Definition
Vessels of the legs - arteries, arterioles, capillaries, veins and venules that supply blood to the tissues of the lower extremities.
Healthy leg blood vessels are an important component of human health. They supply the legs with blood, oxygen and nutrients, allowing a person to lead a full, active life. When the vessels of the legs are exposed to diseases, without proper and timely treatment this leads to serious consequences. The arteries of the lower extremities are paired. Here are the main ones:
- femoral artery (continuation of the iliac artery)
- popliteal artery (divides into tibial arteries)
- artery of the foot.
The veins of the lower extremities are divided into superficial and deep. The deep veins are paired; they accompany the arteries and participate in the process of blood drainage. Excessively dilated blood vessels in the legs are not only an aesthetic problem, but also a sign of pathological processes in the body.
Anatomy of the veins of the lower extremities
The veins of the lower extremities are divided into superficial and deep.
Superficial veins of the lower limb
The superficial venous system of the lower extremities begins from the venous plexuses of the toes, forming the venous network of the dorsum of the foot and the cutaneous dorsal arch of the foot. From it originate the medial and lateral marginal veins, which pass into the greater and lesser saphenous veins, respectively. The plantar venous network anastomoses with the deep veins of the fingers, metatarsals and the dorsal venous arch of the foot. Also, a large number of anastomoses are located in the area of the medial malleolus.
The great saphenous vein is the longest vein in the body, contains from 5 to 10 pairs of valves, and its normal diameter is 3-5 mm. It originates in front of the medial epicondyle and rises in the subcutaneous tissue behind the medial border of the tibia, bends around the medial femoral condyle behind and passes to the anteromedial surface of the thigh, parallel to the medial border of the sartorius muscle. In the area of the oval window, the great saphenous vein pierces the ethmoidal fascia and flows into the femoral vein. Sometimes the great saphenous vein on the thigh and leg can be represented by two or even three trunks. From 1 to 8 large tributaries flow into the proximal portion of the great saphenous vein, the most constant of which are: the external genital, superficial epigastric, posteromedial, anterolateral veins and the superficial vein surrounding the ilium. Typically, tributaries flow into the main trunk in the area of the fossa ovale or somewhat distally. In addition, muscle veins can flow into the great saphenous vein. The small saphenous vein begins behind the lateral malleolus, then it rises in the subcutaneous tissue, first along the lateral edge of the Achilles tendon, then along the middle of the back surface of the leg. Starting from the middle of the leg, the small saphenous vein is located between the layers of the fascia of the leg (N.I. Pirogov’s canal) accompanied by the medial cutaneous nerve of the calf. That is why varicose veins of the small saphenous vein are much less common than the large saphenous vein. In 25% of cases, the vein in the popliteal fossa pierces the fascia and flows into the popliteal vein. In other cases, the small saphenous vein can rise above the popliteal fossa and flow into the femoral, large saphenous vein, or into the deep vein of the thigh. Therefore, before the operation, the surgeon must know exactly where the small saphenous vein flows into the deep one in order to make a targeted incision directly above the anastomosis. The constant estuarine tributary of the small saphenous vein is the fenopopliteal vein (vein of Giacomini), which flows into the greater saphenous vein. Many cutaneous and saphenous veins flow into the small saphenous vein, most in the lower third of the leg. It is believed that the small saphenous vein drains blood from the lateral and posterior surface of the leg.
