What is a blood sterility test?
If the blood is prescribed for sterility, the doctor will help you figure out what it is. He must explain to his patient about the diagnostic plan and the need for each study.
When the body is infected, bacteria can enter the bloodstream and move freely throughout the body, infecting organs and tissues. In the blood, pathogenic microflora appears when the integrity of the skin, tissues and blood vessels is damaged. This occurs with injuries: cuts, burns, scratches, bites, open fractures, etc.
A common cause of blood poisoning is surgery and some cosmetic procedures.
Any bacterium, under certain favorable conditions, begins to actively multiply and form a colony. Taking advantage of this feature of microorganisms, scientists use a Petri dish with a nutrient medium in which colonies of bacteria grow from a blood solution.
This allows you to study their type, characteristics and determine the method of treating the patient. If there are no bacteria, a colony does not form, the blood is considered sterile.
References
- Clinical guidelines for the diagnosis and treatment of brain abscesses, intracranial epidural and subdural empyemas. Association of Neurosurgeons of Russia, 2015. - 28 p.
- Kupchenko, A.M., Kosinets, V.A. Identification and determination of antibacterial sensitivity of anaerobic microflora in the treatment of widespread purulent peritonitis. Surgery news, 2014. - No. 4. - pp. 457-462.
- Guilhot, E., Khelaifia, S., Scola, B. et al. Methods for culturing anaerobes from human specimen. Future microbiology, 2021. - Vol. 13. - P. 369-381.
In what cases is it prescribed
A blood sterility test helps to find out about the presence and characteristics of bacteria in the body. This is a procedure that is carried out not only for diagnosis, but also in preparation for certain medical procedures.
In what cases is a blood test for sterility prescribed:
- For diseases associated with immunodeficiency of the body, for example, HIV. In this case, the patient should know - blood testing for sterility: what is a periodic examination that will help timely diagnose a disease that the body cannot cope with on its own.
- In the absence of effect from antibiotic treatment. Using a sterility test, it is possible to find out about the sensitivity of bacteria to a particular antibiotic and select the right medicine. Diagnostics, as a rule, is repeated after taking a course of the drug.
- Before and after surgical interventions. Any operation carries a risk of blood poisoning. This is especially dangerous if there are already pathogens in the blood. After surgery, determining sterility helps determine the absence or presence of bacteria in the body and, if necessary, determine a treatment strategy.
- After accidents or serious injuries. It is imperative that blood be tested for sterility in case of extensive wounds or multiple open fractures. This allows you to determine the number and types of bacteria, as well as fungi, that can enter the blood and lead to infection.
- For rupture of abscesses, perforation of purulent formations, necrosis and peritonitis. In these cases, a large amount of pus with bacteria and fungi enters the body cavity and blood.
- After complex abortions and other obstetric procedures, during which infection with staphylococcus is possible.
- For purulent diseases of the ENT organs: tonsillitis, sinusitis and otitis.
- For oncological diseases. In this case, a sterility test is carried out after laser or chemical therapy. These treatments reduce immune defenses to 0.
- For severe fever that lasts more than 3 days.
What diseases can be detected
Using a blood sterility test, the following diseases can be diagnosed:
- Sepsis. This is a general infection of the body in which a huge number of bacteria or fungi enter the blood. The danger of the disease is that the infection spreads through the blood to all organs and leads to rapid death without treatment.
- Meningitis. Infectious lesions of the membranes of the spinal cord and brain. One of the ways of infection with the bacterial form of meningitis is hematogenous. The blood carries the infection from the inflammatory focus in the tissues or organs to the brain.
- Pyoderma. A severe skin infection caused by coccus bacteria. Infection can occur due to a small scratch, after which the pathogens spread through the blood to other parts of the body.
- Endocarditis. An inflammatory focus in the inner lining of the heart. The main causative agent is streptococci. Appears in the presence of a primary infectious disease.
- Osteomyelitis. An infectious disease of the bones and bone marrow, which is accompanied by necrosis and purulent discharge. The pathogen enters the bone through the blood from the infectious focus. Less commonly, bacterial infection occurs through an open wound when it is contaminated.
