The human immunodeficiency virus (HIV) belongs to the family of retroviruses and is the cause of AIDS, one of the most famous diseases of our time. There are two forms of the virus: HIV-1, which is more common in Europe, Russia, Asia, the United States and Australia, and the rare HIV-2, mainly found in West Africa.
The virus spreads through blood and body fluids (sperm, vaginal discharge, breast milk), so it is most often transmitted through unprotected sex, the use of unsterile medical instruments, drug injection and breastfeeding.
HIV attacks the cells of the immune system. As the disease progresses, the body loses its ability to fight both HIV infection itself and other infectious diseases, and AIDS develops - a stage of the disease in which the immune system no longer works. Most often, secondary diseases occur against the background of AIDS, such as pneumonia, fungal infections, tuberculosis, and other severe pathologies.
It is important to promptly identify HIV carriage and register with a regional AIDS center to receive the necessary therapy. Antiretroviral therapy prescribed to patients with HIV can save life and prolong the asymptomatic stage of the disease. The second, no less important factor is the patient’s knowledge of his HIV status, which significantly reduces the risk of infecting other people.
At the onset of the disease there may be no painful manifestations; some patients develop a flu-like condition. There is a so-called “serological window” period, when the virus is already multiplying in the body, and the immune system has not yet produced antibodies. At this time, the test for antibodies to HIV may be negative, but the person is already capable of infecting others. Therefore, in case of questionable contact or risk of HIV infection, repeat tests after 3 and 6 months are recommended.
The standard method for laboratory diagnosis of HIV infection is the determination of antibodies/antigens to HIV. To confirm the results of HIV antibodies, confirmatory tests (immune, linear blot) are used.
The HIV test is a screening test and has high sensitivity. Laboratory tests that have the highest sensitivity produce very few false negative results, but may produce false positive results in a small percentage of cases.
In what cases is research usually prescribed?
- For symptoms of unknown origin that last 2–3 weeks or more: low-grade fever, diarrhea, night sweats, sudden weight loss, swollen lymph nodes.
- For recurrent herpes, pneumonia, tuberculosis, toxoplasmosis and other chronic infections.
- For detected sexually transmitted diseases (syphilis, chlamydia, gonorrhea, genital herpes).
- When having unprotected sex with a new partner or a partner whose HIV status the patient is not sure of.
- During transfusion of blood or its components.
- When using injecting drugs.
- During pregnancy and when planning pregnancy.
- In case of an accidental injection or cut with a medical syringe or other instrument containing HIV-infected blood.
- During medical examination, before hospitalization and surgical interventions.
Indications for the study
Indications for prescribing the analysis are preparation for hospitalization and planned surgery.
For preventive purposes, a study should be conducted if infection through sexual contact is suspected. First of all, this applies to people at risk: those who use drugs administered intravenously, frequently change sexual partners and do not use protective equipment. The human immunodeficiency virus multiplies quite slowly in the human body, and quantitative results regarding antigens and antibodies to the virus can, as a rule, be obtained no earlier than 3-6 weeks after infection. However, there are still no clinical symptoms of the disease.
After three months, HIV antigens and antibodies to the virus are detected in almost all patients. Thanks to the advent of new fourth-generation combined test systems, obtaining an accurate result of a qualitative analysis for HIV infection is possible within two weeks from the moment the virus enters the body. This test detects the HIV p24 antigen, a protein of the viral capsid (the outer shell of the virus).
Testing for antibodies to HIV 1/2 and HIV 1/2 antigen is prescribed at the planning stage and during pregnancy management, when transmission of the virus to the fetus is possible. The analysis is also carried out after childbirth, since the child of an HIV-positive mother can be infected during passage through the birth canal and during breastfeeding.
Fever, weight loss without objective reasons, increased fatigue, enlarged regional lymph nodes, sweating, especially at night, prolonged cough, diarrhea - these persistent clinical symptoms of unknown origin, noted within 2-3 weeks, also serve as an indication for a blood test. HIV 1/2 antibodies and HIV 1/2 antigen.
Skin manifestations can also be a symptom of HIV infection, as they develop against a background of weakened immunity. These include recurrent herpetic rash, affecting large areas of the skin, oral cavity, and genitals. Herpes also affects the deep layers of the skin with the development of an ulcerative-necrotic form. Ulcers and erosions form, followed by the formation of scars, which do not occur with ordinary herpes.
Another characteristic symptom of HIV infection is hairy leukoplakia, which is associated with the activation of a latent infection caused by the Epstein-Barr virus (which indicates immunosuppression). The disease manifests itself as white thread-like formations with further keratinization of the affected areas of the tongue and oral mucosa.
