Sclerotherapy (scleroobliteration) of veins is a modern method of treating varicose veins, based on the introduction of special chemicals (sclerosants) into the lumen of the vessel, causing gluing of the walls and subsequent resorption of the vein. The technique is aesthetic, since without incisions or scars it allows you to fight various manifestations of varicose veins.
History of the method of sclerotherapy (scleroobliteration) of veins
The first mentions date back to the period of antiquity. The works of Hippocrates describe a method of obliterating a vein using a metal rod. An artificial inflammation was induced, then the vein was punctured with an oriental plane tree thorn. The first documented experiments on the injection of solutions into a vein were carried out by Christopher Wren (a mathematician and architect from Oxford) in 1656. The pioneer of sclerotherapy in 1682 was D. Zollikofer (Swiss doctor). Using acid, he tried to cause vein thrombosis.
Dr. C. Pravaz – inventor of the syringe
In 1851, C. Pravaz (a French surgeon) invented a syringe and sclerosed arterial aneurysms with its help. The first procedure in a form close to the modern one (iron perchloride was injected) was reported by Debout and Chassaignac in 1853. Due to the large number of complications accompanying sclerotherapy, the method was given a negative assessment at the congress of surgeons held in Lyon in 1893. At the beginning of the 20th century, Jean Sica injected sodium salicylate into veins, and later sodium carbonate and founded the “French” technique of sclerotherapy.
The discovery of detergents in the 1930s (an effect based on damage to proteins in the inner wall of the vein) marked the beginning of a new chapter in the history of sclerotherapy. Tetradecyl sulfate was invented in 1946, and polidocanol in 1950. Their introduction into practice allowed the technique to become widespread. In the mid-1950s, K. Sigg proposed a “bottom-up” technique (Swedish). In 1960, D. Fegan published work based on successful treatment in 13 thousand patients. In it, he formulated the main postulates of modern sclerotherapy.
Syringe system for foam sclerotherapy according to L. Tissari
The foam block technique, proposed by K. Sigg back in 1949, became widespread in 2000 after the introduction of a three-way valve by L. Tessari (production of high-quality fine foam). The widespread introduction of ultrasound diagnostics made it possible to introduce echo-assisted interventions, which made it possible to carry out stem sclerotherapy and scleroobliteration of perforating veins.
Sclerotherapy (scleroobliteration) of veins - what is it
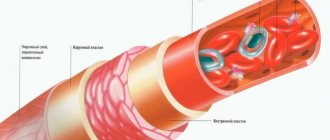
The essence of the technique is the effect of a special chemical substance (sclerosant) on the inner wall of the vein (intima), which ultimately leads to its gluing and complete elimination.
The following requirements apply to sclerosants:
- The effect should only be at a certain concentration, below which the drug has no effect.
- The effect of the drug on the venous wall is only after prolonged contact with it (areas with stagnation of blood, healthy veins are not damaged).
- The drug must be strong enough to sclerosis even large veins, but without damaging the tissue surrounding the vessels.
- Do not cause allergies.
- Do not cause pain when inserted, do not cause pigmentation or scarring of the skin.
- Be highly soluble in saline.
Why do spider veins develop?
There are several theories:
- pathological venous reflux
- micro valve failure
- hormonal influence
- activation of vasoactive mediators under the influence of a variety of conditions, which leads to vascular reorganization
- connective tissue abnormalities.
In general, such a vascular reaction can be caused by a number of diseases and provoking external and internal factors:
- Hormonal changes: pregnancy, taking COCs, corticosteroids.
- Genetic predisposition.
- Violation of the venous system of the lower extremities.
- Symptomatic spider veins in liver cirrhosis, carcinoid, collagenosis, HIV, mastocytosis, cardiovascular disease.
- Congenital diseases and syndromes.
- Physical, mechanical stress: solar, radiation, temperature, injury.
Telangiectasia often develops with age due to the fragility of blood vessels. Their appearance is also influenced by an unhealthy lifestyle.
Types of sclerosants for vein sclerosis
Currently, the following groups of drugs are used in the world for the purpose of sclerosis:
- Detergents, which are fatty (carboxylic) acids and fats. These include: sodium morruate, ethanolamine oleate, tetradecyl sulfate, polidocanol, glycerin.
- Hypertonic and ionic solutions: hypertonic sodium chloride solution (20 and 23.4%); sclerodex – a mixture of 25% dextrose; 10% NaCl with a small amount of 2-phenylethanol; ionized iodine (variglobin).
- Cellular toxins.
The most widely used drugs are the detergent group.
Tetradecyl sulfate (Fibro-vane)
Their action is based on the extraction and denaturation of endothelial membrane proteins of the venous wall. This leads to delayed cell death and obliteration of the vein. The detergent only affects the pathologically altered vein, since the natural blood flow dissolves it to a safe concentration. Thus, only varicose veins with slow blood flow are exposed to chemical effects, healthy ones are not damaged. Unlike other sclerosants, detergents do not cause destruction of blood cells (hemolysis) and intravascular coagulation aggregation (clotting). These qualities determined the leading position of these drugs in sclerotherapy.
