You can take a blood test for antibodies to the hepatitis B virus at the nearest INVITRO medical office. A list of offices where biomaterial is accepted for laboratory research is presented in the “Addresses” section. Interpretation of study results contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. The doctor makes an accurate diagnosis using both the results of this examination and the necessary information from other sources: medical history, results of other examinations, etc.
Hepatitis B: carriage or disease leading to cirrhosis and cancer?
Hepatology, the study and development of new treatments for liver disease, has made incredible progress over the past two decades. Methods for accurate virological assessment of the activity of hepatitis C and B viruses in the human body, which are the most common causes of chronic hepatitis, cirrhosis, and liver cancer, have been developed and implemented. So-called “non-invasive” methods have been developed and are widely used, that is, without the use of liver biopsy, diagnosing the degree of liver damage, or establishing the stage of cirrhosis. Even more impressive progress has been made in the treatment of these diseases. We have discussed the problem of hepatitis C many times. One has only to add that a new era is opening in the treatment of hepatitis C - drugs with a direct antiviral effect have been developed and are already beginning to be used, thanks to which it is believed that within a decade it will be possible to achieve one hundred percent effectiveness of treatment. In this article we will talk about hepatitis B and new advances in its treatment.
The hepatitis B virus is 100 times more contagious than HIV (human immunodeficiency virus).
Despite the widespread introduction of vaccination against hepatitis B, the prevalence of the disease remains high. In different regions of Russia, the prevalence of carriage of the virus ranges from 1.5% to 11.5%. As with hepatitis C, the source of infection is the blood of an infected person. The routes of infection are similar: the use of non-sterile needles, instruments for various medical and non-medical (piercing, tattoos, manicure/pedicure) manipulations, the use of personal hygiene items of an infected person in everyday life (razor, scissors, toothbrush, etc.), unprotected sexual contact, transmission of the virus from an infected mother to her child. The hepatitis B virus is more stable in the external environment and more contagious than the hepatitis C viruses and human immunodeficiency viruses. Therefore, the natural routes of transmission of the B virus (sexual transmission and mother-to-child transmission) are more significant for this virus.
Complexes with this research
Examination during pregnancy.
1st trimester 10,260 ₽ Composition Male check-up No. 1 39 studies for annual preventive examination 10,960 ₽ Composition
Preparation for IVF for a man Examination to prepare a man for the IVF procedure 4,010 ₽ Composition
IN OTHER COMPLEXES
- Expanded hospital complex RUB 4,390
- Joining IVF RUB 15,090
- Pregnancy planning. Diagnosis of infections RUB 5,720
- Examination during pregnancy. 3rd trimester 5,820 RUR
- Women's check-up No. 1 RUB 11,880
How to protect yourself from hepatitis B?
The only means of protection is vaccination against hepatitis B, which is currently administered to all newborn children and adolescents. Adults with risk factors for infection should also be vaccinated. The hepatitis B vaccine is one of the safest vaccines in the world. Three-time administration of the vaccine according to a special scheme leads to the formation of specific antibodies that prevent the development of hepatitis B disease in 98% of those vaccinated. Immunity lasts for at least 8-10 years, but often remains for life.
Hidden disease
As with hepatitis C, the acute phase of the infection often occurs without jaundice. In the vast majority of cases, patients with acute hepatitis B recover and acquire lifelong immunity to re-infection (protective antibodies to viral proteins are detected in their blood serum). After infection, some people become carriers of the HBsAg virus protein, also called the “Australian antigen.” Carriage most often occurs when infected in childhood. In a small proportion of patients, acute hepatitis drags on and becomes chronic. Chronic hepatitis B, like chronic hepatitis C, often occurs latently and unnoticed for a long time. For many years, a person can feel absolutely healthy, and the first symptoms of the disease appear only at the late stage of liver cirrhosis, when the disease is more difficult to treat and the overall prognosis is unfavorable.
Hepatitis and HBsAg
So, the HBsAg antigen is one of the components of the hepatitis B virus (HBV) envelope. In the context of laboratory research, it is a marker (indicator) of the virus[1].