Deep veins of the lower limb
The deep veins begin as the plantar digital veins, which become the plantar metatarsal veins, which then drain into the deep plantar arch. From it, blood flows through the lateral and medial plantar veins into the posterior tibial veins. The deep veins of the dorsum of the foot begin with the dorsal metatarsal veins of the foot, which drain into the dorsal venous arch of the foot, from where blood flows into the anterior tibial veins. At the level of the upper third of the leg, the anterior and posterior tibial veins merge to form the popliteal vein, which is located lateral and somewhat posterior to the artery of the same name. In the area of the popliteal fossa, the small saphenous vein and the veins of the knee joint flow into the popliteal vein. Then it rises in the femoral-popliteal canal, now called the femoral vein. The femoral vein is divided into the superficial vein, located distal to the deep vein of the thigh, and the common vein, which is located proximal to it. The deep vein of the thigh usually flows into the femoral vein 6-8 cm below the inguinal fold. As you know, the femoral vein is located medial and posterior to the artery of the same name. Both vessels have a single fascial sheath, while doubling of the trunk of the femoral vein is sometimes observed. In addition, the medial and lateral veins surrounding the femur, as well as muscular branches, flow into the femoral vein. The branches of the femoral vein widely anastomose with each other, with the superficial, pelvic, and obturator veins. Above the inguinal ligament, this vessel receives the epigastric vein, the deep vein surrounding the ilium and passes into the external iliac vein, which merges with the internal iliac vein at the sacroiliac joint. This section of the vein contains valves, in rare cases, folds and even septa, which causes thrombosis to be frequently localized in this area. The external iliac vein does not have many tributaries and collects blood mainly from the lower limb. Numerous parietal and visceral tributaries flow into the internal iliac vein, carrying blood from the pelvic organs and pelvic walls. The paired common iliac vein begins after the confluence of the external and internal iliac veins. The right common iliac vein, somewhat shorter than the left, runs obliquely along the anterior surface of the 5th lumbar vertebra and has no tributaries. The left common iliac vein is slightly longer than the right and often receives the median sacral vein. The ascending lumbar veins flow into both common iliac veins. At the level of the intervertebral disc between the 4th and 5th lumbar vertebrae, the right and left common iliac veins merge to form the inferior vena cava. It is a large vessel without valves, 19-20 cm long and 0.2-0.4 cm in diameter. In the abdominal cavity, the inferior vena cava is located retroperitoneally, to the right of the aorta. The inferior vena cava has parietal and visceral branches, which supply blood from the lower extremities, lower torso, abdominal organs, and pelvis. Perforating (communicating) veins connect the deep veins with the superficial ones. Most of them have valves located suprafascially and thanks to which blood moves from the superficial veins to the deep ones. About 50% of the communicating veins of the foot do not have valves, so blood from the foot can flow from deep veins to superficial ones, and vice versa, depending on the functional load and physiological conditions of outflow. There are direct and indirect perforating veins. Direct ones directly connect the deep and superficial venous networks, indirect ones connect indirectly, that is, they first flow into the muscular vein, which then flows into the deep vein. The vast majority of perforating veins arise from tributaries rather than from the trunk of the great saphenous vein. In 90% of patients, there is incompetence of the perforating veins of the medial surface of the lower third of the leg. On the lower leg, incompetence of the perforating veins of Cockett, which connects the posterior branch of the great saphenous vein (vein of Leonardo) with the deep veins, is most often observed. In the middle and lower thirds of the thigh there are usually 2-4 most permanent perforating veins (Dodd, Gunter), directly connecting the trunk of the great saphenous vein with the femoral vein. With varicose transformation of the small saphenous vein, incompetent communicating veins of the middle, lower third of the leg and in the area of the lateral malleolus are most often observed. In the lateral form of varicose veins, the localization of perforating veins is very diverse.
Vascular diseases of the extremities and their causes
Among diseases of the blood vessels of the legs, atherosclerosis and inflammatory lesions of the arteries are common. Atherosclerotic lesion of the vessels of the lower extremities is a disease that affects older people (over 45 years old), mainly men. With atherosclerosis of the vessels of the extremities, the arteries of the legs narrow, preventing the passage of blood.
Another type of disease that affects the vessels of healthy-looking legs is inflammatory lesions of the arteries. They also cause vasoconstriction, which occurs as a result of the development of the inflammatory process. When inflamed, the walls of the artery thicken evenly along their entire length, complicating the flow of blood. Smoking increases the risk of arterial disease; thromboangiitis obliterans is more often diagnosed in young men who smoke.
Complete blockage or occlusion of the vessels of the legs can occur with any of the listed pathologies. Its sad consequences are gangrene and amputation. To avoid this, consult a doctor promptly when the first characteristic symptoms appear:
- Intermittent claudication;
- Pain in the legs that occurs when walking;
- Feelings of fatigue and weakness in the legs (or one leg);
- Erectile dysfunction in men;
- Cold feet, numbness, tingling sensation.
