Varicose veins Signs, symptoms, causes. When to see a doctor, what questions to ask. Signs, symptoms, causes. When to see a doctor, what questions to ask. Examinations, tests and procedures for diagnosing varicose veins. Treatment of varicose veins. Vein care and prevention.
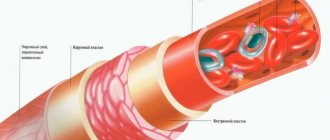
Veins are blood vessels that carry blood to the heart. Varicose veins occur most often on the legs and thighs. Thickened, twisted, or dilated sections of the vein are called varicose veins. As a rule, it is inherited and becomes more noticeable as a person ages.
Causes of varicose veins
There are many theories about why varicose veins occur, but the consensus is that defective/damaged valves in the veins are the cause. The valves prevent blood from flowing back inside the vein. They keep blood in the vein, which moves towards the heart. It is not clear what causes the valves to operate less efficiently. Some experts believe that the problem is hereditary. Some people may be born with abnormal vein walls.
Varicose veins can be aggravated by many factors:
- Pregnancy
- Prolonged standing
- Overweight
- Tension: Chronic constipation, urinary retention, chronic cough or any other condition that forces a person to strain for a long period of time causes an increase in the forces transmitted to the veins of the legs. These mechanisms also contribute to the formation of hemorrhoids, which are varicose veins located in the rectal and anal areas.
- Previous surgery or leg injury: These conditions interfere with normal blood flow through the channels.
- Age: In general, most older people experience some degree of varicose veins.
When to see a doctor about varicose veins
If a person has varicose veins and has any of these symptoms and signs, they should see a doctor.
Inflammation, discoloration or ulceration of the skin or swelling of the calf or leg are more common with problems involving the deeper veins, especially a blood clot. Unexplained pain or swelling in the leg, in particular, suggests a blood clot. Varicose veins by themselves usually do not cause leg swelling.
Varicose veins themselves are relatively harmless, but can cause minor problems from time to time. If the skin covering the vein is thin or irritated, minor trauma from a blow or even shaving can cause bleeding. In this case, raising the leg and applying pressure for a few minutes should be enough to stop the bleeding. If, at any time, the patient feels chest pain or has trouble breathing, this may indicate the presence of a blood clot in the blood vessels of the heart or lungs.
Having varicose veins does not necessarily mean that a person will eventually develop a blood clot or that the blood clot somehow caused them. However, in rare cases, a clot increases pressure in the veins, blocking blood flow. This increased pressure will cause blood to flow back through weakened valves, creating varicose veins.
Are your legs bothering you? Check your blood vessels! Who can benefit from ultrasound scanning of lower extremity vessels?
Spider veins, swelling, a feeling of heaviness in the legs - these signs can be, in particular, a manifestation of vascular diseases of the lower extremities. Ruslan Akhyaevich Bidzhiev, ultrasound diagnostics doctor at Clinic Expert Stavropol, talks about in which cases ultrasound scanning of the vessels of the legs should be performed and how this study is performed.
— Ruslan Akhyaevich, Ultrasound scanning of the vessels of the lower extremities - what kind of study is this?
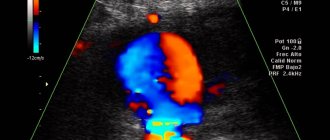
- This is a modern, highly informative method for identifying pathological changes in the vessels of the legs - arteries and veins. The abbreviation “UZDS” stands for “ultrasonic duplex scanning”.
I would like to note that until recently, Doppler ultrasound (USDG) was considered one of the widely used diagnostic procedures for assessing the condition of the vessels of the extremities. However, with its help it was possible to evaluate only one indicator - the patency of the vessel.
Unlike ultrasound doppler scanning, duplex ultrasound scanning of leg vessels allows you to visualize in detail the condition of the vascular wall of both large arteries and veins and small ones, identify the presence of blood clots and atherosclerotic formations, and determine the speed, direction and intensity of blood flow in the vessels. That is, we have the opportunity to obtain more detailed information.
— For what symptoms is ultrasound scanning of the vessels of the lower extremities performed?
— The main complaints of patients for which ultrasound scanning may be prescribed are pain and swelling of the legs. Redness of the skin, spider veins, various compactions (especially in the popliteal region), nodules in the projection of the vessels of the legs can also serve as a reason for prescribing this study.
Typically, ultrasound duplex scanning of the arteries and veins of the lower extremities is prescribed to the patient by the attending physician - a vascular surgeon, cardiologist, neurologist, therapist, traumatologist.
— In the diagnosis of what diseases can ultrasound of the arteries and veins of the lower extremities help?