If we talk about the composition of the capsid (virus envelope) of hepatitis B in more detail, it is a complex combination of proteins, glycoproteins, lipoproteins and lipids of cellular origin. HBsAg in this case is responsible for the process of adsorption of the virus by the cell, that is, it ensures the absorption of HBV by hepatocytes - liver cells. Like any other virus, after being introduced into a favorable environment, it begins to replicate (produce) new DNA and proteins necessary for further reproduction (copying) of the virus. Fragments of the virus, in our case HbsAg, enter the bloodstream, through which they spread further.
This is interesting!
HbsAg has amazing resistance to both physical influences (its molecule remains unchanged at temperatures up to 60°C, as well as during cyclic freezing) and chemical influences - the antigen feels great in both extremely acidic environments (2 pH) and alkalis ( 10 pH)[2]. Able to withstand 2% solutions of phenol and chloramine, 0.1% formalin solution, and tolerate urea treatment. Thus, HBV has a very reliable shell for survival in the most unfavorable conditions.
Antigen (antigen) is literally an “antibody producer” (ANTIbody GENerator); it is capable of forming an immunological “antigen-antibody” complex. In other words, it initiates the formation of antibodies in the human body, forming specific immunity that can protect a person from a repeated attack of the virus in the future. This most important feature of HBV is the basis for the production principle of most vaccines containing either “dead” (inactivated) HBsAg or genetically modified antigens that are not capable of leading to infection, but the presence of which is sufficient to form a stable immune response to the hepatitis B virus.
The causative agent of hepatitis B belongs to the hepadnaviridae, the very name of which indicates their connection with the liver (hepa) and DNA (DNA). Thus, HBV is a hepatotropic virus, and the only one among all hepatitis viruses that contains DNA. Its activity (contagiousness and virulence) depends on many factors:
- age (for example, the probability of chronicity of the disease in children under one year of age is 80–90%, under six years of age — 30–50%, in adults — less than 5%)[3];
- individual sensitivity;
- virus strain;
- infectious dose;
- hygienic living and working conditions;
- epidemiological situation.
But in general, the contagiousness of the hepatitis B virus is low, below average, unless you completely neglect all the rules of safe sex life and hygiene.
How is the hepatitis B virus transmitted?
The infection process occurs through blood and biological fluids in the following ways [4]:
- Parenteral, that is, when it enters directly into the blood or mucous membrane, bypassing the body's protective barriers, such as the skin or gastrointestinal tract. Examples of such infection include an unsterile syringe or any surgical instrument.
- Vertical - transplacental, that is, in utero from mother to child, during childbirth, after it.
- Sexual (in all its forms).
- Household, that is, through personal hygiene items (razors, combs, toothbrushes), when applying tattoos, piercings, and so on.
Pathogenesis of hepatitis B
After infection has occurred, an incubation period begins, during which the virus multiplies and accumulates in the body unnoticed. Depending on many factors, the duration of the latent phase of viral replication can vary greatly from case to case, but on average it is 75 days[5].
This is important to know!
HBsAg is the earliest and most reliable serological marker of hepatitis B virus activity. This antigen can be detected even on the 14th day after infection, but most often it is 30–45 days, which also depends on the chosen research method. This diagnostic indicator is also very important because it makes it possible to detect HBV infection sometimes 26 days before, but guaranteed seven days before the appearance of any changes in the biochemistry of blood or urine. The dynamics of the increase in its concentration in the blood serum is similar (proportional) to the change in ALT.
At the end of the incubation period, the so-called prodromal phase of the disease begins, preceding the acute period and foreshadowing it. Then the first signs of the disease appear in the form of general malaise, weakness, fatigue, fever with a temperature on the verge of 37°C, decreased appetite, nausea, bowel disorders, joint and muscle pain, a feeling of tightness and heaviness in the right hypochondrium, irritability and apathy, skin rashes in the area of joints and itching. It should be noted here that all these symptoms can be expressed to varying degrees in different people, be completely absent or go unnoticed. The prodromal, or pre-icteric, period can last from one to 30 days. Its end is indicated by an enlarged liver and spleen, increased urobilinogen in the urine, discoloration of feces, and in the blood serum one can detect an increase in the concentrations of AlAt and AsAt, a decreased content of leukocytes, although in general the leukocyte formula is normal.
