Hypertensive crisis (HC) is a serious condition with serious consequences for health and life. The process develops against the background of increased blood pressure. If the readings on the tonometer are close to 200/100 mmHg. Art. and more, this means that the body is in danger and requires urgent medical attention.
The consequences of this serious condition in the form of varying degrees of damage to vital internal organs can be the most unpredictable (in 19 cases out of 100, premature death occurs with GC). The primary targets for high blood pressure are blood vessels and the heart.
The several-fold increase in the likelihood of heart attack and stroke is the main danger of a hypertensive crisis. According to statistics, 400 thousand cases of stroke resulting in severe disability are registered in the Russian Federation per year, 25% of them lead to premature death.
More than 65 thousand people die every year from myocardial infarction in the country, half of whom do not live to see emergency help. The recent rapid development of the pharmaceutical industry does not make the situation any easier, since official medicine cannot yet offer an effective way to solve the problem of the most common and deadly disease.
Competent therapy and qualified patient care will help prevent the development of such dangerous complications.
Responsibilities of medical staff
Qualified intervention for GC involves the provision of medical services taking into account the characteristics of the clinical picture of a particular patient. The responsibilities of the medical staff in this case include:
- First aid for relieving hypertension;
- Organization of conditions for normalization of blood pressure and recovery of the patient;
- Carrying out all medical procedures prescribed by a doctor;
- Helping the patient with everyday issues;
- Teaching the patient self-care in new conditions;
- Increasing awareness of the patient and his family about the characteristics of his disease.
Stages of the nursing process
In addition to service, the stages of nursing care include diagnosis, development of goals for nursing participation, agreement on a care plan and its implementation, and analysis of achieved results.
- Monitoring subjective information and analyzing real and potential patient complaints at the first visit will help plan care and rehabilitation.
- Drawing up a personal care plan for HC involves detailed development of short-term and long-term goals.
- Realization of goals. It is convenient to place all activities in a table, which indicates the date of the visit, the current problem, expected results, a list of services provided, and the reaction of the hypertensive patient’s body to manipulation.
- Analysis of the achieved result with adjustment of the patient’s living conditions. At this stage, it is advisable to discuss the results with the medical staff who took part in restoring the patient’s health.
Collection of information during the initial examination
A hypertensive crisis can be recognized by some general signs:
- Sudden changes in blood pressure;
- Increasing headache;
- Dizziness and weakness;
- The body trembles as if with a chill;
- Nausea not relieved by medication;
- Heart pain;
- Vision problems;
- Flushed face.
With such symptoms, the nurse, with the help of a third party, urgently calls a doctor, and while the ambulance team gets to the patient, they take urgent measures to alleviate his condition:
- Places the patient in a position convenient for such an illness: the head is raised with an additional pillow, while the legs should be lowered.
- The soles of the feet and shins are covered with a warm blanket; you can apply a heating pad or mustard plasters to the calf muscles.
- If the patient has a nosebleed, he should be reassured, as this is a good sign.
After the arrival of the ambulance and all the necessary procedures, the patient requires further professional care:
- The nurse should ensure strict adherence to bed rest.
- The diet must correspond to the diet; all food is prepared without salt.
- Provide the patient with conditions for deep and long sleep.
- Control bad habits, avoiding the consumption of strong and alcoholic drinks, smoking, and diet violations.
The health worker must behave with the utmost care and caution, since the patient after a crisis cannot contain his irritation, and he needs to create a calm environment.
Main aspects of the prevention of hypertension in the work of a general practitioner nurse
There has been a “rejuvenation” of cardiovascular diseases, which explains the current demographic situation in the country. The high prevalence of arterial hypertension in working age and young people leads to decreased performance and to such serious complications as myocardial infarction and stroke.
The concept of managing patients with arterial hypertension includes:
- early active identification of patients with minimal clinical manifestations of arterial hypertension and risk factors for its development;
- rehabilitation of patients with risk factors for developing arterial hypertension in order to reduce the risk of developing the disease;
- early diagnosis of arterial hypertension itself and its possible complications;
- early prescription of adequate drug and non-drug therapy;
- active physical rehabilitation of patients;
- training patients suffering from arterial hypertension and their relatives in the basics of maintaining health and preventing the development of complications.
