMAS plication of the middle and lower zone of the face; removal of the cheek fat pad; EVLT of the residual area of hypervascular tissue (Fig. 4).
Rice. 4. Stages of the operation. Arrows indicate areas of hypervascular tissue
The main areas of hypervascularization, sclerosed and coagulated with a laser in the first stages, significantly simplified the intervention technique and made it possible to perform it almost bloodlessly.
The postoperative period was uneventful. The patient was discharged on March 23, 2011 with a good clinical result and cosmetic effect (Fig. 5).
Rice. 5. Photo of the patient after surgery
Histological conclusion: in the first tissue fragment there are fragments of fatty tissue with inclusions of fibrous and bone tissue. In the second tissue fragment there are many dilated capillaries and vascular cavities of various shapes and sizes. The walls of the cavities are lined with endothelium and separated by connective tissue septa.
Using this clinical observation as an example, we wanted to show the capabilities and effectiveness of various methods of vascular obliteration - laser, chemical and surgical - in the staged treatment of angiodysplasia. The presence in the surgeon’s arsenal of several complementary treatment methods allows one to achieve sufficient radicalism and a good cosmetic effect.
Surgery
At the Northern Clinic, surgical treatment of vascular formations is carried out. Some of them are amenable to drug therapy (capillary, mixed, combined hemangiomas), some of them can be eliminated with a laser (capillary hemangiomas), and a number of vascular formations (cavernous hemangiomas, lymphangioma, vascular malformations) can only be removed surgically.
Without a queue for compulsory medical insurance for residents of Russian regions
More details
Literature
- Mulliken JB Hemangioma sandvascular malformations in infants and children: A classification based on endothelial characteristics / JB Mulliken, J. Glowacki // Plast Reconst Surg. – 1982 Mar. – Vol. 69, N 3. – P. 412–420.
- Venous malformations (angiodysplasia) - the possibilities of modern methods of diagnosis and treatment / V. N. Dan [et al.] // Phlebology. – 2010. – T. 4, No. 2. – P. 42–48.
- Ethanol Sclerotherapy for the Management of Craniofacial Venous Malformations: the Interim Results / Ho Lee // Korean J Radiol. – 2009 May-Jun. – Vol. 10, N 3. – P. 269–76.
- Venous malformations of skeletal muscle / KD Hein // Plast Reconstr Surg. – 2002 Dec. – Vol. 110, N 7. – P. 1625–35.
- Ethanol sclerotherapy of venous malformations: evaluation of systemic ethanol contamination / FD Hammer // J Vase Interv Radiol. – 2001 May. – Vol. 12, N 5. – P. 595–600.
- Advanced management of venous malformation with ethanol sclerotherapy: mid-term results / BB Lee // J Vasc Surg. – 2003 Mar. – Vol. 37, N 3. – P. 533–38.
- Diagnosis and treatment of venous malformations. Consensus Document of the International Union of Phlebology / BB Lee [et al.] // Int Ang. – 2009 Dec. – Vol. 28, N 6. – P. 434–51.
- Sonographically guided percutaneous sclerosis using 1% polidocanol in the treatment of vascular malformations / R. Jain // J Clin Ultrasound. – 2002 Sep. – Vol. 30, N 7. – P. 416–23.
- Treatment of venous malformations with sclerosant in microfoam form / J Cabrera // Arch Dermatol. – 2003 Nov. – Vol. 139, N 11. – P. 1409–16.
- Percutaneous sclerotherapy of peripheral venous malformations in pediatric patients / F. Gulsen // Pediatr Surg Int. – 2011 Dec. – Vol. 27, N 12. – P. 1283–37.
Information about authors
Sonkin I.N., Candidate of Medical Sciences, Head of the Department of Vascular Surgery of the National Healthcare Institution "Road Clinical Hospital" of JSC "Russian Railways", St. Petersburg.
Shaydakov E.V., Doctor of Medical Sciences, Professor, Deputy Director for Scientific and Clinical Work of the Federal State Budgetary Institution "Research Institute of Experimental Medicine" of the North-Western Branch of the Russian Academy of Medical Sciences, St. Petersburg. Mikhailov V.V., Candidate of Medical Sciences, Associate Professor of the Department of Maxillofacial Surgery, North-Western State University named after I.I. Mechnikov. Remizov A.S., Candidate of Medical Sciences, Deputy Chief Physician for Surgery of the National Healthcare Institution "Road Clinical Hospital" of JSC "Russian Railways", St. Petersburg. Krylov D.V., surgeon, department of vascular surgery, National Health Institution "Road Clinical Hospital" of JSC "Russian Railways", St. Petersburg. Chernykh K.P., surgeon, department of vascular surgery, National Health Institution "Road Clinical Hospital" of JSC "Russian Railways", St. Petersburg. The article was received on May 24, 2013.
Causes
The specific causes, mechanism of occurrence and course of the disease have not been fully studied. Most researchers believe that this systemic vascular pathology is a consequence of congenital changes in the structure of elastic tissue. A deficiency of elastic fibers leads to a compensatory increase and proliferation of muscle and fibrous tissue.
Some doctors focus on the specific role of mechanical stress. An example is the development of characteristic degeneration of the renal artery due to tension in the vascular pedicle of the kidney due to its excessive pathological mobility - ptosis. But this conclusion remains quite controversial.