- Tuberculosis. A disease of the respiratory system (less commonly of other systems), which occurs due to infection with Koch bacilli. When inoculating for sterility, it is possible not only to determine the presence of the pathogen, but also its resistance to drugs.
How to prepare for analysis
The result of the study largely depends on preparation for analysis. Preparation methods differ from how the study is carried out: routinely or urgently. Routine blood sampling for sterility is carried out in diseases associated with immunodeficiency, in the diagnosis of purulent skin diseases and tuberculosis. Preparation for the study usually begins several days in advance.
At this time, the following rules must be followed:
- Depending on the form of treatment for the disease, antibiotics or other anti-infection drugs must be taken 2-5 days before blood sampling. If medications are not taken, treatment cannot be started, including homeopathic medications.
- For two days, you must stop eating fatty, fried and spicy foods, and completely eliminate alcohol from your diet.
- On the day of the test, smoking and taking any medications are prohibited.
- Some doctors recommend increasing your fluid and food intake on the day of blood donation.
If blood sampling occurs as an emergency, in case of fever, suspected sepsis, after a severe injury or accident, the following rules must be followed:
- The patient’s blood must be taken during the period of peak body temperature – 39-40 degrees. Drugs that reduce fever can be given only after analysis.
- If the patient is taking antimicrobial medications, they should be stopped at least 12 hours before the test.
- In case of open injuries and accidents, blood is first taken to ensure sterility, and only then broad-spectrum antibiotics are administered.
Everything for work: SOP The procedure for taking blood from a patient from a vein by a procedural nurse
1 area of use
This standard operating procedure (hereinafter referred to as SOP) determines the procedure for the nurse to perform when drawing blood from a vein and transporting the resulting samples to the laboratory from the facility's treatment room.
This SOP is intended for the procedural nurse. Monitoring of compliance with the SOP rules by the procedural nurse is carried out by the senior nurses of each department. Work verification according to SOP rules is carried out once a month.
2. Normative references
1. SanPiN 2.1.3.2630-10 “Sanitary and epidemiological requirements for organizations engaged in medical activities.” 2. GOST R 53079.4-2008 “Medical laboratory technologies. Ensuring the quality of clinical laboratory tests. Part 4. Rules for conducting the preanalytical stage." Entered into force on 01/01/2010. 3. ISO 15189:2015 “Medical laboratories. Requirements for quality and competence." 4. Methodological recommendations “Organization of the preanalytical stage when centralizing laboratory research”, adopted at the XVI forum “National Days of Laboratory Medicine of Russia - 2012”, Kishkun A.A., Gilmanov A.Zh. et al.
3. Terms and definitions, abbreviations used SOP
– standard operating procedure.
Vacuum blood collection system
– a set of materials necessary for drawing blood from a vein (vacuum tube, needle, needle adapter).
Primary sample,
specimen - a discrete portion of biological fluid, exhaled air, hair or tissue, taken for research, study or analysis of one or more quantities or properties that are supposed to be attributed to the whole.
4. The procedure for taking blood from a vein
4.1. Inviting a patient to the office
4.1.1.
The procedural nurse invites the patient to enter the office. 4.1.2. The procedural nurse takes a referral form from the patient or person accompanying him. 4.1.3. The procedural nurse asks the patient to sit down on a chair and clear the venipuncture site of clothing. 4.2.
Registration of the referral form in the patient’s appointment sheet 4.2.1. The procedural nurse informs the patient about the progress of the procedure for taking blood from a vein and asks about the correct preparation of the patient for the study, and also explains to the patient all the additional actions necessary for the correct performance of laboratory tests by the attending physician. The procedural nurse’s questions to the patient about the correctness of his preparation for blood donation and the procedural nurse’s explanation of additional information to the patient are given in Appendix A. 4.2.2. Before starting her work in the office, the procedural nurse takes a patient intake sheet, which indicates the patient’s full name and age, card number, time of patient admission, name of the insurance company, diagnosis code with attributes (the procedural nurse in this paragraph indicates the doctor’s specialty who ordered the study). The patient intake form is presented in Appendix B.