Prevention of hypertension can be primary (aimed at the main predisposing factors) and secondary (aimed at preventing hypertensive crises and complications).
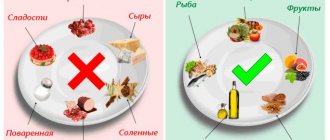
An important role in the prevention of arterial hypertension in patients is played by a general practitioner nurse, who, at an independent appointment, conducts patient questionnaires, anthropometric measurements, calculating body mass index, and measuring blood pressure in order to identify risk factors for the development of chronic non-communicable diseases. Based on the identified risk factors, the general practitioner nurse conducts individual preventive consultation on rational nutrition, physical activity, giving up bad habits, daily routine, healthy lifestyle and refers patients to health schools (see figure).
Primary prevention of arterial hypertension involves:
- increased physical and physical activity;
- to give up smoking;
- refusal to drink alcohol;
- limiting daily consumption of table salt;
- nutrition optimization;
- correction of body weight;
- adherence to sleep and wakefulness;
- exclusion of stressful conditions;
- avoiding being in a noisy environment.
Secondary prevention is carried out in patients in whom arterial hypertension is diagnosed. Its goal is to prevent complications from occurring. Moreover, this type of prevention includes two components: non-drug treatment of arterial hypertension and antihypertensive (drug) therapy. Non-drug treatment, in principle, corresponds to primary prevention, only with more stringent requirements. If each individual person is not able to change heredity and environment, then lifestyle and nutrition are quite possible. Drug therapy is drugs prescribed by a doctor that specifically act on high levels of blood pressure, reducing it. As mentioned earlier, patients with arterial hypertension should take such drugs for life, thereby preventing the risk of complications.
Planning
To organize the nursing process during a hypertensive crisis, the nurse must draw up a treatment plan:
- Determine the goal: reducing blood pressure over a certain period of time, which will depend on the patient’s condition and symptoms of the disease;
- Set deadlines for the implementation of short-term (lowering blood pressure, emergency therapy) and long-term goals (rehabilitation of the patient after discharge from the hospital or relief of a hypertensive crisis at home).
To plan medical intervention for a hypertensive crisis, it is important to consider the following nuances:
- Calling a doctor;
- Eliminating panic in the patient;
- The patient maintains a reclining position, with his head turned to one side (if attacks of nausea and vomiting are observed);
- Measurement of pulse, blood pressure, respiratory rate, heart rate and body temperature;
- Preparation of instruments and materials for performing medical procedures.
During the first 2 hours after an attack, blood pressure should be reduced by 25%. The tonometer reading should be no more than 160/100 mmHg. Art. Over the next 6 hours the situation should stabilize.
If the increase in blood pressure is not accompanied by symptoms of other diseases, and other organs and systems are functioning normally, emergency measures are not needed.
Health Research
Laboratory methods include:
- Clinical minimum;
- Blood test (biochemical);
- ALT, AST, lipoproteins, cholesterol, bilirubin, creatinine, total protein, coagulogram.
Instrumental research methods:
- ECG (to exclude the possibility of left ventricular hypertrophy, if atherosclerosis has joined, then it is necessary to check the symptoms of coronary artery insufficiency);
- FCG (emphasis of 2 tones on the aorta);
- EchoCG (to exclude the development of left ventricular hypertrophy);
- X-ray (assessment of the aortic configuration of the heart: the aorta may be elongated, thickened or dilated);
- Ophthalmoscopy (to detect narrowing of arteries, dilated veins, retinal hemorrhages);
- Ultrasound of the abdominal cavity (liver, kidneys, gall bladder are examined in detail).