These and other symptoms of vascular diseases of the lower extremities are a reason to urgently consult a doctor.
How are the legs supplied with blood?
Depending on the structural features and functions performed, all vessels can be divided into arteries, veins and capillaries.
Arteries are hollow tubular formations that carry blood from the heart to peripheral tissues.
Morphologically they consist of three layers:
- external – loose tissue with feeding vessels and nerves;
- medium, made of muscle cells, as well as elastin and collagen fibers;
- internal (intima), which is represented by endothelium, consisting of squamous epithelial cells, and subendothelium (loose connective tissue).
Transport of oxygenated blood
Depending on the structure of the middle layer, medical instructions distinguish three types of arteries.
Table 1: Classification of arterial vessels:
| Name | Description | Vessels in the body |
| Elastic | The middle layer of such vessels is represented mainly by elastic fibers. They are able to withstand large pressure differences. |
|
| Mixed | The number of elastic and muscle fibers in such vessels is approximately the same. |
|
| Muscular | The middle layer is represented mainly by muscle fibers located along the diameter. |
|
Note! Arteries are also represented by arterioles - small vessels that directly continue into the capillary network.
Veins are hollow tubes that carry blood from organs and tissues to the heart.
They are divided into:
- Muscular - have a myocyte layer. Depending on the degree of its development, there are underdeveloped, moderately developed, and highly developed. The latter are located in the legs.
- Non-muscular - consist of endothelium and loose connective tissue. Found in the musculoskeletal system, somatic organs, and brain.
Vein structure
Arterial and venous vessels have a number of significant differences, presented in the table below.
Table 2: Differences in the structure of arteries and veins:
| Sign | Arteries | Vienna |
| Diameter | Less | More |
| Number of elastic vessels | More | Less |
| Walls | Thicker | Thinner |
| Middle layer | Developed | Not developed |
| Outer layer | Weakly expressed | Strongly expressed |
| Valves | None | Made of venous wall and endothelium. Regulate the movement of blood “from bottom to top” |
The photo shows a schematic representation of the arteriovenous network in the human body.
Arteries of the legs
Blood supply to the legs occurs through the femoral artery. A. femoralis continues the iliac a., which in turn extends from the abdominal aorta. The largest arterial vessel of the lower limb lies in the anterior groove of the thigh, then descends into the popliteal fossa.
Blood supply to the thigh
Note! If there is severe blood loss due to a wound in the lower limb, the femoral artery is pressed against the pubic bone at its exit.
Femoral a. gives several branches represented by:
- superficial epigastric, rising to the anterior wall of the abdomen almost to the navel;
- 2-3 external genitalia, supplying the scrotum and penis in men or the vulva in women; give off 3-4 thin branches called inguinal;
- superficial circumflex, directed to the upper anterior surface of the ilium;
- deep femoral - the largest branch, starting 3-4 cm below the inguinal ligament.
With atherosclerosis, blood circulation is often impaired at level a. femoralis
Note! The deep femoral artery is the main vessel providing O2 access to the tissues of the thigh. A. femoralis, after its departure, goes down and supplies blood to the lower leg and foot.
The popliteal artery begins from the adductor canal.
It has several branches:
- the superior lateral and middle medial branches pass under the knee joint;
- lower lateral – directly in the knee joint;
- middle genicular branch;
- posterior branch of the tibial region.
In the area of the lower leg, popliteal a. continues into two large arterial vessels called tibial (posterior, anterior). Distal from them are the arteries that supply the dorsum and plantar surfaces of the foot.
Blood supply to the leg and foot
Veins of the legs
Veins provide blood flow from the periphery to the heart muscle. They are divided into deep and superficial (subcutaneous).
The deep veins, located in the foot and leg, are double and run next to the arteries. Together they form a single trunk of V. poplitea, located slightly posterior to the popliteal fossa.
The outflow of blood from the NK is carried out through numerous veins
How is the examination carried out?
The doctor examines and interviews the patient and prescribes a comprehensive examination. It includes laboratory tests and vascular diagnostics. Various methods, including instrumental ones, help to assess the condition of blood vessels.
