What is the oncological marker CEA?
CEA is a protein substance that, under normal conditions, is produced in the embryo during development in the organs of the digestive tract.
It stimulates the division of new cells. In adults, this substance is also present, but its purpose has not been determined to this day. If the amount changes, this is a signal for the possible development of oncology or another pathology or inflammatory process. Therefore, such an indicator as the CEA tumor marker has appeared, which helps determine the risk and presence of cancer in a person. It is measured in nanograms per milliliter of blood (ng/ml).
What are the norms for men and women
To date, the following limits have been defined that are considered normal:
| Men | smokers – from 0.52 ng/ml to 6.3 ng/ml; non-smokers – from 0.37 ng/ml to 3.6 ng/ml. |
| CEA tumor marker is normal in women | smokers – from 0.42 ng/ml to 4.8 ng/ml; non-smokers – from 0.21 ng/ml to 2.5 ng/ml. |
For benign formations, depending on their location, the following standards are defined:
| Pulmonary pathologies | 1.4-5.6 ng/ml |
| Kidney diseases | 0.75-3.00 ng/ml |
| Hepatitis | 0.95-3.8 ng/ml |
| Thyroid diseases | 0.55-2.2 ng/ml |
| Other non-oncological entities | 0.95-3.8 ng/ml |
Now let's see what the CEA tumor marker shows if a malignant process develops:
| Bladder tumor | 0.75-3.00 ng/ml |
| Breast oncology | 2.05-8.2 ng/ml |
| Colorectal tumor | 2.55-10.2 ng/ml |
| Esophageal carcinoma | 2.25-9.00 ng/ml |
| Lung oncology | 2.4-9.6 ng/ml |
| Ovarian cancer | 0.65-2.6 ng/ml |
| Tumor in the kidneys | 0.5-2.00 ng/ml |
| Pancreas cancer | 9.7-38.4 ng/ml |
| Stomach oncology | 28.25-113 ng/ml |
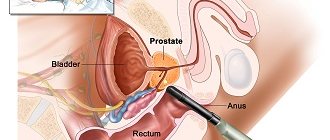
| Prostate cancer | 0.6-2.4 ng/ml |
| Tumor in the rectum | 0.7-2.8 ng/ml |
| Other cancers | 1-4 ng/ml |
Important! In the presence of a malignant tumor, the CEA tumor marker always shows growth, as in the case if treatment does not produce results.
At the same time, a negative and normal result does not guarantee the absence of cancer. Therefore, additional studies are often prescribed, in particular in patients with a hereditary predisposition, frequent inflammatory diseases, and a weak immune system.
Let us remind you that independent interpretation of the results is undesirable, since this requires special knowledge that the oncologist has.
It is enough to know the limits of the norms and carry out the analysis in several clinics at once, at least because the equipment in each of them is different, which can give different results. Of course, the qualifications of the doctor and his ability to work with equipment and read test results are important. Consult an Israeli specialist
High CEA tumor marker
In fact, there are many reasons for the increase in the production of this protein compound. Moreover, they are the same for men and women. We have highlighted the main ones, which are the most popular and occur more often than others:
- Smoking. It is known that the CEA tumor marker in a smoker always reveals a significant increase in pathological protein in the blood.
- Inflammatory process in any human organ and system.
- Pulmonary tuberculosis.
- Cirrhosis of the liver.
- Nodular enlargement of the liver.
- Hemangioma.
- Cystic fibrosis.
- Crohn's syndrome and many others.
- Development of benign formations (polyps, fibromas, lipomas, neuromas and others).
- Oncology and metastases.
If the cause of the increase is not cancer, the CEA tumor marker will show an increase in the range of 5-10 ng/ml without subsequent changes in level in the absence of treatment. If this figure is higher, depending on the organ/system being examined, additional examination may be required to identify the location and stage of tumor development.
When is it necessary to see a doctor?
An increase in the indicator to a level of 10 μg/l or higher is a reason to immediately undergo examination
. Decoding the CEA tumor marker is a really important procedure; with its help, it is possible to obtain many times more information than from a banal oncology test.
Typically, with such high concentrations of CEA, women begin to experience other symptoms. The most common occurrences are:
- causeless cough, frequent shortness of breath;
- general fatigue and lethargy, even with moderate exercise;
- a swelling protruding on the body that is easily palpable;
- body temperature rises, active sweating is observed;
- appetite decreases or is completely absent;
- weight loss unreasonably;
- disruptions in the functioning of the gastrointestinal tract occur;
- moles appear;
- wounds heal poorly, causeless bleeding may occur;
- aching pain in certain parts of the body.
If you notice such symptoms, it is important not to panic and consult a doctor as soon as possible, while realizing that cancer in the early stages is curable.
CEA tumor marker analysis
A test to determine the amount of this protein compound is most informative in the presence of a malignant tumor in the rectum and colon. Here it accurately shows the true picture and does not require additional analysis.
In combination with other studies, the CEA tumor marker is carried out to determine the cancer process in:
- Mammary glands.
- Lungs.
- Stomach.
- Ovaries.
- Prostate gland.
Attention! In the presence of metastases in bone tissue and liver, the level of cancer antigen may increase.
It is mandatory to be prescribed after surgical treatment of a malignant tumor in order to determine its effectiveness. If everything is in order, then after two months the amount is restored to the normal level, as shown by the CEA tumor marker.