Extensive fungal infections (primarily yeast fungi of the genus Candida) are also a typical symptom accompanying HIV infection. First, candidiasis affects the mucous membrane of the mouth and esophagus, then spreads to the mucous membranes of the gastrointestinal and genitourinary tract. In this case, large lesions are formed, characterized by pain and a tendency to ulceration.
HIV infection may be accompanied by the development of extensive papillomatosis. In HIV-infected women, cervical canal papillomas tend to quickly cause cervical cancer.
An AIDS indicator disease is Kaposi's sarcoma, a multifocal vascular tumor that affects the skin and mucous membranes. Its foci in the form of reddish or brownish nodules and plaques merge, quickly spreading throughout the body. Over time, they form tumor fields that ulcerate and suppurate.
Pathological conditions that accompany HIV infection in almost all patients include polyadenopathy (enlarged lymph nodes). As a rule, the sub- and supraclavicular, chin, parotid and cervical lymph nodes enlarge first. In the future, they may be accompanied by enlargement of the inguinal and femoral lymph nodes. They can be soft or firm to the touch, painless and mobile. Sometimes several lymph nodes merge, forming a kind of conglomerate. Inflammation of two or more groups of lymph nodes is considered a sign of generalized lymphadenopathy. Damage to the lymph nodes can be observed for several years, with periods of exacerbation followed by remission.
Pulmonary diseases that accompany HIV infection include tuberculosis and pneumonia.
An analysis for antigens and antibodies to HIV is recommended if the patient is diagnosed with sexually transmitted diseases (syphilis, chlamydia, gonorrhea, genital herpes, bacterial vaginosis).
What do the test results mean?
“Not detected” means that the screening test did not detect antibodies to HIV, but this does not exclude the presence of infection during the “serological window”.
“Detected” means that antibodies to HIV have been detected. The study was first performed twice in a screening laboratory, followed by confirmatory testing in a reference laboratory. The initially positive serum is re-examined by the reference laboratory using a test system from another manufacturer, and then, upon receiving a second positive result, it is examined by immunoblotting. It should be remembered that a positive result of antibodies to HIV is not a diagnosis. The diagnosis of HIV infection can only be made by a doctor upon examination of the patient, taking into account all the results of his research.
The test result “not detected” can be obtained the very next day after the test. Positive results are sent to a reference laboratory for confirmation and may be delayed for up to 10 days.
How to take a blood test for HIV
Preparing for the test is simple - before donating blood (8 hours), you should refrain from eating. Therefore, in almost all clinics, the test material is collected early in the morning, this makes it easier for patients, they do not eat anything in the evening, and after the procedure they can go to breakfast.
Depending on the blood test method, the HIV result may be ready after 2-10 days. Even if the reaction is negative, it is recommended to take the test again after 2-3 months, since in the early stages the presence of the virus in the body is difficult to diagnose even with the help of modern and expensive equipment.
To take a blood test for HIV, contact the President-Med medical centers in Moscow and Vidnoye
Modern methods of HIV diagnosis
Currently, a two-level approach is used in diagnosing HIV - indirect and direct tests. Indirect tests can detect specific antibodies to HIV in the patient’s blood, while direct tests help identify HIV itself and determine the degree of viral load in the body. In Russia, standard HIV diagnosis includes the following laboratory research methods:
- ELISA (enzyme-linked immunosorbent assay).
- Immunoblot (immune blotting).
The following techniques can also be used:
- Express ICA test (immunochromatography).
- PCR (polymerase chain reaction).
Diagnostic principles of laboratory tests and the degree of their reliability are given in the table below.
| Research method | Diagnostic principle | Credibility | Time after infection |
| Express ICA test | Detection of antibodies to HIV | 93-99% | from 3 weeks |
| ELISA screening test | Detection of antibodies to HIV and virus antigens | ||
| Immunoblot | Antibodies to several HIV proteins | 99,9% | from 5 weeks |
| PCR | The genetic material of the virus is being studied | 80% | from 5 days |
| 98% | from 2 weeks |
When conducting research, it is important to use ultra-precise equipment and correctly interpret test results. Otherwise, the diagnostic accuracy is reduced. At the same time, experts believe that it is most rational to conduct research in the following sequence.
- First, express diagnostics based on the ICA method.
- In case of a positive result, another blood test using the ELISA method.
- A positive second result means further examination is carried out using ELISA or immunoblotting.