Polidocanol (Ethoxysclerol)
In Russia, only drugs from the detergent group are approved for use: polidocanol (ethoxysclerol) and tetradecyl sulfate (fiberwein). Another advantage of these sclerosants is the possibility of using a foam form of the drug.
Types of sclerotherapy (scleroobliteration) of the veins of the lower extremities
- Microsclerotherapy of telangiectasia. The drug is administered in liquid form into vessels with a diameter of up to 1 mm: polidocanol (concentration 0.25-0.75%), tetradecyl sulfate (0.1-0.2%).
- Microsclerotherapy and microfoam (foam-form) sclerotherapy for venulectasias (1-2 mm) and reticular veins (2-4 mm). The foam form of the drug is used: polidocanol (0.5-1%), tetradecyl sulfate (0.25-0.4%).
Foam sclerotherapy Foam-form small veins and spider veins
- Echo-guided sclerotherapy: great and small saphenous veins, tributaries of the great veins, perforating veins. Only the foam form of sclerosant is used in a high concentration of 3% for polidocanol and 1-3% for tetradecyl sulfate.
Foam sclerotherapy (scleroobliteration) of veins under ultrasound guidance
Vein sclerotherapy
Sclerotherapy is a treatment method based on the introduction of drugs into pathologically altered vessels or cavities (for example, cysts), causing their sclerosis (i.e. closing the lumen due to damage by the drug and fusion of the walls).
Currently, the method is mainly used by phlebologists for the treatment of benign neoplasms of the vascular and lymphatic system (hemangiomas, lymphangiomas) and for the treatment of varicose veins and telangiectasia (spider veins) in adults.
In addition, the method is used in proctology for the treatment of chronic hemorrhoids (essentially also a vascular disease), although recently interest in sclerotherapy for the treatment of this disease has decreased significantly due to the emergence of more promising alternative techniques.
Further in the article we will talk only about the use of the method in phlebology; more details about the use of sclerotherapy in proctology can be read in a separate article on our website.
General information about the sclerotherapy method
In our country, three sclerosing drugs are approved for use: thrombovar, fibro-vein, and ethoxysklerol (lately, most experts prefer the last two).
The general principle of the method is quite simple at first glance - using a syringe with a thin needle, without the use of additional diagnostic equipment (what is called “blindly”), a sclerosing drug is injected into the superficial vein, after which in most cases the area of drug administration is compressed with elastic bandages or special compression garments.
But such “simplicity” is applicable only to vessels of very small diameter, the sclerosis of which can be attributed not even to phlebology, but to hardware cosmetology. Until recently, sclerotherapy of larger vessels was accompanied by too high risks of serious complications and was practically not used. Therefore, many experts treated sclerotherapy as a purely symptomatic method, unable to seriously affect the course and prognosis of varicose veins. The situation has changed qualitatively only in the last decade, when, with the development of medical technologies, several modifications of the technique appeared, the classification of which currently looks like this:
microslerotherapy
echosclerotherapy (UNDER THE CONTROL OF AN ULTRASOUND DEVICE)
foam-form therapy (FOAM - FORM)
- Microsclerotherapy is the oldest, classical method of sclerotherapy, which is carried out in the “simple” mode described above. The method is indicated for the removal of very small vascular formations, up to 2 mm in diameter.
- Echosclerotherapy is a variant of sclerotherapy in which the drug is administered under the control of ultrasound duplex scanning of the vessel. Visual control avoids extravascular administration of the drug and significantly reduces the risk of a number of complications, which allows sclerosis of vessels of larger diameter and deeper located ones.
- Foam-form therapy is the latest development in the field of sclerotherapy. Its peculiarity is that sclerosing substances are introduced into the vessel not in liquid form, but in the form of foam. The main drugs for sclerotherapy are detergents (substances with high surface activity), which makes it possible to obtain foam when mixed with air in a ratio of 1:4 or 1:3. The resulting foam allows you to reduce the dose of the sclerosing drug, improve the quality of its effect on the endothelium of the venous wall and increase the time of this effect.
The combination of echosclerotherapy with the introduction of sclerotherapy in the form of foam (foam-form) allows sclerosis of the superficial veins of the lower limb of almost any diameter, not only tributary veins, but also the main vessels - the great and small saphenous veins, even near their confluence with the deep veins, which makes sclerotherapy a significant competitor to surgical methods for treating varicose veins.