Evaluation of results and correction of the nursing intervention plan:
- In case of a hypertensive crisis - a reduction in the number of complaints, a gradual (every 1-2 hours) reduction in blood pressure to the patient’s usual value;
- During subsequent treatment of arterial hypertension, preventive measures are taken during the rehabilitation period.
Nursing process in hypertension
Content
Introduction…………………………………………………………………………………3
1. Etiology……………………………………………………………………………….4
2. Clinic………………………………………………………………………………….5
3. Diagnostics………………………………………………………………………………..7
4. Treatment………………………………………………………………………………….8
5. Nursing process for hypertension……………………..9
Conclusion……………………………………………………………………………….15
Literature………………………………………………………………………………..16
Introduction
Arterial hypertension is an increase in blood pressure in the arteries as a result of increased heart function or increased peripheral resistance, or a combination of these factors. There are primary (essential) and secondary arterial hypertension.
Hypertension, or essential hypertension, is an increase in blood pressure not associated with organic damage to the organs and systems that regulate it. The development of hypertension is based on a violation of the complex mechanism that regulates blood pressure under physiological conditions.
According to a survey of a representative sample (1993), the age-standardized prevalence of hypertension (>140/90 mm Hg) in Russia is 39.2% among men and 41.1% among women. Women are better informed about the presence of the disease than men (58.9% versus 37.1%), are treated more often (46.7% versus 21.6%), including effectively (17.5% versus 5. 7%). In men and women, there is a clear increase in hypertension with age. Before 40 years of age, hypertension is more often observed in men, after 50 years - in women.
The development of hypertension can be divided into three parts:
central - a violation of the relationship between the processes of excitation and inhibition of the central nervous system;
increased production of pressor substances (norepinephrine, aldosterone, renin, angiotensin) and a decrease in depressor effects;
tonic contraction of arteries with a tendency to spasm and organ ischemia.
Etiology
Hereditary burden is the most proven risk factor and is well identified in relatives of the patient of close kinship (the presence of HD in mothers of patients is of particular importance). We are talking, in particular, about the polymorphism of the ACE gene, as well as the pathology of cell membranes. This factor does not necessarily lead to headache. Apparently, genetic predisposition is realized through the influence of external factors.
People with excess body weight have higher blood pressure. Epidemiological studies have convincingly shown a direct correlation between body weight and blood pressure. With excess body weight, the risk of developing hypertension increases 2-6 times (Quetelet index, which is the ratio of body weight to height, exceeds 25; waist circumference >85 cm in women and >98 cm in men). The factor of excess body weight is associated with a more frequent development of hypertension in industrialized countries.
Metabolic syndrome (syndrome X), characterized by a special type of obesity (android), insulin resistance, hyperinsulinemia, and lipid metabolism disorders (low levels of high-density lipoproteins - HDL - are positively correlated with increased blood pressure).
Alcohol consumption. SBP and DBP in persons who consume alcohol daily are 6.6 and 4.7 mmHg, respectively. higher than in people who drink alcohol only once a week.
Salt consumption. Many experimental, clinical and epidemiological studies have shown a connection between high blood pressure and daily consumption of table salt.
Physical activity. People living a sedentary lifestyle are 20-50% more likely to develop hypertension than physically active people.
Psychosocial stress. It has been established that acute stress load leads to an increase in blood pressure. It is assumed that long-term chronic stress also leads to the development of hypertension. The patient’s personality traits are probably also of great importance.
Clinic
The central symptom of hypertension is an increase in blood pressure, from 140/90 mm Hg. Art. and higher.
Main complaints: headaches, dizziness, blurred vision, pain in the heart, palpitations. Patients may have no complaints. The disease is characterized by an undulating course, when periods of deterioration are replaced by periods of relative well-being.
In the stage of functional disorders (stage I) there are complaints of headaches (usually at the end of the day), sometimes dizziness, and poor sleep. Blood pressure increases inconsistently, usually due to anxiety or fatigue (140-160/905-100 mm Hg).
In the second stage.
Complaints of constant headaches localized in the occipital region. Patients have poor sleep and dizziness. Blood pressure is persistently elevated. Attacks of pain in the heart appear.