— Vascular surgeons and phlebologists prescribe it to detect varicose veins, phlebitis (inflammation of a vein), superficial and deep thrombosis (phlebothrombosis and thrombophlebitis).
After operations on the lower extremities, ultrasound scanning is used to monitor the consistency and quality of the performed manipulations. Traumatologists prescribe duplex scanning to prevent thrombosis of the vessels of the lower extremities, associated either with compression of the vessels by a plaster cast or with a blood clotting disorder.
Ultrasound scanning will also be informative in case of some heart pathologies, after chemotherapy, and will also help to distinguish some infectious diseases from vascular pathology (in particular, erysipelas from thrombosis). In addition, this research method makes it possible to detect traumatic injuries and anomalies in the structure of blood vessels, intervascular malformations (connections).
— Do I need any preparation for ultrasound duplex scanning of the vessels of the lower extremities?
- No.
— How is ultrasound scanning of the vessels of the lower extremities performed?
— Traditionally, this study is performed in various projections. Despite the fact that, according to generally accepted recommendations, the patient is examined in a standing position during ultrasound scanning, practice shows that sometimes this is not enough, so our clinic provides a more expanded and thorough approach to this issue.
I would like to emphasize that we carry out diagnostics step by step, relying in our work on the laws of physics. First, the patient is placed on the couch. After normalizing the blood pressure, we perform an ultrasound scan of the femoral vessels, then the patient turns over on his side and the back of the thigh and lower leg are examined.
The next stage is to examine the patient’s limbs in a standing position, that is, under load. If necessary, we perform the examination in a sitting position.
— Does it happen that to clarify a patient’s diagnosis, ultrasound duplex scanning of the vessels of the legs is not enough, and some other research methods are required? And if so, which ones?
— Today, ultrasound scanning is one of the most informative diagnostic methods, which, by the way, is considered the gold standard for studying the blood vessels of the legs. In my opinion, the best method for detecting and assessing pathologies of the veins of the extremities has not yet been invented. To confirm this, I would like to add that, based on our conclusions, traumatologists, vascular surgeons, and cardiologists prescribe treatment and successfully perform operations.
Traditional angiography or CT angiography may also be prescribed to assess the condition of the arteries.
If necessary, the attending physician may additionally recommend that the patient undergo laboratory blood tests. Among them, in particular, assessment of blood clotting indicators (including prothrombin index) and a number of other studies.
You can sign up for ultrasound duplex scanning (USDS) of blood vessels here. ATTENTION: the service is not available in all cities
Interviewed by Sevilya Ibraimova
The editors recommend:
Doppler, duplex, triplex... What types of vascular ultrasound are there? Ultrasound of neck vessels: when is it prescribed? When is ultrasound of cerebral vessels prescribed? When is CT angiography needed?
For reference:
Bidzhiev Ruslan Akhyaevich
Graduate of the Faculty of Medicine of Stavropol State Medical University in 2015.
In 2021, he completed an internship in the specialty “Therapy with a course in dietetics.”
He completed training and advanced training courses in ultrasound diagnostics at the FMBA research center (Moscow).
Currently holds the position of ultrasound diagnostics doctor at the Expert Clinic, Stavropol. Receives at the address: Dovatortsev St., 39A.
Examinations, tests and procedures for diagnosing varicose veins
Diagnosing varicose veins is relatively easy. They are easily recognized simply by their characteristic appearance upon physical examination. The healthcare provider will likely perform a thorough medical history and examination, looking not only at the extent of the patient's varicose veins, but also at potential risk factors.
Any of several simple tourniquet tests can be done to determine the points of reflux.
Another useful device to help localize the extent of the problem is Doppler ultrasound. This test can rule out the presence of clots in deeper veins.
Magnetic resonance venography is another test performed when the duplex scan test is unclear. This test can even look for blood clots in the deep veins.
Blood tests (laboratory) are not helpful in diagnosing varicose veins.
Follow-up care after a diagnosis of varicose veins is usually only necessary if a person is considering surgery or sclerotherapy. Otherwise, contact a healthcare professional only if symptoms become severe or worsen.
Caring for varicose veins at home
- Raise your legs as high as possible. If possible, take half-hour breaks throughout the day to rest. It is very important to raise your legs above heart level to get the maximum effect, and do this for about half an hour each time.
- Wear compression stockings.
- If you are overweight, try to lose weight. Eat a high-fiber, low-fat, low-salt diet.
- Avoid alcohol.
- Contact your doctor if you have health problems such as chronic constipation, urinary retention, or chronic cough.
- Avoid wearing tight clothing such as belts or belts.
- Don't cross your legs when sitting.
- Walking more is good exercise and can help the muscles push blood out of the deeper venous system.