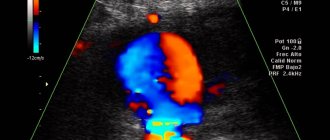
Today, examination of the blood vessels of the legs is carried out using modern equipment. These are angiography, Doppler ultrasound, magnetic resonance angiography and others. Once the diagnosis is made, the patient is prescribed treatment and given recommendations regarding his lifestyle. If the condition is not severe, standard drug treatment and prevention of atherosclerosis are prescribed. If there are vascular diseases of the extremities, the patient is advised to immediately stop smoking, move more, consume less salt and animal fats, and control weight. When the vessels are significantly affected and drug treatment does not bring results, the patient is recommended to undergo surgery. Read more about how obliterating atherosclerosis of the arteries of the lower extremities is treated in the following publication.
Vienna
Human venous system
When considering the arteries, do not forget that the human circulatory system also includes venous vessels, which must be considered together with the arteries to create an overall picture. Arteries and veins have a number of differences, but still their anatomy always requires a combined consideration.
Veins are divided into two types and can be muscular or non-muscular. Venous walls of the muscleless type contain endothelium and loose connective tissue. Such veins are found in bone tissue, internal organs, the brain and the retina.
Venous vessels of the muscular type, depending on the development of the myocyte layer, are divided into three types, and are underdeveloped, moderately developed and highly developed. The latter are located in the lower extremities, providing them with tissue nutrition.
Veins transport blood, which does not contain nutrients and oxygen, but is saturated with carbon dioxide and breakdown substances synthesized as a result of metabolic processes. The blood flow passes through the limbs and organs, moving directly to the heart. Often the blood overcomes the speed and force of gravity several times less than its own. This property is ensured by the hemodynamics of the venous circulation. In arteries this process occurs differently. These differences will be discussed below. The only venous vessels that have different hemodynamics and blood properties are the umbilical and pulmonary.
Peculiarities
Let's look at some of the features of this network:
- Compared to arterial vessels, venous vessels have a larger diameter.
- They have an underdeveloped subendothelial layer and have fewer elastic fibers.
- They have thin walls that fall off easily.
- The middle layer, consisting of smooth muscle elements, is poorly developed.
- The outer layer is quite pronounced.
- They have a valve mechanism created by the venous wall and inner layer. The valve consists of myocyte fibers, and the inner leaflets consist of connective tissue. The outside of the valve is lined with an endothelial layer.
- All venous membranes have vascular vessels.
The balance between venous and arterial blood flow is ensured due to the density of the venous networks, their large number, venous plexuses, and larger sizes compared to arteries.
Differences
How does the vascular network differ from the arterial network - these vessels have not only similarities, but also differences, which will be discussed below.
Structure
Arterial vessels are thicker-walled. They contain a large amount of elastin. They have well-developed smooth muscles, that is, if there is no blood in them, they will not fall off. They ensure rapid delivery of oxygen-enriched blood to all organs and limbs, thanks to the good contractility of their walls. The cells included in the wall layers allow blood to circulate through the arteries without obstruction.
They have an internal corrugated surface. They have this structure due to the fact that the vessels must withstand the pressure generated in them due to powerful blood emissions.
Venous pressure is much lower, so their walls are thinner. If there is no blood in them, then the walls collapse. Their muscle fibers have weak contractile activity. The inside of the veins has a smooth surface. Blood flow through them is much slower.
Their thickest layer is considered to be the outer one, in the arteries - the middle one. Veins do not have elastic membranes; in arteries they are represented by internal and external sections.
Form
The arteries have a regular cylindrical shape and a round cross-section. Venous vessels have flattening and a tortuous shape. This is due to the valve system, thanks to which they can contract and expand.
Quantity
There are approximately 2 times fewer arteries in the body than veins. There are several veins for each middle artery.
Valves
Many veins have a valve system that prevents blood flow from flowing in the opposite direction. The valves are always paired and are located across the entire length of the vessels opposite each other. Some veins do not have them. In arteries, the valve system is present only at the exit from the heart muscle.