In stage 2 hypertension, the ECG shows signs of left ventricular hypertrophy and myocardial malnutrition.
In stage three hypertension, various organs are affected, primarily the brain, heart and kidneys. Blood pressure is persistently elevated (more than 200/110 mm Hg). Complications develop more often.
Hypertensive crisis
- a sudden increase in blood pressure, accompanied by disorders of the autonomic nervous system, increased disorders of the cerebral, coronary, and renal circulation and an increase in blood pressure to individually high numbers.
There are crises of types I and II.
Type I crisis occurs in stage I headache and is accompanied by neurovegetative symptoms.
Type II crisis occurs in stages II and III of headache.
Symptoms of a crisis:
severe headache, transient visual impairment, hearing impairment (stupefaction), heart pain, confusion, nausea, vomiting.
The crisis is complicated by myocardial infarction and stroke. Factors provoking the development of crises: psycho-emotional stress, physical activity, sudden withdrawal of antihypertensive drugs, use of contraceptives, hypoglycemia, menopause, etc.
The benign variant of the development of hypertension is characterized by slow progression, changes in organs are at the stage of stabilization of blood pressure. The treatment is effective. Complications develop only in the later stages. For definitions of risk levels, see the table.
The malignant variant of hypertension is characterized by a rapid course, high blood pressure, especially diastolic, rapid development of renal failure and brain disorders. Changes in the fundus arteries with foci of necrosis around the optic nerve nipple and blindness appear quite early. The malignant form of hypertension can be fatal if left untreated.
Diagnostics
Diagnosis of hypertension and examination of patients with hypertension is carried out in strict sequence, meeting certain objectives:
— determination of the stability of the increase in blood pressure and its degree;
- exclusion of symptomatic hypertension or identification of its form;
— identifying the presence of other risk factors for cardiovascular diseases and clinical conditions that may affect prognosis and treatment, as well as classifying the patient to a particular risk group;
— determination of the presence of lesions of “target organs” and assessment of their severity.
According to the 1999 WHO-ITF international criteria, hypertension is defined as a condition in which blood pressure is 140 mmHg. Art. or higher and/or ADD - 90 mm. rt. Art. or higher in individuals not receiving antihypertensive therapy.
Headache is divided into primary, when headache and associated symptoms form the core of the clinical picture and are combined into an independent nosological form (migraine, tension headache, cluster headache), and secondary, when it becomes a consequence of obvious or masked pathological processes.
Among primary headaches, the most common forms are tension-type headache (TTH) and migraine (M).
In a patient with newly diagnosed hypertension, a careful history must be taken, which should include: - the duration of hypertension and levels of elevated blood pressure in the history, as well as the results of previously used antihypertensive treatment, a history of hypertensive crises.
Additional examination:
OAK—increase in red blood cells, hemoglobin. BAC—hyperlipidemia (due to atherosclerosis). OAM—proteinuria, cylindruria (with chronic renal failure). Zimnitsky test - isohyposthenuria (with chronic renal failure). ECG - signs of left ventricular hypertrophy. Ultrasound of the heart - enlargement of the wall of the left ventricle. Examination of the fundus - narrowing of the arteries, dilatation of the veins, hemorrhages, swelling of the optic nerve nipple.
Treatment
Treatment of stage I headache is usually carried out using non-drug methods, which can be used at any stage of the disease. A hyposodium diet is used, body weight is normalized (fasting diets), limiting alcohol intake, quitting smoking, constant physical activity, acupuncture, rational psychotherapy, acupuncture, physiotherapeutic treatment, herbal medicine.
If there is no effect from non-drug treatment within 6 months, drug treatment is used, which is prescribed in stages (starting with one drug, and if ineffective, a combination of drugs).
In patients with stages I and II, the leading role in treatment belongs to systematic drug therapy, which should be comprehensive. At the same time, it is necessary to systematically carry out preventive measures, among which physical education occupied a significant place.