Indications for vascular sclerotherapy
The main indications for sclerotherapy are:
- varicose veins of the lower limb
- telangiectasia (spider veins)
- reticular varicose veins
- benign neoplasms of the vascular and lymphatic system (hemangiomas, lymphangiomas)
For telangiectasia (intradermal vascular “stars” with a diameter of up to 0.5 mm) and reticular varicose veins (small, tortuous saphenous veins with a diameter of up to 2 mm) and small vascular neoplasms, microsclerotherapy has proven itself very well. Questions can only be raised by the presence of a competitive technique - laser photocoagulation (in our database of medical services it is described in the section “Medical cosmetology”). There is no single standard for choosing a treatment method in this situation. Cosmetic results are approximately the same, there are no serious complications, and minor temporary cosmetic defects can occur when using both methods (hyperpigmentation, burns, etc.). It is believed that laser photocoagulation is preferable for veins with a diameter of less than 1 mm; if the vessel is larger, the use of sclerotherapy is preferable, although this, of course, is very conditional. By and large, the choice of treatment method in this case is subjective, and mainly depends on the availability of this or that equipment in the clinic where you went, and the preferences and experience of the doctor involved in your treatment. In specialized clinics, a combination of these methods is often used.
If the patient turned to a phlebologist on time (which, unfortunately, does not happen often in our country), in the early stages of varicose veins, then the combination of sclerotherapy in combination with phlebotropic drug therapy and the compression method of treatment is also optimal and can stop the development of the disease for a very long time. long term.
In cases of advanced stages of varicose veins, when more significant medical intervention is required to normalize the venous blood flow of the lower extremities, the situation is not so clear. Currently, quite a lot of methods for treating varicose veins have been developed that claim the honorary title of “the optimal method for treating varicose veins”: echosclerotherapy, phlebectomy (including the so-called miniphlebectomy), endovasal laser coagulation, radiofrequency ablation, transillumination shaver phlebectomy, cryostripping (cryophlebectomy) . The general principles of these interventions are absolutely the same: blocking or crossing the place where the superficial main vein (great saphenous vein) flows into the deep one is performed, removal (stripping) or obliteration of the lumen of the main saphenous vein (along its entire length, or only in the pathologically changed area), removal or obliteration lumen of varicose tributary veins. Data on treatment results given in the medical literature do not differ significantly, therefore modern methods of treating varicose veins “compete” with each other mainly in terms of rehabilitation and hospital stay, the need for anesthesia and cosmetic results. Moreover, taking into account the interest in promoting all the methods of companies producing equipment and drugs for treatment, there are more than enough laudatory articles about each of them, and they need to be treated with caution.
Returning to the topic of this article - what place does sclerotherapy take in the treatment of advanced forms of varicose veins?
Objective contraindications to sclerotherapy, as an independent method of treating varicose veins, are described in the next section of the article. Otherwise, the choice of treatment method is again subjective, and mainly depends on the availability of this or that equipment in the clinic where you went, the experience and preferences of the doctor involved in your treatment. Additional objective criteria can be obtained in the process of examining the vessels of the lower extremity using Doppler ultrasound and duplex scanning of blood vessels (these examinations are currently mandatory in the standard examination of patients with varicose veins). Dopplerography methods make it possible to clarify the prevalence of varicose veins, the consistency of the vein valves at different levels, the condition of the deep and perforating veins (the joints between the superficial and deep venous system of the limb). But, again, there are no uniform and unambiguous global standards; these are simply additional factors taken into account by the doctor when choosing a treatment method based on his own clinical experience. For example, if the diameter of the trunks of the great or small saphenous vein is more than 10 mm, sclerotherapy is not recommended by most specialists. In specialized phlebological clinics, combined treatment is often carried out using several of the above methods.
Contraindications for sclerotherapy of veins
- pregnancy and lactation
- allergic reactions to sclerosing drugs
- severe atherosclerosis of the arteries of the lower extremities
- current thrombophlebitis (acute thrombosis of deep or superficial veins)
- repeated previous thrombosis (relative contraindication)
- some heart defects (particularly patent foramen ovale)
- inflammatory or infectious skin diseases in the area of proposed injections (pyoderma, boils, etc., a relative contraindication)
Preparing for the sclerotherapy procedure
- It is not recommended to drink alcohol and smoke for 2 days before and after sclerotherapy
- It is not recommended to perform hair removal or use lotions and creams on the eve of the procedure.
- It is recommended to take a hygienic shower immediately before the procedure
- It is recommended to eat lightly 1.5-2 hours before sclerotherapy
In addition, you must inform your doctor if you are taking hormonal drugs (contraceptives, estrogens, etc.) and stop taking aspirin, trental, ibuprofen and other anti-inflammatory drugs 2 days before starting treatment.
Sclerotherapy technique
For sclerotherapy, special needles have been developed, the diameter of which is 0.2-0.5 mm, which makes the procedure almost painless, although discomfort during the procedure is possible, and the smaller the diameter of the vessel, the greater the likelihood of such discomfort. Given the low-painfulness of the procedure, sclerotherapy in all modifications is carried out on an outpatient basis and does not require anesthesia.
Before sclerotherapy, with the patient in an upright position, varicose veins and telangiectasias (presumed injection sites for the drug) are marked. Next, the patient lies down on the couch. After treating the skin with a disinfectant solution, a vein puncture and aspiration test are performed to confirm the location of the needle tip in the vein lumen. After this, a sclerosing drug is administered. Several injections are performed per session, the number of which depends on the form of varicose veins (from 3-7 for main forms of varicose veins, to 10-20 injections for multiple telangiectasia and widespread reticular varicose veins).