Yellowness of the skin and icterus of the sclera (yellow pigmentation of the white membrane of the eyes) mark the entry into the acute phase, or the height of hepatitis B. The increase in the content of total and direct bilirubin in the blood serum increases during the first or second week of the icteric period of the disease, reaching its maximum , after which stagnation and a gradual decline in skin pigmentation occurs until the yellow color disappears completely, which can take up to 180 days or even more.
At the peak points of the disease, in most cases, bradycardia, low blood pressure, and weakening of heart sounds are recorded. In addition, if hepatitis is severe, the following are found:
- depression of the central nervous system;
- pronounced disturbances in the gastrointestinal tract;
- tendency to bleeding in the mucous membranes (prothrombin index is greatly reduced);
- AlAt concentration is higher than AsAt;
- low mercuric acid test, ESR reaction - 2-4 mm/hour, leukopenia;
- lymphocytosis.
After the acute period (not to be confused with the severe form), the disease develops according to one of the following scenarios:
- a period of convalescence (recovery) begins with a gradual decrease (disappearance) of signs of hepatitis B at the clinical, biochemical and morphological levels;
- superinfection in the form of hepatitis D occurs and/or the disease develops into a fulminant form, into the so-called fulminant severe hepatitis (in 1% of cases) [6];
- the disease becomes active chronic:
- a. recovery;
- b. liver cirrhosis and carcinoma (20–30%)[7];
- the disease goes into a state of stable remission (stable chronic form):
- a. cure;
- b. extrahepatic pathologies.
This is important to know!
HBsAg persists throughout the acute stage of hepatitis B. If the antigen is detected in the blood for more than 180 days, it means that the disease has become chronic[8].
From the point of view of the burden on the body, doctors define three main forms of acute hepatitis B: mild, moderate and severe. From the standpoint of the severity of the symptoms of the disease, its icteric (typical), anicteric and subclinical (atypical) forms are distinguished. Typically, the disease proceeds exactly as described above. Most cases occur in atypical forms, when there is no pigmentation of the skin and mucous membranes, and other symptoms are mild (anicteric variant) or when any clinical manifestations are absent at all (subclinical form).
No matter how paradoxical it may sound, in most cases, hepatitis B does not require any special treatment: supportive therapy based on hepatoprotectors, vitamins and microelements, plenty of fluids and a strict diet is sufficient. Of course, the exception is cases with an inherited infection or when there is an immune deficiency (as well as immunosuppressive therapy), concomitant diseases or a severe form of the disease. Otherwise, the human immune system independently copes with the virus within one or two months, acquiring specific immunity. Many people who develop antibodies to the virus claim that they have never had it, when in fact they simply did not notice it or confused it with the regular flu. But the situation is not so successful for all infected people; in addition, no matter in what form a person contracts hepatitis B, there remains an increased risk of developing certain liver pathologies throughout his life.
There is another interesting fact: the so-called asymptomatic antigen carriers[9]. These are not the people who suffered from hepatitis B in a latent, subclinical form - they did not have it at all and do not suffer from it. At the same time, HBsAg carriers remain dangerous to others. Such people act as the main reservoir of infection. This phenomenon has not been studied, but it is likely that the virus itself leaves this category of people “untouched” in order to preserve its population for a rainy day. By what criteria the virus preserves the health of these particular people without causing any harm to their body is unknown. But this is just a hypothesis, and in any asymptomatic carrier the virus can wake up at any minute, or it may never do so.
The diagnostic criteria for asymptomatic carriage are as follows:
- HBsAg antigen is detected in the blood after 180 days;
- the HBeAg marker is not detected in the serum;
- anti-HBe present;
- HBV DNA level in blood serum is less than 105 copies per 1 ml;
- AlAt/AsAt concentrations show normal values during repeated tests;
- during liver biopsy, the histological activity index (MGA) of the inflammatory-necrotic process in the liver is usually below 4.
Hepatitis B markers
As you can see, the serological marker HBsAg is the first, main, most reliable, but far from the only indicator of hepatitis B infection; in addition to it, other antigens, antibodies and viral DNA molecules also require determination in the blood serum (see Table 1).