Long-term antihypertensive therapy with individual maintenance doses is required. In elderly patients, blood pressure decreases gradually, since a rapid decrease worsens cerebral and coronary circulation. Blood pressure should be reduced to 140/90 mmHg. or to values lower than the original ones by 15%. Treatment should not be abruptly stopped; treatment should begin with known medications.
Of the many groups of antihypertensive drugs, 4 groups have received practical use: β-blockers (propranolol, atenolol), diuretics (hypothiazide, indapamide, uregit, veroshpiron, arifon), calcium antagonists (nifedipine, adalat, verapamil, amlodipine) ACE inhibitors (captopril , enalapril, sandopril, etc.).
Nursing process in hypertension
Lifestyle changes are recommended for all patients, including those receiving drug therapy, especially in the presence of certain risk factors. They allow:
lower blood pressure; reduce the need for antihypertensive drugs and maximize their effectiveness; favorably influence other existing risk factors; carry out primary prevention of hypertension and reduce the risk of concomitant cardiovascular disorders at the population level.
Non-drug methods include:
- to give up smoking; — reduction and/or normalization of body weight (achieving a BMI < 25 kg/m2); - reducing the consumption of alcoholic beverages to less than 30 g of alcohol per day in men and less than 20 g per day in women; - increase in physical activity (regular aerobic (dynamic) physical activity for 30-40 minutes at least 4 times a week); — reducing the consumption of table salt to 5 g/day;
- a comprehensive change in diet (increasing the consumption of plant foods, reducing the consumption of saturated fats, increasing the diet of potassium, calcium contained in vegetables, fruits, grains, and magnesium contained in dairy products).
The target blood pressure level is a blood pressure level of less than 140 and 90 mm Hg. In patients with diabetes, it is necessary to reduce blood pressure below 130/85 mm Hg. Art., with chronic renal failure with proteinuria more than 1 g/day below 125/75 mm Hg. Achievement of target blood pressure should be gradual and well tolerated by the patient. The higher the absolute risk, the more important it is to achieve the target blood pressure level. With regard to concomitant hypertension and other associated risk factors, it is also recommended to achieve their effective control, and, if possible, normalize the corresponding indicators (Table 5. Target values of risk factors).
Achieving and maintaining target blood pressure levels requires long-term monitoring with monitoring of compliance with recommendations for lifestyle changes, regularity of antihypertensive therapy and its correction depending on the effectiveness and tolerability of treatment. During dynamic observation, it is crucial to achieve individual contact between the patient and the nurse, and a patient education system that increases the patient’s sensitivity to treatment.
In a hospital setting, the entire rehabilitation process is based on three motor modes: bed: strict, extended; ward (semi-bed); free.
During extended bed rest, the following tasks are solved: improving the neuropsychic status of the patient; gradual increase in the body’s adaptation to physical activity; decreased vascular tone; activation of the function of the cardiovascular system by training intra- and extracardiac circulatory factors.
At the stage of ward (semi-bed) rest, the following tasks are solved: eliminating the patient’s mental depression; improving adaptation of the cardiovascular system to increasing loads through strictly dosed training; improvement of peripheral blood circulation, elimination of congestion; training in proper breathing and mental self-regulation.
During the free regime, the tasks of improving the functional state of the central nervous system and its regulatory mechanisms are solved; increasing the overall tone of the body, the adaptability of the cardiovascular and respiratory systems and the whole body to various physical activities; strengthening the myocardium; improving metabolic processes in the body.
This motor mode in a hospital setting is characterized by the greatest motor activity. The patient is allowed to walk freely around the department; it is recommended to walk up the stairs (within three floors) with pauses for rest and breathing exercises
In hypertensive crisis
Lasix IV, nitroglycerin, clonidine or Corinfar, nifedipine - 1 table are used. under the tongue. If there is no effect - intravenous aminophylline, intravenous labetolol. Parenteral treatment is prescribed by a doctor.
It should be remembered that blood pressure must be reduced slowly, over 1 hour; with a rapid decrease, acute cardiovascular failure can develop, especially in the elderly. Therefore, after 60 years, antihypertensive drugs are administered only intramuscularly.