During echosclerotherapy of large main veins, injections of the drug are performed under the control of an ultrasonic sensor, which makes it possible to control the penetration of the needle into the vessel and monitor the spread of foam throughout the vessel. The sensor can be used by the surgeon performing the procedure, or an assistant can participate in the therapy session.
When performing microsclerotherapy for single small foci of varicose veins or single telangiectasia, further compression is not required. In other cases, elastic compression of the lower extremities to the foot is performed with latex pads, elastic bandages or special compression hosiery.
Each sclerotherapy session takes no more than 10-20 minutes. Depending on the extent of the process, from 1 to 5 (on average 2-3) procedures may be required.
The rehabilitation period after sclerotherapy
Immediately after the procedure, the patient is prescribed a mandatory one-hour walk. If there are no adverse reactions, the patient is sent home, where he can lead his usual lifestyle. In the first three days after sclerotherapy, you should not engage in aerobics, gymnastics or on an exercise bike. No other serious restrictions on physical activity and work are provided. It is recommended to walk for at least 1 hour every day, avoid prolonged standing or sitting if possible, not take hot baths for 2 weeks and not visit the sauna for 1.5-2 months. With the exception of microsclerotherapy options for single pathological lesions, elastic compression is necessary throughout the entire treatment period and up to 1-3 months after the last injection. In this regard, many experts recommend performing sclerotherapy not during the hot summer period.
Complications of sclerotherapy
- skin itching, usually disappears 1-2 hours after the procedure, but in some cases it can occur sporadically for several days
- temporary pigmentation (darkening) of the skin along the sclerotic vein is observed in 5-8% of patients, sometimes it can persist up to 1 year after the procedure
- epidermolysis is a burn of the skin at the injection site, with necrosis of the upper layer of the dermis, associated with the penetration of a sclerosing drug under the skin. As a rule, it goes away on its own without cosmetic defects.
- peeling of the skin is observed in less than 1% of cases, while a small superficial wound forms at the injection site, healing without a trace after 2-4 weeks
- pain at the injection sites or along the sclerotic vein is noted in a small number of cases. Nagging pain at injection sites usually occurs during physical activity and can last for 3-9 days
- in rare cases, 2-4 weeks after treatment, a thin reddish vascular “mesh” may appear along the sclerotic vein, usually disappearing on its own within 4-6 months
- short-term swelling in the ankle area can be observed during treatment of varicose veins and spider veins located in that area, as well as when wearing high-heeled or narrow shoes during treatment
In a very small percentage of cases, more serious complications may occur:
- paravasal necrosis is an area of necrosis (tissue destruction) of varying depth associated with the penetration of a sclerosing agent under the skin. After healing, cosmetic skin defects remain
- thrombophlebitis - inflammation of the superficial vein into which the drug was injected, occurs during sclerotherapy of large veins. Disappears with stronger local compression.
- deep vein thrombosis is the most serious complication, but it occurs very rarely, according to medical statistics, even less often than after surgical treatment.
Results of treatment using sclerotherapy
Despite the development of a large number of new, high-tech methods for treating varicose veins, there are currently no methods that can guarantee and permanently get rid of this disease. Relapses of the disease are possible, including after sclerotherapy. The probability of relapse and the need to undergo re-treatment after 5-10 years with sclerotherapy is approximately the same as after other methods, including surgical ones.
Sincerely, YOUR DOCTOR!
← previous article archive of articles next article →
Indications for sclerotherapy (scleroobliteration) of veins
Any varicose vein can be successfully treated with endovenous chemical obliteration. The emergence and availability of modern minimally invasive methods of thermoobliteration (EVLO, RFO) has somewhat narrowed the range of applications of sclerotherapy (scleroobliteration) of veins in Moscow. But it remains still relevant, and sometimes irreplaceable.
Most often the indications are as follows:
- The presence of reticular varicose veins and telangiectasias is often an aesthetic problem; sometimes bleeding from these vessels is indicated.
- Isolated varicose veins of the tributaries of the small or great saphenous veins.
- The presence of pathological reflux in the perforating veins, after its elimination in the main ones.
- If other treatment methods are contraindicated for patients with the stem form of varicose veins. It has been proven that the intervention is effective even when the diameter of the ostial valve of the great saphenous vein is up to 30 mm.
Patient examination
Sclerotherapy is a minimally invasive method of treating varicose veins. A contraindication to sclerotherapy is the presence of somatic diseases that can affect the results of the procedure and the rehabilitation process. For this reason, doctors at the Yusupov Hospital conduct a comprehensive examination of the patient on the eve of vein sclerosis, which includes the following studies:
- General blood analysis;
- General urine analysis;
- Blood test for the presence of antibodies to the causative agent of syphilis, hepatitis B and C, HIV;
- ECG diagnostics;
- Fluorography;
- Dopplerography of the vessels of the lower extremities;
- Determination of blood group and Rh factor;
- Blood test for clotting.