- In exceptional cases, a more complex and expensive PCR method can be used to make a final diagnosis.
Express tests using the ICA method or ELISA screening, which involves a serological enzyme immunoassay of blood, are performed within 15-30 minutes. High speed of diagnosis is relevant in emergency cases, when planning urgent operations. But to make a final diagnosis, it is necessary to use the main diagnostic method - immunoblotting. If the results of ELISA and immunoblotting contradict each other, then it is possible to carry out reference diagnostics - analysis by two methods at once. PCR is used in exceptional cases, because This is the most expensive research method. Next, we will analyze each of the diagnostic methods in more detail.
Express ICA test
Immunochromatographic tests have proven themselves well in the rapid diagnosis of HIV. Visually, they look like strips, onto the surface of which the biological material being studied (blood, saliva) is applied. To obtain the result, it will take only 10-15 minutes, after which the test will show either a color and control strip - a positive result confirming the presence of antibodies to HIV, or only the control strip - a negative result.
Recently, the American company OraSure Technologies has launched mass production of rapid tests for home use. They are available without a prescription and can be used by anyone if desired. However, it is necessary to take into account that ICA is inferior to the ELISA method in terms of diagnostic accuracy, and immunoblotting is necessary to make a final diagnosis.
ELISA screening test
The principle of the method is based on the ability of artificially created HIV proteins to capture specific antibodies produced in the human body. As a result of interaction, the ELISA test system changes the color of the indicator. The resulting color changes are processed using equipment that produces an analysis result. It should be taken into account that the screening test is designed to detect not HIV as such, but antibodies to it. And since it takes time for them to appear in the body, it is most advisable to carry out screening 3-6 weeks after the fact of possible infection. To do this, only 5 ml of blood from the patient’s vein is enough, which is taken on an empty stomach, i.e. 7-8 hours after the last meal.
In addition to a positive or negative result, the ELISA test can give a false positive or false negative result.
- False positive - we can talk about antibodies that are similar in structure, which are produced in the body during autoimmune diseases, multiple myeloma, alcoholic hepatitis and other pathologies.
- False negative – most likely, the testing was done prematurely or the immune system is too weak and does not produce antibodies to HIV.
If the result is questionable, the test is repeated.
Immune blotting
Immunoblot is the main method for diagnosing HIV, combining an enzyme-linked immunosorbent assay (ELISA) with preliminary electrophoretic transfer of virus antigens onto a nitrocellulose strip. To identify them, the analysis is carried out in three stages:
- preparation of nitrocellulose strips;
- examination of a sample of the patient’s biological material;
- interpretation of the result.
Thus, during the study, the main HIV proteins are distributed over the surface in the form of separate bands, which appear during the enzyme immunoassay reaction and confirm the presence or absence of antibodies to HIV antigens. The results obtained during the immunoblotting study are considered final.
Polymerase chain reaction (PCR)
The main difference between PCR and other diagnostic methods is that the test system determines the DNA of the virus. It can be used to detect even single viral particles. The method can be used already on the 5th day after the fact of possible infection with an accuracy of up to 80%, which allows for early diagnosis of HIV. However, PRC is carried out only in exceptional cases.
- to diagnose newborns born from HIV-infected mothers;
- with questionable immunoblot results;
- for operational research of donor blood;
- to assess the level of HIV in the blood of an infected patient.
Despite the high sensitivity of the PCR method, it has lower diagnostic sensitivity for HIV, which is explained by the variability of the virus genome. Therefore, this method is not used to make a final diagnosis.
The importance of clinical diagnosis of HIV
In the understanding of many people, an HIV-infected person looks sick and exhausted. He coughs, sneezes, itches, groans, everything hurts... In fact, this is not so! The problem is that after HIV infection and during the subsequent incubation period, there are no symptoms at all. Then comes the acute phase, during which there are symptoms reminiscent of ARVI or flu. But they soon pass, and the so-called latent period begins - a long period of time when HIV infection does not show itself in any way. From the moment of infection to the pre-AIDS stage, about 10 years can pass, during which neither the patient himself nor his environment even suspects about the disease. And when it already declares itself at full capacity, it is very difficult to control it. It is difficult to resist the complications of HIV and maintain the practically destroyed human immune system.
It is very important to understand that, although there are risk groups - homosexuals, drug addicts and girls of easy virtue - for the most part, patients with HIV infection are ordinary people. They study, go to work, visit public places, meet people on the Internet - in general, they live like everyone else. Unfortunately, no one is immune from HIV. Unprotected sexual intercourse in a fit of passion, a treasured tattoo without maintaining sterility, a half-price manicure from a novice artist, a street fight - all these and many other everyday situations can result in HIV infection.