Table 1. Markers of HBV infection.
| Marker | Marker characteristics | Clinical significance |
| HBeAg | HBV nuclear e antigen, appears in the first week after HBsAg and disappears after 20–45 days | indicates HBV replication in hepatocytes, high virus activity in the blood and a high risk of perinatal transmission of the virus |
| HBcAg | HBV nuclear core antigen | marks HBV replication in hepatocytes, is detected only during morphological examination of liver biopsy specimens and at autopsy, is not detected in free form in the blood |
| anti-HBc (total) (HBc Ab) | total antibodies to HBcAg, detected 7–14 days after HBsAg | an important diagnostic marker, especially with negative results of HBsAg indication, used for retrospective diagnosis of hepatitis B and for unverified hepatitis, HBcAg is determined without division into classes |
| IgM anti-HBc (HBc Ab IgM) | class M antibodies to nuclear antigen , present in the blood from 60 to 540 days | one of the earliest serum markers of hepatitis B, its presence in the blood indicates an acute infection (phase of the disease), in the chronic form it marks HBV replication and the activity of the process in the liver |
| anti-HBe (HBeAb) | antibodies to the e-antigen are found in 90% of patients after 60 days | may indicate the beginning of the convalescence stage (with the exception of the mutant form of HBV) |
| anti-HBs (HBsАb) | protective antibodies to HBV surface antigen | indicate a past infection or the presence of post-vaccination antibodies (their protective titer against HBV infection >10 IU/l); detection of antibodies in the first weeks of hepatitis B predicts the development of a hyperimmune variant of fulminant hepatitis B |
| HBV-DNA | Hepatitis B virus DNA | marker for HBV presence and replication |
The above markers appear and disappear in a certain sequence in accordance with the stages of the disease. Some, such as IgG anti-HBc, remain for life. Only the entire set of markers provides a complete and reliable diagnostic picture. In addition, acute, chronic, fulminant and mixed hepatitis have their own serological profiles (more on this below).
It is impossible not to touch upon such a rare but extremely dangerous phenomenon as parallel infection with hepatitis D (HDV); it can occur in two variants:
- Coinfection, that is, simultaneous infection with hepatitis B and D (delta) viruses, which leads to a much more severe form of the disease, but almost does not become chronic.
- Superinfection, that is, the addition of HDV to a previously “dormant” HBV in the form of an acute severe form or as an exacerbation of the chronic form of hepatitis B. In the latter case, after suppression, it also becomes chronic with a prognosis of cirrhosis or liver cancer.
HDV is a kind of parasite of the hepatitis B virus, its satellite. It cannot replicate in the absence of HBV, since the synthesis of its shell proteins is impossible without the presence of the hepatitis B virus in hepatocytes. Thus, you can get hepatitis B without delta infection, but the other way around will not work. The addition of HDV can cause fulminant hepatitis with the development of acute liver failure and hepatic encephalopathy, which grow rapidly, sometimes leading to death. If the result is positive for the HBsAg antigen, delta infection must be diagnosed. For this purpose, serological markers are used (see Table 2).
Table 2. Markers of HDV infection.
| Marker | Marker characteristics | Clinical significance |
| IgM anti-HDV | class M antibodies to hepatitis D virus | mark HDV replication in the body |
| IgG anti-HDV | class G antibodies to hepatitis D virus | indicate possible HDV infection or previous infection |
| HDAg | hepatitis D virus antigen | marker for the presence of HDV in the body |
| HDV-RNA | Hepatitis D virus RNA | HDV presence and replication marker |
What is important to know about the forms of hepatitis B virus infection?
Chronic infection can occur in two main forms:
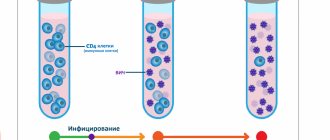
The first form is inactive carriage of HBsAg. It is characterized by the absence of viral particles in the blood serum or their detection in a low titer, the absence of inflammation in the liver and, as a rule, a non-progressive course. With a decrease in immunity, inactive carriage of HBsAg can turn into the active form of hepatitis B.