Doctors make the decision to perform the procedure if there are no changes in the tests and research results. A contraindication to sclerotherapy is a blood clotting disorder, so doctors recommend that patients a few days before the procedure refrain from taking nonspecific anti-inflammatory drugs and agents that can increase bleeding. If the patient is taking hormonal medications, he must notify the phlebologist about this.
Make an appointment
Contraindications for sclerotherapy (scleroobliteration) of veins
Like every treatment method, sclerotherapy has contraindications.
Absolute:
- Cardiopulmonary failure.
- Allergy to sclerosant.
- Thrombosis of deep and superficial veins.
- Thrombophilia.
- Pregnancy and lactation period.
- Inflammatory processes in the procedure area.
- Sedentary patients.
- Open oval window in the heart (for foam form).
- If varicose veins are the only route of blood outflow from the lower extremities (10% PTF).
Relative:
- Hormonal therapy.
- Proximity to long flights.
- Ischemia of the lower extremities.
- Obesity and lymphostasis.
Doctors performing sclerotherapy
Bylov Konstantin Viktorovich
Cardiovascular surgeon
23 years of experience
Make an appointment
Malakhov Yuri Stanislavovich
Doctor - cardiovascular surgeon, phlebologist, Honored Doctor of the Russian Federation, Doctor of Medical Sciences, doctor of the highest category
Experience 36 years
Make an appointment
Technique for sclerotherapy (scleroobliteration) of veins
The sclerotherapy technique is non-traumatic and does not require hospitalization or changes in the usual rhythm of life, and is well tolerated by patients.
One-handed sclerotherapy technique
The session is performed in a horizontal position. Sometimes it is necessary to create an elevated position of the limb. Injections are performed with the thinnest 27-30G needles, so they are practically not felt by patients. After treating the skin with an antiseptic solution, sclerosant is injected into the lumen of the veins. Depending on the caliber of the vessels and their location, a liquid or foam form of one concentration or another is used. The introduction is carried out slowly to avoid stretching and rupture of the vessel. For additional visualization, ultrasound guidance or a venovisor can be used.
Use of modern methods of vein visualization
After the injections, bandages are applied to the skin along the veins, and class 1 or 2 compression hosiery is worn.
Reasons for the development of the disease
Experts say the main cause of spider veins is hormonal imbalance in the body. In addition, they can develop with problems with the heart or blood vessels and pathology of other organs.
Fact! Genetic predisposition also plays a very important role. Therefore, if one of your relatives already suffers from varicose veins, then you should lead a healthy lifestyle, monitor your diet and physical activity to reduce the risk of developing the disease.
Recommendations after a session of sclerotherapy (scleroobliteration) of veins
The length of time to wear knitwear is determined by the diameter of the sclerosed veins. At the end of the session, the patient is shown walking for 15-20 minutes, and subsequently, every day, patients must perform certain exercises for the lower extremities. Walking, cycling and light aerobics are ideal exercises after sclerotherapy.
There are also limitations during the course of treatment, namely:
- visiting baths, saunas;
- long-term static loads;
- sunbathing;
- long flights (a week after the session);
- hair removal (week after the session).
Rehabilitation period
The process of treating varicose veins using sclerotherapy is not a one-step process. To achieve results, a certain rehabilitation period must take place. It is individual for each patient and depends on the characteristics of a particular organism. The main condition for high-quality recovery is the patient’s self-control and discipline.
After sclerosis, local aseptic inflammation occurs in the venous wall (without the participation of microorganisms). During this period, the patient may experience pain in the leg, swelling may develop, and minor hemorrhages may appear. This is a normal course of the recovery period. For severe pain, your doctor may prescribe acetaminophen. You should refrain from taking non-steroidal anti-inflammatory drugs. Swelling after sclerotherapy decreases when the patient lies down for 15 minutes with his leg elevated at an angle of 15°.
During the recovery period after sclerotherapy, bruises may appear at the injection sites. They first have a characteristic bluish color, but over time they become yellow. Approximately 7-10 days after the procedure, the skin acquires its normal color. Wearing compression stockings can prevent bruising and speed up the process of bruising. In 5-10% of cases, hyperpigmentation of the skin occurs at the injection sites of drugs during the recovery period after sclerotherapy. It does not require treatment and goes away on its own after 2-3 months.
Make an appointment
Complications and side effects of sclerotherapy (scleroobliteration) of veins
- Hyperpigmentation - occurs due to the deposition of hemosiderin in the superficial layers of the skin, is an infrequent side effect of sclerotherapy, and usually goes away on its own within 6-12 months.
- Local edema - occurs as a result of the administration of significant doses of the drug in a small area, and regresses on its own.
- Transient neurological complications: migraine, loss of visual fields - can occur when using a foam form of sclerosant. Self-limited within 10-15 minutes.
- Metting (secondary, recurrent telangiectasias) – incidence up to 15%.
In most cases, they disappear spontaneously within a few months.
- Nerve damage is a fairly rare complication and occurs due to the close proximity of the nerve branches to the trunks of the GSV and SVC. It often goes away on its own.