4.3. Selection of vacuum tubes
4.3.1. According to the instructions of the attending physician, noted in the referral form, the treatment nurse selects the appropriate type of tubes. Appendix B lists the names of the studies and the corresponding tube types. For biochemical and immunological studies, blood is taken into a biochemical test tube with or without a coagulation activator, for hematological studies - into a test tube with the anticoagulant K2(3)EDTA, for coagulological studies - into a test tube with the anticoagulant sodium citrate. Blood is taken into a separate tube for the following studies: – glycated hemoglobin (in a tube with anticoagulant K2(3)EDTA 2 ml); – blood groups – full name and full name are indicated on the test tube (in a test tube with a coagulation activator); – for ELISA studies (in a test tube with a separation gel).
4.4. Blood collection
4.4.1. The procedural nurse puts on gloves. 4.4.2. He takes the needle and removes the protective cap from the rubberized end, inserts the needle into the holder with the rubberized end and screws it in as shown in the figure. 4.4.3. Places a tourniquet on the patient’s arm 7–10 cm above the venipuncture. Treats the venipuncture field with a skin antiseptic. Removes the protective cap from the outer needle and inserts it into the vein. The holder should touch the forearm and be positioned as parallel to it as possible. 4.4.4. Once the needle is in the vein, the procedure nurse inserts the vacuum tube from its lid into the holder and presses on the bottom of the tube so that the inner needle pierces its rubber stopper, as shown in the figure. 4.4.5. Immediately after blood begins to flow into the test tube, the tourniquet must be removed. Blood flows into the test tube until the vacuum in the test tube is compensated. When drawing blood, do not allow the inner needle to come into contact with the contents of the tube! 4.4.6. After the blood flow stops, disconnect the test tube from the needle and remove it from the holder, resting your thumb on its rim. 4.4.7. The procedural nurse carefully mixes the contents of the tube, inverting it five to six times to completely mix the blood with the anticoagulant, if any, in the tube. 4.4.8. If necessary, the next tube can be inserted into the holder. Immediately after drawing blood, the procedure nurse removes the needle and its holder from the vein, places it in a container intended for disposal, and applies an aseptic bandage to the site of blood collection. 4.4.9. It is necessary to draw blood in the following sequence of tubes (Appendix D): 1) tubes for biochemical and immunological studies with or without a coagulation activator, for ELISA studies with a separation gel; 2) test tubes for studying hemostasis with the anticoagulant sodium citrate; 3) tubes for clinical and PCR studies with anticoagulant K2(3)EDTA. 4.4.10. The procedure nurse places blood samples in racks. 4.4.11. Removes gloves and discards them into a container with a yellow bag intended for the collection of Class B waste.
4.5. Transporting samples from the treatment room
4.5.1. The procedural nurse places specimen racks in a container, places the directions in a folder labeled “For Directions,” and delivers them to the laboratory every 30 minutes, regardless of the number of tubes collected.
Appendix A
Questions from the procedural nurse to the patient about the correctness of his preparation for blood donation and explanation by the procedural nurse of additional information about the patient’s further actions
Questions from the procedural nurse to the patient about the correctness of his preparation for blood donation:
1. Does the patient donate blood on an empty stomach? 2. If a patient donates blood to study platelet aggregation, then it is necessary to clarify when was the last time he was sick? 3. Is the patient taking any medications? 4. Were instrumental examinations performed on the patient the day before (a week before blood collection)?
Additional information provided by the treatment nurse to the patient:
1. When taking a glucose tolerance test, explains how and where to dilute the glucose powder and indicates the time for repeated blood sampling. 2. When applying an aseptic dressing, reminds that the dressing should be removed after 10–15 minutes.