Treatment of hypertension is carried out for a long time and antihypertensive drugs are discontinued only when blood pressure stabilizes to the desired level over time (the doctor decides to cancel).
Stage I – nursing examination based on objective and subjective complaints
sick
Stage II Stage III Stage IV Stage V
| Patient problems | Goals | Nursing interventions | Evaluating the effectiveness joint venture (produced upon expiration of the delivery period) no purpose | ||
| k/s | d/s | plan | motivation | ||
| Main: - increased blood pressure | Achieve a gradual decrease in blood pressure by the end of the first day | Achieve stabilization of blood pressure indicators by day 10 (at discharge) | 1. Ensure physical and psychological rest 2. Place the patient or transfer him to a horizontal position with the head end raised 3. Provide access to fresh air 4. Place mustard plaster on the area. back of the head and calf muscles 5. Monitor the patient’s condition, measure blood pressure every 30 minutes until blood pressure normalizes 6. Follow all doctor’s orders: monitor regular intake of antihypertensive drugs 7. Train the patient in measuring blood pressure | For the effectiveness of treatment In order to reduce blood flow to the goal. brain and heart For enriched. air with oxygen To reduce blood pressure For timely. providing emergency assistance in case of emergency. complications | By the end of the first day, blood pressure was reduced - the goal was achieved. By the 10th day, blood pressure remained at a stable level - the goal was achieved. |
| - headaches, dizziness, tinnitus | The patient will note a decrease in goals. pain and dizziness by the end of the 3rd day | The patient will not complain about the goal. pain and dizziness - dizziness at the time of discharge | 1. Ensure physical and mental rest 2. Ensure medication intake. Medicines prescribed by a doctor. 3. If dizziness occurs, accompany the patient. 4. Ensure frequent ventilation of the rooms. | By day 3, the patient has no headaches - the goal has been achieved. At the time of discharge, the patient does not complain of headaches - the goal has been achieved. | |
| Comorbidities: sleep disturbance | Within 7 days the patient will be able to fall asleep and sleep without awakening for 4-6 hours, if necessary with the help of sleeping pills | By the time of discharge from the hospital, the patient will be able to sleep from 6 to 7 hours continuously without taking sleeping pills | 1. Observe the patient’s sleep and assess sleep disturbances. 2. Distract the patient from sleep during the day (which promotes night sleep) 3. Ensure that all types of food and drinks containing caffeine are excluded from the patient’s diet, including tea and coffee. 4. Take measures to help the patient fall asleep, e.g.: rubbing the back, warm baths, airing the room before bed, warm non-stimulating drinks (milk), quiet music, relaxation exercises. 5. Set a certain time for going to bed and do not violate this schedule. 6. Assure the patient that if he needs anything, he will get the help he needs. 7. As prescribed by the doctor, give the patient sleeping pills | For the first 5 days the patient slept with the help of sleeping pills, from the 6th day he began to fall asleep without them - the goal was achieved. | |
| - vomit | Reduce the severity of vomiting by the end of 3 days | Vomiting will not bother the patient | 1. Provide the patient with everything necessary (basin, tray) for vomit, towel, mouthwash, if necessary 2. Avoid dehydration (give drink) 3. Create physical and mental peace, eliminate bright light, noise. 4. Give antiemetics as prescribed by the doctor. | On the 2nd day the patient no longer complains of vomiting - the goal has been achieved | |
| - irritability, anxiety | Reduce the patient's irritability and anxiety within 6 days | The patient will not be irritable upon discharge | 1. Create a calm environment. 2. Talk with the patient more often on various topics. 3. Instill confidence in a favorable outcome of the disease 4. Ensure the use of sedatives (such as valerian, motherwort) as prescribed by the doctor 5. Teach the patient relaxation methods. | By day 6, the patient became less irritable, the anxious state does not bother the patient - the goal has been achieved. | |
| Potential - the possibility of developing complications; — ineffectiveness of taking antihypertensive drugs. | Prevent the development of complications and progression of the disease | 1. Conduct conversations: A) about the importance of observing work, rest, diet - with limited salt and liquid. B) about the effect of smoking and drinking alcohol on increasing blood pressure C) about the importance of systematically taking antihypertensive drugs and periodically visiting a doctor. | |||
Conclusion
Hypertension is a chronic disease that affects various systems of the body, characterized by an increase in blood pressure above normal, the most common disease of the cardiovascular system.