Blood
Blood flows in veins many times more than in arteries.
Location
Arteries are located deep in the tissues. They reach the skin only in areas where the pulse can be heard. All people have approximately the same pulse zones.
Direction
Blood flows through arteries faster than through veins due to the pressure of the heart. At first the blood flow is accelerated, and then it decreases.
Venous blood flow is represented by the following factors:
- The force of pressure, which depends on the blood impulses coming from the heart and arteries.
- Suction force of the heart during relaxation between contractile movements.
- Suction venous action during breathing.
- Contractile activity of the upper and lower extremities.
Also, the blood supply is located in the so-called venous depot, represented by the portal vein, the walls of the stomach and intestines, the skin and the spleen. This blood will be pushed out of the depot in case of large blood loss or severe physical exertion.
Color
Since arterial blood contains a large number of oxygen molecules, it has a scarlet color. Venous blood is dark because it contains decay elements and carbon dioxide.
During arterial bleeding, the blood flows like a fountain, and during venous bleeding, it flows in a stream. The first poses a serious danger to human life, especially if the arteries of the lower extremities are damaged. The distinctive features of veins and arteries are:
- Transportation of blood and its composition.
- Different wall thicknesses, valve systems and blood flow strength.
- Number and depth of location.
Veins, unlike arterial vessels, are used by doctors to draw blood and inject drugs directly into the bloodstream to treat various ailments.
Knowing the anatomical features and the arrangement of arteries and veins not only in the lower extremities, but throughout the body, you can not only correctly provide first aid for bleeding, but also understand how blood circulates throughout the body.
When to see a doctor
If you have symptoms of chronic venous insufficiency and you want to determine the exact cause and completely get rid of the discomfort, then sign up for a consultation right now. Employees of the Phlebological Center of the City Clinical Hospital named after V.V. Veresaeva will check the condition of the vascular bed and give individual recommendations based on the treatment experience of the best clinics in the USA and Europe.
Causes of varicose veins
Weak or damaged valves can lead to varicose veins. Arteries carry blood from your heart to your tissues, and veins return blood to your heart. The veins in the legs work against gravity.
The contractions of the muscles in the lower legs act as a pump, and the walls of the elastic vein help blood return to your heart. Tiny valves in your veins open as blood flows toward your heart and then close to stop the blood flowing back. If these valves are weak or damaged, blood can flow backward and pool in the vein, causing the veins to stretch or twist.
Risk factors
These factors increase the risk of developing varicose veins:
- Age . The risk of varicose veins increases with age. Aging causes wear and tear on the vein valves that help regulate blood flow. Ultimately, wear and tear causes blood to flow back into your veins.
- Floor . Women are more likely to develop this disease. Hormonal changes during pregnancy, premenstruation, or menopause may be a factor because female hormones tend to reduce the elasticity of vein walls. Hormonal medications, such as birth control pills, may increase the risk of developing varicose veins.
- Pregnancy . During pregnancy, the volume of blood in your body increases. This change supports fetal growth, but can also lead to the unwanted side effect of dilated veins in the legs. Hormonal changes during pregnancy may also play a role.
- Family illness . If other family members have had varicose veins, you have a better chance.
- Obesity . Excess weight puts extra pressure on your veins.
- Standing or sedentary lifestyle . Your blood doesn't flow as well if you stay in the same position for a long time.
Complications
Complications of varicose veins, although rare, may include:
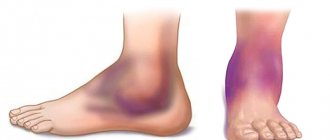
- Ulcer . Peptic ulcers can form on the skin near varicose veins, especially near the ankles. A discolored patch of skin usually appears before an ulcer forms. Call your doctor immediately if you suspect you have an ulcer.
- Blood clot formation . Sometimes the deep veins in the legs become enlarged. In such cases, the affected leg may become painful and swollen. Any persistent leg pain or swelling requires medical attention because it may indicate a blood clot, a condition medically known as thrombophlebitis.
- Bleeding . Sometimes veins very close to the skin can burst. This usually causes only minor bleeding. But any bleeding requires medical attention.