The second form is chronic active hepatitis B. It is characterized by the presence of a large number of viral particles in the blood, the presence of inflammation in the liver, which is reflected in changes in the so-called liver tests (or enzymes), and a progressive course with the risk of developing cirrhosis and liver cancer. In recent years, it has been found that the higher the concentration of virus in the blood, or “viral load,” the higher the risk of developing cirrhosis and liver cancer.
It is impossible to distinguish between these two forms based on the patient’s well-being and only clinical signs of the disease (which, as with inactive carriage, may be completely absent in a patient with chronic hepatitis B).
When do you need to get tested for Hepatitis B, HBs Ag (quality)?
- Suspicion of infection with viral hepatitis B;
- Changes in liver biochemistry, indicating liver damage;
- Development of jaundice;
- Screening during pregnancy;
- Comprehensive examination before hospitalization;
- Pre-employment screening for specialists in certain professions (medical workers and others);
- Examination of people from groups at high risk of infection (receiving intravenous injections, undergoing hemodialysis, blood donors and others).
What to do if you are diagnosed with HBsAg?
Unfortunately, hepatologists are often faced with underestimation on the part of the patient, as well as doctors of other specialties, of the seriousness of HBsAg detected over many years. A patient who is diagnosed with HBsAg for the first time must undergo an examination, which will make it possible to make a correct diagnosis - to distinguish between inactive carriage of HBsAg and active chronic hepatitis B that requires treatment. To do this, the hepatologist will suggest that you do a number of studies: - a study of a biochemical blood test, - a study of the viral load using quantitative PCR (polymerase chain reaction) - a study for the presence of another protein (or antigen) of the hepatitis B virus, which characterizes the high infectiousness of the patient, — HBeAg — study for the presence of a companion virus of hepatitis B - delta virus — study of alpha-fetoprotein (tumor marker of a liver tumor) — ultrasound examination of the liver — fibroelastography to clarify the stage of liver fibrosis (other studies are possible according to indications)
Modern treatment of chronic hepatitis B can stop the disease!
If you are nevertheless diagnosed with chronic hepatitis B, it is necessary to prescribe antiviral treatment, that is, treatment using drugs that can block the replication of the virus.
The goal of modern antiviral therapy for chronic hepatitis B is to persistently suppress the replication of the virus, achieve remission of the disease, that is, transfer the process to an inactive state. When this result is achieved, the development of liver cirrhosis and its complications (such as ascites, internal bleeding, liver failure) is prevented, and the risk of developing liver cancer is greatly reduced.
A number of drugs with antiviral effects are currently registered for the treatment of chronic hepatitis B. Among the new generation of drugs there are safe drugs that can be used for several years, drugs to which the virus does not develop resistance. Your attending physician will help you choose a treatment appropriate to the stage and form of your disease.
References
- Ivashkin, V.T., Mayevskaya, M.V., Pavlov, Ch.S. and others. Clinical recommendations of the Russian Society for the Study of the Liver and the Russian Gastroenterological Association for the treatment of complications of liver cirrhosis. - Russian Journal of Gastroenterology, Hepatology, Coloproctology, 2021. - V. 26(4). — P. 71-102.
- Schwarz, W., Heidi, M., Nancy, E. False positive hepatitis B surface antigen test caused by hepatitis B vaccine, The Pediatric Infectious Disease Journal, 2001. - Vol. 8(2). — P. 189-193.
- Tripathi, N., Mousa, O. Hepatitis B. - In: StatPearls, 2020.
- Anjum, Q. False positive Hepatitis B Surface Antigen due to recent vaccination. - IntJHealthSci (Qassim), 2014. - Vol. 8(2). — P. 189-193.
Is it necessary to follow a diet for patients with chronic hepatitis B?
No special diet is required for chronic viral hepatitis, however, you should avoid drinking alcohol even in small doses, since the combined effect of alcohol and the virus on the liver significantly increases the risk of developing cirrhosis and liver cancer. If you are overweight, you should limit your intake of fats and high-calorie foods, since fat deposition in the liver accelerates the development of cirrhosis. Factors that reduce immunity, in particular sun exposure, should be avoided, that is, you should not use a solarium or sunbathe on the beach. It is advisable to quit smoking. You can continue to exercise. Swimming and hardening procedures that support the state of your immunity are useful.