- Skin necrosis - can occur due to the substance entering the paravasal tissue or small arteries. This complication is extremely rare.
- Thrombotic complications (thrombophlebitis, deep vein thrombosis, pulmonary embolism) are extremely rare.
- Allergy, anaphylaxis. As with any drug, a reaction is possible. Fortunately, they are quite rare.
In the vast majority of cases, the only thing that worries patients is small hematomas at the injection sites. They dissolve within a week.
Drugs
Sclerotherapy of varicose veins is performed by administering liquid and foam preparations. At the Yusupov Hospital, doctors use sclerosants for sclerotherapy, registered in the Russian Federation. They are effective and have a minimal range of side effects.
Drugs that are used for sclerotherapy, after being introduced into the lumen of a venous vessel, affect the inner layer of the vein and cause denaturation of the protein of the inner lining. The lumen of the vein collapses, the walls “stick together”, it becomes empty and is replaced by connective tissue.
There are 3 groups of drugs for sclerotherapy:
- Detergents;
- Osmotic solutions;
- Corrosives.
Detergents are surfactants. They are capable of destroying intercellular tissue within a few seconds. The first signs of the effects of osmotic solutions are visible 5 minutes after injection of the drug into the lumen of the vein, and the maximum result is achieved after 30 minutes. The phlebosclerosing effect of the drugs directly depends on the saturation of the solution. Corrosive drugs act simultaneously on the internal and muscular layers of the vein.
The following drugs for vein sclerosis are registered in the Russian Federation: thrombovar, ethoxysklerol, fibro-vein. The main advantage of thrombovar is its availability and attractive price. After administration of the drug, side effects often develop: allergic reactions, pain. For this reason, doctors at the Yusupov Hospital do not use this medicine for sclerotherapy.
Ethoxysclerol has a strong adhesive effect and has a minimal range of side effects. The drug is used for sclerosis of reticular veins, spider veins, small tributaries and perforating veins. Fibro-vein is characterized by high phlebosclerosing activity. It is used for sclerotherapy of large veins. The drug can have significant side effects: skin necrosis and hyperpigmentation.
Advantages and disadvantages of foam sclerotherapy for veins
For Foam-Form sclerotherapy, doctors use fine foam, which is obtained by mixing gas (oxygen, carbon dioxide, air) with a sclerotherapy solution. The foam consists of a large number of gas bubbles, the wall of which is a sclerosing agent. It displaces blood from the vessel, thereby ensuring the effect of an empty vein. The foam, remaining in the lumen of the vein until the bubbles disintegrate, acts on the vessel wall much longer than the sclerosant in its natural form.
The main difference between the action of the foam is the pronounced persistent spasm of the venous vessel, which it fills despite the fact that the initial concentration of the liquid drug used to obtain the foam is low. The diameter of the vein can decrease by 5 times. As a result of spasm of the vein in the vessel, sclerophlebitis develops, rather than classic thrombophlebitis (red blood clot).
Foam-Form sclerotherapy has the following advantages:
- More complete contact of the sclerosant with the venous wall is ensured, due to the absence of blood in the lumen of the vessel;
- The volume of the drug is increased due to gas, which allows you to reduce the dose of its natural form and reduce the cost of the procedure;
- Thanks to the use of a drug of lower concentration, which ensures the effect of scleroobliteration, the risk of complications (skin necrosis and pigmentation) is reduced;
- The duration of contact of the foam solution with the vein wall and the length of the sclerosed zone increases in comparison with classical therapy;
- The phlebologist has the ability to carry out echo control of the process of administering the sclerosing drug and its distribution throughout the venous network.
Some patients, due to individual intolerance or other reasons, extremely rarely develop adverse reactions and complications of foam sclerotherapy. In terms of time of occurrence, they can be early (develop directly during the procedure) and late (appear after several hours or even days), and in terms of severity - mild and severe. Allergic reactions may occur in patients prone to allergies. They manifest themselves as urticaria or mild bronchospasm and go away on their own within 30 minutes.
Nausea, dizziness and fainting, a feeling of lack of air and tightness in the chest are the result of vascular spasm or a psycho-emotional reaction. More common during venous puncture and insertion. Sometimes doctors accidentally inject a sclerosing agent into an artery or nerve. Phlebologists at the Yusupov Hospital are fluent in the technique of foam sclerotherapy and do not allow technical errors when performing the procedure.
An extremely rare complication of foam sclerotherapy is visual disturbances (double objects, flickering “spots” and blurred vision). It occurs when foam bubbles move from the right side of the heart to the left, due to the presence of septal defects (oval window, atrial or ventricular septal defect), and from there into the systemic circulation and into the cerebral vessels. At the Yusupov Hospital, before performing foam sclerotherapy on a patient, doctors conduct a comprehensive examination to exclude concomitant pathologies that increase the risk of complications.
Make an appointment
Aesthetic sclerotherapy (scleroobliteration) of veins
Convenience and efficiency have allowed sclerotherapy to become not only a therapeutic, but also a cosmetic procedure. The method is the most effective for the treatment of telangiectasias and the only one for eliminating reticular varicose veins. In recent years, Russia has seen a kind of boom in aesthetic phlebology.