Detailed description of the study
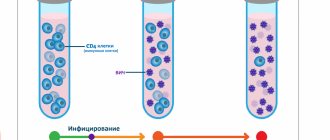
Carcinoembryonic antigen (CEA) is a protein present in certain tissues of the developing fetus. By the time a child is born, its production is significantly reduced. CEA does not penetrate the placental barrier, so its content in the mother’s blood does not increase during pregnancy.
In adults, CEA is normally present in the blood in very low quantities. Men have, on average, slightly higher levels of this substance than women. Its production in the body increases sharply during certain oncological processes and inflammation.
CEA is not an antigen in relation to tissues and cells in the human body, but it has the ability to combine with antibodies during immunochemical analysis, that is, it exhibits antigenic properties.
These features of REA determine the name of this analysis. It is used as one of the tumor markers to detect cancer.
Assessment of the content of CEA in human blood is more often used for colorectal cancer, that is, damage to the colon and rectum, since for diseases of this localization it has a fairly high sensitivity.
This study is of greatest diagnostic value for people with already confirmed cancer and is used to assess the response to treatment and achieve remission.
In case of successful chemotherapy or surgery, CEA levels decrease within several months. Their repeated increase may indicate a relapse of the disease.
An isolated increase in CEA serves as an auxiliary tumor marker for malignant tumors of many locations. However, an increase in CEA in the absence of clinical and laboratory-instrumental data on the presence of cancer does not necessarily mean that any organ is affected by cancer.
An increase in CEA production is observed with inflammation of the gastrointestinal tract and mammary gland. Long-term smoking doubles its concentration. Metabolism of this tumor marker is carried out in the liver, therefore, when it is damaged, CEA indicators are increased even in the absence of an oncological process.
CEA tumor marker transcript
It is carried out in a hospital using the immunochemiluminescence blood test (ELISA) method in a laboratory setting.
To do this, blood is taken from a vein from the patient using a syringe. This test takes time as the sample first goes through a centrifuge and is then analyzed by a laboratory technician. Since in most public medical institutions the panel is designed for 40 people, the reaction is not immediately given. And only after collecting the required number of samples is the research process completed and the reaction performed.
Since there are often cases when the patient cannot or does not want to wait, a rapid analysis is performed. But in this case, the result will be uninformative and will not be enough to make a diagnosis. Even if we are talking about examinations of the large and small intestines. Therefore, when choosing a quick method, you should prepare to undergo additional diagnostics and laboratory tests.
Before the test, patients need to prepare:
- 8 hours before the start of the examination, do not eat (only still water is allowed).
- For half an hour, avoid being exposed to stress and physical overexertion, so you need to take care to exclude all kinds of irritants (you can listen to music, for example).
- The day before the procedure, stop smoking and other bad habits.
In general, the preparation is similar to that required before a blood test for biochemistry. Please note that only blood from a vein is used for analysis.
It is very important to comply with these requirements, since this determines what level the CEA tumor marker will show.
The reference values at this moment are determined by the following figures: for smokers - no more than 3.8 ng/ml, for those who have a nicotine addiction, this figure is no more than 5.5 ng/ml. As these indicators increase, the risk of the onset of a malignant process increases.
As a rule, in the presence of oncology, decoding of the CEA tumor marker demonstrates its growth within 6-8 months. This indicates the need to begin immediate treatment.
What other studies are needed to determine oncology?
If the decoding of the CEA tumor marker is uninformative, additional studies are prescribed for other tumor markers, a general analysis of urine and blood, tests for beta-3-microglobulins in the urine and blood, and various cancer antigens. Also, for accurate diagnosis, magnetic resonance imaging is recommended, which will show the presence of pathological cells not only in organs, but also in fluids and body systems.
Please note that the normal CEA tumor marker is the same for men and women. A slight difference can only be detected in the case of bad habits and the degree of their severity (chronic smoking with experience, alcohol, drugs).
Preparing for the test
Proper preparation for any analysis reduces the risk of false results and increases the accuracy of the study. The biomaterial for the criterion under consideration is blood serum, which is collected in special vacuum sterile disposable tubes from the patient’s cubital vein. Recommendations for preparation:
- 1 day before, exclude fatty, smoked and fried foods from the diet, and at least 8 hours before donating blood, do not eat food. This rule is explained by the fact that during the digestion of food, the production of enzymes in the human body is activated, some of which are similar in chemical structure to tumor markers. Neglecting the recommendation will lead to the risk of obtaining false positive results;
- in the evening before collecting biomaterial, you are allowed to drink clean, non-sweetened water without carbon, and in the morning - 1-2 glasses of water. This will reduce the risk of hemolysis and the formation of blood clots in vitro;
- half an hour before the procedure, it is necessary to exclude physical and emotional stress, which leads to changes in the functioning of the hormonal and endocrine systems and, as a result, unreliable results. 15 minutes before donating blood, calm down and sit in the laboratory in a comfortable position;
- It is necessary to limit the intake of any medications in consultation with your doctor for at least 1 day. If it is impossible to cancel life-saving medications, it is important to notify laboratory staff about their use. In this case, when selecting reference values, not only gender, age, alcohol and smoking abuse, but also medication use will be taken into account.
The duration of research in private clinics is 1 day, not counting the day of taking the biomaterial, and the price starts from 550 rubles.