It has been established that those suffering from hypertension account for 15 - 20% of the adult population according to various epidemiological studies. HD quite often leads to disability and death. The underlying cause of the disease is arterial hypertension.
Arterial hypertension is one of the main risk factors for the development of coronary artery disease, cerebral stroke and other diseases.
Primary prevention of hypertension is the prevention of etiological risk factors.
Secondary prevention is medical examination of patients with hypertension. Patients are examined and examined at least once a year.
The main goal of treating a patient with hypertension is to achieve the maximum degree of reduction in the overall risk of cardiovascular morbidity and mortality. This involves addressing all identified reversible risk factors, such as smoking, high cholesterol and diabetes, appropriate treatment of associated diseases, as well as correction of high blood pressure itself.
The target blood pressure level is a blood pressure level of less than 140 and 90 mm Hg. In patients with diabetes, it is necessary to reduce blood pressure below 130/85 mm Hg. Art., with chronic renal failure with proteinuria more than 1 g/day below 125/75 mm Hg. Achievement of target blood pressure should be gradual and well tolerated by the patient.
Literature
1. Gogin E.E. “Hypertension” - M, 1997 – 62 p.
2. Roytberg G. E. Strutynsky A. V. Internal diseases. Cardiovascular system, M, 2002 – 123 p.
3. Smoleva E.V. Nursing in therapy. – Rostov n/a: Phoenix, 2007 – 169 p.
4. Tulyankin V.F. Tulyankina T.I. Home Doctor. JSC "Paritet", 2002-248p.
Working with the patient's family
The role of nursing care in the prevention and prevention of complications from a hypertensive crisis is extremely important. If the health worker does not explain to the patient and his family that the degree of danger of all the consequences of an attack will depend on regular monitoring of blood pressure, adherence to diet and regimen, then they themselves are unlikely to come to such a conclusion and will comply with all preventive measures.
Relatives and the patient must understand that treatment of hypertension is a long process. The nurse tells them about all the features and possible consequences of the disease, teaches them the rules of caring for a patient after a hypertensive crisis.
Hypertensive patients have an active role to play in strengthening their own health, and the health worker must tactfully but persistently support the patient in his desire to change his life. This is especially important for mature patients who find it difficult to change long-established habits.
Hypertension: risk factors, treatment and prevention methods
Gilmanshina Diana Ralifovna
Cardiologist, general practitioner
Hypertension
is a pathology of the cardiovascular system, developing as a result of dysfunction of higher centers of vascular regulation, neurohumoral and renal mechanisms and leading to arterial hypertension, functional and organic changes in the heart, central nervous system and kidneys.
Arterial hypertension (AH)
– stable increase in systolic pressure more than 140 mmHg. Art. or diastolic more than 90 mm Hg. Art.
According to research, arterial hypertension is one of the most common chronic diseases. Hypertension is the most common chronic disease in the practice of general practitioners and cardiologists.
Arterial hypertension occurs in approximately one third of the population of most developed and developing countries. According to recent epidemiological studies in Russia, about 48% of men and 40% of women have arterial hypertension.
Risk factors for hypertension.
They can be conditionally divided into irremovable and removable.
Unavoidable risk factors for hypertension:
• Age (the incidence of the disease is more common after 45 years).
• Gender (men are more susceptible to hypertension).
• Genetic predisposition, heredity (if one of the parents had the disease, the probability is 50–60%, if both parents were sick, the probability is almost 100%).