Appendix B
Selection of vacuum systems depending on the assigned test
| Test name | Type of study | Used anticoagulant in vitro |
| Total protein | Serum | Clotting activator |
| Albumen | Serum | Clotting activator |
| Protein fractions | Serum | Clotting activator |
| Serum glucose | Serum | Clotting activator |
| Glucose 1 hour after eating | Serum | Clotting activator |
| Glucose 2 hours after eating | Serum | Clotting activator |
| Urea | Serum | Clotting activator |
| Serum creatinine | Serum | Clotting activator |
| Uric acid | Serum | Clotting activator |
| Total cholesterol | Serum | Clotting activator |
| Triglycerides | Serum | Clotting activator |
| High density lipoproteins (HDL) | Serum | Clotting activator |
| Low-density lipoproteins (LDL) | Serum | Clotting activator |
| Total bilirubin | Serum | Clotting activator |
| Direct bilirubin | Serum | Clotting activator |
| Amylase | Serum | Clotting activator |
| Pancreatic amylase | Serum | Clotting activator |
| Alanine aminotransferase (ALT) | Serum | Clotting activator |
| Aspartate aminotransferase (AST) | Serum | Clotting activator |
| Gamma glutamyl transferase (GGT) | Serum | Clotting activator |
| Alkaline phosphatase | Serum | Clotting activator |
| Total creatine phosphokinase (CPK) | Serum | Clotting activator |
| K, Na, Cl | Serum | Clotting activator |
| Magnesium | Serum | Clotting activator |
| Total calcium | Serum | Clotting activator |
| Phosphorus, inorganic | Serum | Clotting activator |
| Iron | Serum | Clotting activator |
| General iron-binding | Serum | Clotting activator |
| Ability (OJSS) | Serum | Clotting activator |
| Saturation factor | Serum | Clotting activator |
| C-reactive protein (CRP) | Serum | Clotting activator |
| Rheumatoid factor (Rf) | Serum | Clotting activator |
| Antistreptolysin "O" (ASL "O") | Serum | Clotting activator |
| PSA total | Serum | Clotting activator + gel |
| PSA free | Serum | Clotting activator + gel |
| SA-19-9 | Serum | Clotting activator + gel |
| SA-15-3 | Serum | Clotting activator + gel |
| SA-125 | Serum | Clotting activator + gel |
| Triiodothyronine (T3) | Serum | Clotting activator + gel |
| Thyroxine (T4) | Serum | Clotting activator + gel |
| Free triiodothyronine (FT3) | Serum | Clotting activator + gel |
| Free thyroxine (FT4) | Serum | Clotting activator + gel |
| Thyroid-stimulating hormone (TSH) | Serum | Clotting activator + gel |
| Antibodies to thyroglobulin (AT to TG) | Serum | Clotting activator + gel |
| Antibodies to thyroid peroxidase (Ab to TPO) | Serum | Clotting activator + gel |
| Thyroglobulin | Serum | Clotting activator + gel |
| Prolactin | Serum | Clotting activator + gel |
| Luteinizing hormone (LH) | Serum | Clotting activator + gel |
| Follicle stimulating hormone (FSH) | Serum | Clotting activator + gel |
| Testosterone | Serum | Clotting activator + gel |
| Estradiol | Serum | Clotting activator + gel |
| Progesterone | Serum | Clotting activator + gel |
| HBs Ag (hepatitis B) | Serum | Clotting activator + gel |
| HCV (hepatitis C) | Serum | Clotting activator + gel |
| Anti-HBcor Ag | Serum | Clotting activator + gel |
| Anti-HIV 1.2 | Serum | Clotting activator + gel |
| AT to measles virus IgM | Serum | Clotting activator + gel |
| AT to measles virus IgG | Serum | Clotting activator + gel |
| % Prothrombin according to Quick INR | Plasma | Sodium citrate 3.9% |
| APTT | Plasma | Sodium citrate 3.9% |
| Fibrinogen according to Clauss | Plasma | Sodium citrate 3.9% |
| Thrombin time | Plasma | Sodium citrate 3.9% |
| Protein S | Plasma | Sodium citrate 3.9% |
| Factor VIII | Plasma | Sodium citrate 3.9% |
| Factor IX | Plasma | Sodium citrate 3.9% |
| Glycosylated hemoglobin | Plasma | K2EDTA |
| General blood analysis | Plasma | K2EDTA |
| Reticulocytes | Plasma | K2EDTA |
| Blood type and Rh factor | Plasma | K2EDTA |
Rules for blood sampling
The result of the study directly depends on the correctness of the blood test for sterility.
What is a sterility test and how to draw blood correctly.
Blood sampling is carried out in the following stages:
- The test is taken by a nurse who should tell you about the method of collecting blood.
- Most often, a vein in the elbow or on the back of the hand is used to collect blood. In rare cases, the material is taken from the fingers.