What methods can be used to examine blood vessels in the legs?
Modern medical practice knows quite a few different ways to determine pathologies of the blood vessels of the legs. How are methods for diagnosing blood vessels of the lower extremities classified? What is the essence of functional research methods? What diseases can be determined using different types of research?
First of all, a distinction is made between invasive and non-invasive methods.
The second classification provides for the division of all diagnostic methods into the following groups:
•Functional;
•Ultrasonic;
•Tomographic;
•X-ray;
•Computer.
Treatment of varicose veins
Sclerotherapy involves injecting a chemical into a vein, which occludes it and causes scarring. Sclerotherapy is not entirely successful in relieving symptoms and preventing more varicose veins from forming. Complications associated with sclerotherapy include allergic reactions to the chemical used, burning or stinging at various injection sites, inflammation, skin ulcers, and permanent skin discoloration. Wearing compression stockings is usually recommended after sclerotherapy. Doctors who perform this procedure must have special training and experience to avoid complications.
Lasers are used as treatment for veins, but are often used in the treatment of smaller veins, medically called telangiectasia (local over-dilation of small vessels). These veins are small, measuring only up to 1 millimeter in diameter, and are dilated capillaries. Using lasers to treat these small vessels may cause changes in skin color or texture. Often multiple treatments are required. This technique is less useful in treating large varicose veins.
If a person has superficial thrombophlebitis, the doctor usually recommends warm compresses and pain medications. Additional treatment depends on whether the doctor thinks the patient may have an infection.
Surgical intervention for varicose veins
Several surgical procedures are available to relieve varicose veins, but not everyone with varicose veins is a candidate for surgery.
If the patient is pregnant or has recently become pregnant, it is advisable to wait at least 6 weeks after giving birth before considering this option because many varicose veins will disappear after pregnancy.
If the veins are only bothering the patient for cosmetic reasons and the patient is not concerned about pain or inflammation, then surgery may not be the best option.
Most surgical interventions are performed on an outpatient basis. The operation involves either ligating the vein (tying) or removing or retracting (pulling back) the smaller branches. There are risks and benefits to any surgery. These should be discussed with your doctor. Recurrence of varicose veins does occur and may be due to incompetent vein puncher or failure to ligate a vein in the groin.
Avulsion requires many tiny incisions and removal of varicose veins that have been outlined in the skin.
Vein stripping requires a recovery period of 5-10 days before returning to your regular routine. For just vein ligation, a few days off is more than enough. There is the possibility of permanent numbness from damage to the nerves in the skin (for this reason, only the vein up to the knee is usually exposed, and not the vein below the knee). The numbness is only mild and does not cause any future problems.
Endovenous laser therapy is a Lazarus method of destroying a vein. The procedure is usually performed in a doctor's office and takes about 30-45 minutes. A small laser is passed into the vein with guidance from an ultrasound machine. The laser is fired in several places, and the entire procedure is performed with some local anesthesia. Recovery is quick and involves minimal pain. The procedure is relatively new and, with the exception of some mild bruising and a feeling of numbness, no other effects were observed in the short term.
Radiofrequency ablation: Ablation is a similar technique to endovascular laser therapy, but it uses heat to destroy the vein. The probe is placed into the vein under ultrasound and, once in position, the vein is heated along its entire length. The procedure is performed under local anesthesia and takes about 30 minutes. Short-term results are excellent with radiofrequency ablation.
Ligation: Previously, this was a surgical treatment for varicose veins until the advent of the new treatments described above. It usually involved making an incision in the groin and tying off the saphenous vein where it enters the femoral vein. The procedure can be performed under local anesthesia.
The sooner a person begins the lifestyle changes described in the home self-care discussed earlier, the better the chances of preventing the formation of new varicose veins.
Prevention of varicose veins
A person cannot change their genes, but they can keep their weight under control, exercise, eat healthy foods high in fiber, and wear loose, comfortable clothes whenever possible. If a person is genetically predisposed to developing varicose veins, they may appear despite best efforts.
TED (thromboembolism - deterrent) stockings are the best non-surgical treatment for varicose veins. They prevent skin destruction and exacerbation of varicose veins. Most people have less swelling in their legs and less fatigue at the end of the day when using TED stockings.
Magnetic resonance angiography
Electromagnetic waves in a magnetic field help detect occlusions, aneurysms, stenoses, and atherosclerosis. Contrast agents are not needed for this type of diagnosis.
Multislice computed tomography
This method is used to study the vessels of the brain and lower extremities. To detect pathologies, X-rays are used. The tomograph displays the scanned vessels layer by layer on the screen. This produces a three-dimensional image, which clearly shows the condition of the veins and arteries and what the results of their regeneration are after the treatment.