Avoidable risk factors:
• Overweight and obesity (if the waist circumference in men is 102 cm or more, and in women – 88 cm or more). It is known that for every 10 kg of excess weight, systolic (upper) blood pressure increases by 2-3 mmHg, and diastolic (lower) - by 1-3 mmHg.
• Smoking.
• Nutritional factors.
• Poor nutrition (excessive consumption of table salt, overeating, excessive consumption of animal fats, lack of dairy products, vegetables and fruits).
• Abuse of alcohol and coffee.
• Chronic stress.
• Physical inactivity – sedentary lifestyle (risk increases by 20 – 50%).
• Presence of concomitant diseases (diabetes mellitus, kidney pathology and atherosclerosis).
You need to know that arterial hypertension ranks first in its contribution to mortality from cardiovascular diseases (CVD). Most often, patients die from its complications. The relationship between blood pressure (BP) and CVD risk is continuous, constant and independent of other risk factors.
With a long-term or malignant course of hypertension, chronic damage to the blood vessels of target organs develops: the brain, kidneys, heart, eyes.
Instability of blood circulation in these organs against the background of persistently elevated blood pressure can cause the development of:
• angina pectoris, • myocardial infarction, • hemorrhagic or ischemic stroke, • cardiac asthma, pulmonary edema, • dissecting aortic aneurysm, • retinal detachment, etc.
The development of acute emergency conditions against the background of hypertension requires a decrease in blood pressure in the first minutes and hours, as it can lead to the death of the patient.
The course of hypertension is often complicated by hypertensive crises - periodic short-term increases in blood pressure. The development of crises may be preceded by emotional or physical overstrain, stress, changes in meteorological conditions, etc. In a hypertensive crisis, there is a sudden rise in blood pressure, which can last several hours or days and is accompanied by dizziness, severe headaches, a feeling of heat, increased heartbeat, vomiting, cardialgia (pain in the heart area), visual impairment. During a hypertensive crisis, patients are frightened, excited or inhibited, and drowsy; in severe cases they may lose consciousness.
Against the background of a hypertensive crisis and existing organic changes in blood vessels, myocardial infarction, acute cerebrovascular accidents, and acute left ventricular failure can often occur.
Hypertension is classified according to a number of characteristics:
reasons for the rise in blood pressure, damage to target organs (brain, blood vessels, heart, kidneys), by blood pressure level, by course, etc.
According to the etiological principle, they distinguish:
- essential (primary) - secondary (symptomatic, i.e. against the background of other diseases) arterial hypertension
Depending on the level there are:
• Optimal blood pressure is < 120/80 mm Hg. Art. • Normal blood pressure - 120-129 /84 mm Hg. Art. • Borderline normal blood pressure - 130-139/85-89 mm Hg. Art. • Arterial hypertension of the 1st degree - 140-159/90-99 mm Hg. Art. • Arterial hypertension II degree - 160-179/100-109 mm Hg. Art. • Stage III arterial hypertension - more than 180/110 mm Hg. Art.
Treatment.
When treating hypertension, it is important not only to lower blood pressure, but also to correct and reduce the risk of complications as much as possible. It is impossible to completely cure hypertension, but it is quite possible to stop its development and reduce the frequency of crises.
Hypertension requires the combined efforts of the patient and the doctor to achieve a common goal.
At any stage of hypertension it is necessary:
• Follow a diet with increased consumption of potassium and magnesium, limiting the consumption of table salt;
• Stop or sharply limit alcohol intake and smoking;
• Get rid of excess weight;
• Increase physical activity: it is useful to engage in swimming, physical therapy, and walking;
• Take prescribed medications systematically and for a long time under the control of blood pressure and dynamic supervision of a cardiologist.
The criteria for the effectiveness of treatment of hypertension is the achievement of:
•
short-term goals:
maximum reduction in blood pressure to a level of good tolerance;
• medium-term goals:
preventing the development or progression of changes in target organs;
• long term goals:
prevention of cardiovascular and other complications and prolongation of the patient’s life.
Cardiologist, Candidate of Medical Sciences Diana Ralifovna Gilmanshina.