- For manipulation, the medical worker uses only sterile instruments. The gloves and syringe must be new and discarded immediately after analysis.
- Before inserting the needle, the skin is thoroughly treated with a disinfectant solution in a 5 by 5 cm square at the injection site.
- The blood volume must be at least 10 ml. The less material there is, the higher the risk of a false negative or false positive result.
- A catheter should not be used when drawing blood. It is a source of infection and can contaminate the material.
- To ensure accurate results, blood is taken from both hands at intervals of half an hour.
- The nurse removes the needle from the syringe over the flame of the burner, and injects the contents into a test tube with a liquid nutrient medium. The edges of the tube are burned and closed with a sterile rubber stopper.
- The test tube is placed in a thermostat with a temperature favorable for the life of bacteria (38-39 degrees) and moved to the laboratory.
In some cases, a small dose of adrenaline may be administered to the patient half an hour before blood sampling. This causes the spleen to contract and speed up blood flow. Used for infection of internal organs.
Features and advantages of vacutainers
The three-component system for venous blood collection consists of:
- sterile vacuum tube with preservative;
- double-sided automatic needle for intravenous injection;
- automatic needle holder.
The advantages of negative pressure systems are related to their design features:
- safety, sterility and guarantee of sample integrity;
- minimizing microclots and hemolysis;
- maintaining a constant time between collection and connection with the additive;
- exact ratio of sample and additive;
- minimizing the tourniquet effect.
Carrying out the procedure in newborns
Some newborns require blood testing for sterility. Every expectant mother should know what this is and not be afraid if the doctor carries out additional diagnostic procedures immediately after the birth of the baby.
A blood test for sterility may be necessary in the following cases:
- immediately after birth, the child’s temperature rises above 39, there are no reflexes, he constantly spits up, etc.;
- the birth was premature;
- during pregnancy, the expectant mother suffered serious illnesses caused by staphylococci or streptococci;
- there is a risk of intrauterine infection;
- the child has developmental anomalies of internal organs;
- if ompholitis of newborns is suspected - purulent inflammation of the umbilical wound.
The peculiarity of the analysis for a child lies in the method of blood sampling. A child's fingers are too small to grasp enough material. Therefore, to conduct a blood test for sterility, venous blood or capillary blood from the heel is used.
The veins of the child in the elbow, where the sampling procedure is carried out in adults, are quite small and difficult to feel.
Vessels from other parts of the body can be used:
- Veins of the head.
- Veins of the back of the hand.
- Veins of the forearm.
- Calf veins
There are rules for analysis that parents should know:
- the child must be calm, not cry or hysterical. Therefore, it is better to take a rattle or musical toy with you for analysis;
- on the day of blood sampling, it is recommended to give the child a little more fluid than usual when feeding;
- The baby's skin and limbs should be warm before the test. Therefore, you cannot go to the laboratory immediately after leaving the street. The child needs to be woken up, undressed and sat with him in the room for 10-15 minutes;
- It is not recommended to take blood samples from a sleeping or drowsy baby; this can frighten him greatly.
Indications for use
The main purpose of the analysis is to identify the presence of harmful microorganisms that provoke the inflammatory process.
The diagnostician may prescribe the patient to donate blood for microbiological testing in the following cases:
- if the patient suffers from specific symptoms, but doctors for a long time cannot determine what is the primary source of the pathological process;
- the physician assumes the presence of a septic infection in the patient;
- the presence of complications caused by improper surgical intervention;
- placing a catheter in internal organs for a long time;
- a person periodically suffers from high body temperature, but doctors cannot determine what causes such a reaction in the body;
- the presence in the body of an implant that is in direct contact with the biological media of the body.
The absolute indication for testing behavior is the presence of artificial myocardial valves. To obtain a reliable analysis result, you will have to wait at least 10 days, since the germination of pathogenic microorganisms will take several days.
Experts warn that the speed of this process depends on the type of pathogen . It is worth noting that after collecting biomaterial, many patients are prescribed antibiotics (based on the presenting symptoms), but choosing a more competent and optimal treatment regimen is possible only after receiving hemotest data.