Only those who do not live do not make mistakes! We cannot know everything in advance, we cannot correct mistakes that have already been made, but we can take simple steps to correct their consequences - go to the nearest dermatovenerology clinic, a local clinic or a specialized AIDS center for testing and early diagnosis of HIV.
ESR indicator
A very important data from the CBC is the erythrocyte sedimentation rate, or ESR for short.
The norm is 4-10 mm per hour.
When the ESR accelerates, this indicates an imbalance in the protein balance of the blood.
Unfortunately, the indicator is completely nonspecific: ESR increases with any infection, injury, or oncology.
Patients are characterized by such a combination when the erythrocyte sedimentation rate is increased to 30-40-50 mm per hour.
And the person feels more or less normal.
This picture is associated with a decrease in the number of white blood cells.
In particular, those lymphocytes that synthesize immunoglobulin proteins.
A decrease in the amount of these immune proteins entails a relative increase in albumin proteins, which is reflected in the increase in ESR.
Detailed description of the study
RULES FOR CONDUCTING TESTING FOR HIV INFECTION
Human immunodeficiency virus (HIV) is the causative agent of chronic systemic viral infection (HIV infection). It belongs to the retrovirus family, or Retroviridae. A viral particle is genetic material (RNA) packaged in a protein capsule - the viral capsid, which in turn is covered with a viral envelope, or supercapsid. Today, two types of the virus are known: HIV-1 and HIV-2. HIV-2 is prevalent mainly in West African countries.
HIV infection is a slowly progressive disease in which the immune system is damaged with the development of acquired immunodeficiency syndrome (AIDS). AIDS is the terminal stage of development of HIV infection, which is accompanied by a wide range of secondary (opportunistic) diseases. With AIDS, opportunistic infections affect all organs and systems of HIV-infected people.
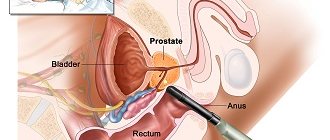
After infection, the virus penetrates into cells on the surface of which the CD4 receptor (cluster of differentiation 4), a transmembrane glycoprotein molecule, is present. This receptor is found in only one type of cell – T-helper cells. This is a population of white blood cells (T-lymphocytes), which plays a key role in maintaining the required level of the adaptive immune response, that is, the body's response to foreign agents. This leads to dysfunction of the immune system in HIV-infected people.
There is no vaccine that prevents HIV infection. However, drugs have been developed for antiretroviral therapy, which can stop the development of HIV infection and prevent immunodeficiency.
Qualitative determination of RNA makes it possible to detect HIV infection before detecting antibodies to the causative agent of HIV infection.
New and alternative methods for diagnosing HIV
Recently, employees at the University of Pittsburgh developed a new highly sensitive test for detecting hidden viruses - the TZA test. It requires less time and patient blood. The principle of TZA action is to search for a gene that is activated only when the virus replicates. Despite the fact that the developers are confident in the effectiveness of the test, most experts are inclined to believe that TZA will not be able to completely replace existing diagnostic methods, since it is characterized by a different mechanism of action and is not suitable for absolutely every HIV-infected patient.
Favorable timing for HIV diagnosis
The fact of possible infection and poor health for no apparent reason are two good reasons to contact a specialist. But a negative antibody test result does not always mean that a person is not infected, as there is a “seronegative window” period (the time between infection and the appearance of antibodies) that is about three months. Therefore, it is better to repeat them 3 months after possible infection. If the answer is again negative, but your anxiety does not go away, and you are sure that you are infected with HIV, then the laboratory diagnosis must be repeated 6 months after the fact of infection.
As for feeling unwell, a combination of the following symptoms may be a reason to get tested for HIV:
- enlarged lymph nodes in the neck, groin, and armpits;
- fever;
- muscle pain or headaches;
- thrush and fungal infections, including oral candidiasis;
- inflammation of the mucous membranes of the nose, mouth or pharynx;
- night sweats;
- aching joints;
- prolonged diarrhea;
- nausea, vomiting;
- a sharp decrease in body weight;
- skin rashes.
It is important to understand that from the moment when the first signs of HIV infection appear until the moment the disease enters the latent stage, very little time passes - about 3-6 weeks from the fact of infection. Don't lose sight of this period of time! Since you will live for the next 8-10 years, feel normal and not even suspect that you have HIV infection. Precious time will be lost.