Scleroobliteration of veins using the Venolight device
Many representatives of the fair sex dream of beautiful legs, cleared of spider veins and spider veins. Sclerotherapy of the veins of the lower extremities copes with this task perfectly. Since the main limitation is wearing compression garments, it is optimal to carry out treatment in late autumn or winter. Elimination of telangiectasia and reticular veins has cosmetic purposes, but patients at the same time have symptoms of venous stagnation, so the effect of treatment is often pleasantly surprising with an improvement in well-being.
Rehabilitation
Immediately after the procedure, a pressure elastic bandage is applied or special knitwear is put on. To prevent possible damaging effects of the drug on the endothelium after the procedure, vigorous walking for 2 hours is recommended. For three days after the procedure, you cannot seriously load your legs or play sports. In the first two weeks, it is forbidden to lie or sit for a long time. Overheating of the affected area is eliminated for 1.5-2 months. Compression stockings or bandages are worn for 1-3 months. Otherwise, the patient can lead a normal lifestyle: do household chores, go to work.
Sclerotherapy of the hands (removal of unsightly veins on the hands) in Moscow
It’s no secret that with age, the skin of women’s hands becomes thinner, fluid is lost, and tissue turgor decreases. Against the background of these changes, clearly visible, unaesthetic veins of the back of the hand and forearm often appear. Skin lasers cannot treat these veins due to the diameter of these vessels. Sclerotherapy easily eliminates them.
Results of removal of unsightly veins on the arms in our clinic. Photos before and after.
Before a sclerotherapy session on your hands
After a sclerotherapy session on the hands
Until recently, patients had to travel to Europe with similar problems. Hand sclerotherapy is now available in Moscow, in our clinic. Doctor Semenov Artyom Yurievich, one of the first in Russia to use this technique, and his results are in no way inferior to his foreign colleagues. Today he has the most experience in sclerosing veins in the arms in our country.
Sclerotherapy (scleroobliteration) of veins in Moscow - prices for procedures
At our center in Moscow, prices for sclerotherapy procedures are strictly fixed, and therefore, when visiting our clinic, patients can count on high-quality service, treatment and an affordable cost. And remember that timely consultation with a doctor will completely cure the disease and avoid its recurrence.
Over the years, our center’s pricing policy has been characterized by loyalty to patients. It is enough to note that the cost of the latest medical services in our phlebology center has not increased since 2014. At the same time, more modern and advanced treatment and diagnostic technologies have appeared in the clinic during this time.
| Service | Treatment category | Price |
| Sclerotherapy (microsclerotherapy) on one lower limb (one session) | Reticular varicose veins and spider veins | 8000₽ |
| Postoperative sclerotherapy (microsclerotherapy) on one lower limb (one session) | Reticular varicose veins and spider veins | 4000₽ 8000₽ |
| Sclerotherapy (microsclerotherapy) on one lower limb (course of treatment) | Does not depend on the number of sessions | 35000₽ |
| Removal of unaesthetic veins on one arm (one session) | 10000₽ | |
| Laser removal of spider veins on one lower limb (one session) | 10000₽ |
For the convenience of our patients, we work with banks that offer credit lines. Also in our center there is a flexible system of discounts and installments. Payment by Visa and Mastercard is possible. At the end of the course of treatment, the patient is given a package of documents to submit to the tax office for tax deduction.
Sclerotherapy is an excellent remedy for varicose veins on the legs!
Sclerotherapy has begun to appear more and more often in Moscow clinics. Indeed, she:
- popular,
- effective,
- safe.
This is an excellent remedy for varicose veins on the legs. This procedure involves the introduction of a specific drug into the diseased vein. If certain conditions are met, this sclerosant practically “seals” the vein. Over time it will disappear completely
This procedure continues for a long time. Sometimes it provides a decent cosmetic effect even for life. You just need to contact one of our phlebolic doctors for help. They will definitely select a course of treatment.
Our competitive advantages and the best remedy for varicose veins on the legs
Sclerotherapy is an excellent investment. With a little patience and courage, you will get excellent legs: slender, light, capable of moving long distances. When you contact a doctor, you need to inform him about all the chronic diseases, infections, and so on that you currently have.
Next, the phlebologist will recommend the best remedy for varicose veins on your legs. He will definitely help you prepare, go through all the examinations, and then return to normal, everyday life. You will definitely receive detailed instructions on how to behave after the operation. With our help, you will definitely return to an active life!
Advantages of the sclerotherapy method on the lower extremities
Vein sclerotherapy (scleroobliteration) is a surprisingly well-tolerated non-surgical procedure that can eliminate both small and large varicose veins. Phlebologists who master the technique practically do not encounter any complications. That is why sclerotherapy has firmly entered the arsenal of modern specialists and continues to improve.
The result of sclerotherapy for varicose veins immediately after the session
Our phlebologists have one of the most extensive experience in treating varicose veins using sclerotherapy. Tens of thousands of successfully treated patients passed through their hands!