Bacteriological culture process
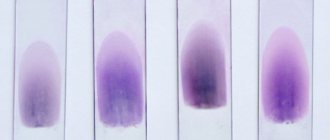
During bacterial culture, the blood is placed on a nutrient culture, due to which the bacteria begin to actively multiply and “build” colonies.
The following substances can be used as nutrient media:
- casein or whey agar;
- egg medium;
- broth made from agar and animal blood.
The nutrient medium can be of two types:
- Liquid medium. Used for small numbers of bacteria. Test tubes are used as instruments.
- Dense environment. Used for large numbers of bacteria and fungi. A Petri dish is used as a tool. It is a carefully sterilized glass or plastic round flat bowl.
The material to be studied is placed into the nutrient medium using glass or metal needles, as well as special devices called a bacterial loop. To count the number of bacteria in the blood, the designation CFU is used - the number of units (microorganisms) in a milliliter of blood that are capable of forming a colony.
There are the following degrees of growth:
- First degree. In a dense structure, colonies are completely absent; a tiny amount of them is observed in a liquid medium.
- Second degree. In a dense environment, 5-8 colonies appear.
- Third degree. In a dense environment, up to 100 colonies can be counted.
- Fourth degree. There are more than 100 colonies of microorganisms in the environment.
In the first and second degrees, a small amount of bacteria may indicate a violation of the blood sampling rules and insufficient sterility. A sign of contamination of material and equipment can also be a mixed result when colonies of different types of bacteria grow.
The advantage of bacterial culture is the possibility of conducting an antibiogram. This is a method for studying the resistance of bacteria to certain antibiotics.
The following methods can be used for this:
- Mixed disk method. Discs soaked in various antibiotics are placed in the environment with bacteria. The sensitivity of microorganisms to the drug can be judged by the zones of growth inhibition and reduction of the colony.
- E-test. The technique is the same as above, but instead of disks, pieces of paper with different concentrations of the same antibiotic are used.
Testing accuracy
A blood test for sterility is accurate in 90-95% of cases. This depends on the qualifications of the clinic and workers, compliance with all rules for collecting material. If no bacteria are found in the blood, it is sterile. This means that there is no disease. In such cases, re-analysis is not required, since there is no risk of inaccuracy of the study.
An inaccurate analysis can be considered if the CFU is very low, or different types of bacteria are detected in the analysis.
An inaccurate result of a blood test for sterility may occur for the following reasons:
- insufficient sterility when collecting blood and working with the material in the future;
- low qualifications of medical personnel and laboratory workers;
- errors when decoding the result;
- taking medications before blood collection;
- violation of the rules for transporting biological material: incorrect temperature in the thermostat or long transportation.
What testing reveals
In most cases, bacterial culture for sterility is prescribed to detect harmful bacteria and microbes in the blood, such as:
- staphylococci;
- streptococci;
- yeast fungi;
- mold spores;
- enterobacteria.
This study is necessary for patients who have reduced body defenses, as well as for people suffering from dangerous pathologies such as HIV, tuberculosis, and acute infectious diseases. In addition, testing is often prescribed if doctors cannot decide on the optimal treatment regimen.
How long does it take for the result to be ready?
After about 3 days, the person being studied can learn that their blood is sterile. Within a few days, doctors can tell about the presence of bacteria and their approximate quantity.
The exact final result is ready in about 10 days. During this time, specialists “grow” infectious pathogens in special dishes. Also during this period, the resistance of bacteria and fungi to various antibiotics is studied.
Where can I donate blood for sterility and cost?
A blood test for sterility can be taken in almost any clinic. This is a study that should be carried out in every medical institution if there is a diagnostic laboratory. In the free city clinic, blood can be tested for sterility only with a referral from the attending physician.
You can conduct research for a fee without a referral in a private clinic at any convenient time. The price in Moscow averages 1,500 rubles per analysis. The minimum cost is 300 rubles.
It depends on the components of the analysis:
- determination of the number of bacteria and fungi;
- identification of types of infectious pathogens;
- determination of drugs to which bacteria and fungi are resistant.
A blood test for sterility indicates what exactly is in the human body. These are studies such as a urine culture tank, a smear from the genital or ENT organs - this is an opportunity to study the disease in more detail.