Advantages and disadvantages of the technique
The main advantage of sclerotherapy is the minimally invasive nature of the intervention - all manipulations are practically painless and are carried out through a puncture of the skin with a needle under visual and ultrasound control.
The main disadvantage of the procedure is considered to be a fairly high risk of relapse. As a result of recanalization, a vein treated with sclerosant may be reintroduced into the blood circulation, and new ones may appear in place of previously sclerosed ones due to the progression of the disease.
Treatment of varicose veins without surgery
Operation time - 10 minutes
Hospital recovery - not required
Cost of the operation: from 4,050 rubles.
Results of treatment of patients using sclerotherapy (sclerotherapy) of veins. Photos before and after treatment.
The result of treatment of a patient in the phlebology clinic "MIFC" using the method of compression sclerotherapy of veins
Photos before and after sclerotherapy (sclerotherapy) of leg veins
Result of varicose vein removal using compression sclerotherapy
Photos before and after sclerotherapy (sclerotherapy) for varicose veins on the legs
Preparing for treatment
No special preparation is required from the patient. We do not recommend using sclerotherapy for women during menstruation. This treatment method should not be used by pregnant women.
Before sclerotherapy, the doctor’s task is to perform an ultrasound scan of the veins and carefully mark all pathologically dilated veins and determine the sites of proposed injections.
Before treatment, the doctor should question the patient about concomitant diseases, allergic reactions to medications, thrombophlebitis and a history of deep venous thrombosis.
Frequently asked questions from patients on the Internet about sclerotherapy (sclerotherapy) of veins in Moscow
How much does sclerotherapy of the veins of the lower extremities cost in Moscow? Svetlana asks from Moscow:
Dear Svetlana! The cost of sclerotherapy (scleroobliteration) of the veins of the lower extremities in Moscow can vary significantly in different medical centers. Some city phlebological centers charge for the removal of each asterisk using scleroobliteration; in some clinics, patients pay for the procedure for each separate segment of the lower limb. This pricing policy is often extremely unprofitable for the patient. At the Moscow Innovative Phlebological Center, the price is charged for the scleroobliteration procedure on the entire lower limb, since the doctor carries out treatment to the maximum extent at each sclerotherapy session. The cost of a sclerotherapy procedure on one lower limb in our Moscow Medical Phlebological Center is 8 thousand rubles.
You can find out detailed information about prices for innovative procedures by phone or on our website page:
Where is the best place to do sclerotherapy of the lower veins in Moscow? Natalia from Moscow is interested in:
Dear Natalia! Sclerotherapy (scleroobliteration) of veins in Moscow is best done in a good phlebological center. In a medical institution that professionally deals with venous pathology, you will definitely undergo a full examination of the venous system before the sclerotherapy procedure. After a good modern diagnosis, the doctor will sign you up for a sclerotherapy session and explain how many procedures will be required to achieve the optimal cosmetic effect.
What is the price of the procedure for sclerotherapy of the veins of the lower extremities at the Moscow Phlebological Center? Asks Valentina from Moscow:
Dear Valentina! The cost of one sclerotherapy procedure for the veins of the lower extremities at the Moscow Innovation Phlebological Center is 8 thousand rubles. The price of the scleroobliteration procedure in our innovative phlebology clinic remains one of the most affordable in Moscow. It is worth noting that the cost of the procedure has not changed since 2014. The session is performed by an experienced specialist who has thousands of similar procedures under his belt. We work according to European standards, so we guarantee the high efficiency and safety of each scleroobliteration procedure.
Where to do vein sclerotherapy in Moscow, as you can tell from reviews? Irina from Voskresensk asks:
Dear Irina! Vein sclerotherapy in Moscow is performed by a huge number of public and private medical centers. Only a few have truly good results from this innovative procedure. The fact is that the technique is largely operator dependent, and the experience of the specialist performing the procedure is of great importance. Therefore, we recommend reading reviews from patients who have already undergone sclerotherapy. You can read reviews of patients who underwent innovative treatment at the Moscow Medical Innovation Center on the page of our website:.
How effective is vein sclerotherapy? Marina from Tver is interested:
Dear Marina! Sclerotherapy or scleroobliteration of veins is a very good modern procedure for removing unaesthetic venous vessels. This treatment technology has earned recognition and trust from leading European specialists. To achieve a good result, strict adherence to procedure protocols is required. Repeated procedures are often necessary to achieve the desired effect. These disadvantages exist, but when performed correctly, sclerotherapy is the best technique for removing telangiectasia and reticular veins.
What can spider veins lead to?
In themselves, such formations do not pose a threat to health. In rare cases, they are accompanied by pain, swelling or bleeding, causing physical discomfort. Telangiectasia can remain only an aesthetic problem if the factor that caused it is eliminated.
However, there are situations when altered vessels are a nonspecific sign of chronic venous insufficiency or severe somatic pathology. It is impossible to make a diagnosis on your own. Finding out the cause of telangiectasia and starting treatment is the doctor’s task.