Now this word is on everyone's lips. But what is the role of antibodies in protecting the body? Does an antibody test really eliminate all questions about whether you have been exposed to the virus? How accurate is it? Why might antibodies make the disease worse? Read in our analysis
Short
Antibodies are created by immune cells to fight a specific pest: virus, bacteria or parasite.
They do not appear immediately, because the body needs time to study the pest (pathogen).
The more antibodies, the stronger the protection. Over time, they may disappear, but cells are able to create them again when faced with a familiar danger.
There can be many antibody variants for one pathogen. Not everyone can “see” tests, so their accuracy is not absolute.
The virus can mutate, and then the old antibodies will not be able to recognize it. Or, having recognized it, they will not be able to neutralize it and themselves will become its conductors into the cells.
How are antibodies related to immunity?
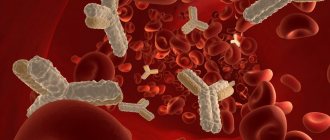
This is one of its main tools in the fight against threats. Antibodies are not independent cells, but protein structures that are created by protective cells (lymphocytes) for a specific target. It happens that it turns out to be completely harmless substances - for example, pollen or chicken egg whites. This is how an allergic reaction occurs. But most often, antibodies fight viruses, bacteria, parasites and other “saboteurs”.
Antibodies can also be produced against the body’s own cells—they are called autoimmune. Each cell of the body has special protein molecules - identification marks that say that it is “our own”. But if the cell has grown old, died or degenerated into a malignant one, an “order” for destruction is also sent against it.
That is, antibodies destroy viruses and bacteria?
Not really. The purpose of antibodies is to neutralize the “intruder” so that it cannot reproduce, or to mark it for destruction. For example, they stick to viral particles, preventing them from entering the cell. Since the virus is unable to reproduce outside cells, it dies. Antibodies can also clump bacteria together into clumps, which are then devoured by phagocytes, or activate a system of immune proteins that will break through the bacterial membrane and kill it.
An antibody works like a molecular master key: it is born already tailored to a certain structural feature of a foreign body. For example, this could be a site (spike) on the surface of a viral particle through which it binds to a cell. The antibody blocks the spike and the virus cannot infect the cell. Related viruses may have similar structural elements, and then antibodies to one member of the family will be effective against another. For example, some people who have had SARS in the past (caused by the SARS-CoV-1 virus) already have effective antibodies against its relative, SARS-CoV-2, which causes COVID-19 infection.
Why are antibodies not immediately formed during illness?
To create the right antibody, the immune system first needs to study the offender. To achieve this, different “departments” cooperate in the body. First, interceptor cells (macrophages) absorb and digest foreign particles. Then they are introduced to their structure of “laboratory” cells (B-lymphocytes). They, in turn, form many copies of themselves with different variants. The “memory” of immunity is not based on antibodies alone. Cells also have it. Lymphocytes that produce antibodies remain dormant until they encounter the pest again. At the right moment, they can quickly create new “shells”. True, such preparation also has a downside, which prevents the creation of effective vaccines against some viruses.
When faced with a familiar virus, the body first throws into battle the cells that were trained to attack it. He suspends the development of new antibodies to save energy. But the virus can mutate in such a way that its vulnerabilities are protected, and the immune system does not recognize this. Even worse: the virus can use the antibody attached to it to enter an immune cell and infect it.
Antibodies to thyroid peroxidase are specific immunoglobulins directed against the enzyme contained in the cells of the thyroid gland and responsible for the formation of the active form of iodine for the synthesis of thyroid hormones. They are a specific marker of autoimmune thyroid diseases.
Synonyms Russian
Antibodies to thyroid peroxidase, microsomal antibodies, antibodies to microsomal antigen, ATTPO, ATPO.
English synonyms
Anti-thyroid Peroxidase Autoantibodies, Antimicrosomal Antibodies, Antithyroid Microsomal Antibodies, Thyroid Peroxidase Autoantibodies, TPO Antibodies, Thyroid Peroxidase Test, Thyroid microsomal antibody, Thyroperoxidase antibody, TPOAb, Anti-TPO.
Research method
Chemiluminescent immunoassay.
Determination range: 5.00 - 600.00 IU/ml.
Units
IU/ml (international unit of milliliter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
Do not smoke for 30 minutes before the test.
General information about the study
This test is designed to determine specific antibodies to thyroid tissue in the blood serum - anti-TPO. They are formed when the human immune system mistakenly recognizes thyroid tissue as a foreign biological substance, which can lead to thyroiditis, damage to the thyroid tissue and various disorders of its function.
The thyroid gland synthesizes a number of vital hormones: thyroxine (T4) and triiodothyronine (T3), which are of great importance in the regulation of metabolism. In turn, the functioning of the thyroid gland is regulated by the pituitary thyroid-stimulating hormone (TSH), which ensures adequate production of thyroid hormones depending on the needs of the body. The damaging effect of antibodies on various biochemical structures can lead to disruption of the normal production of thyroid hormones and negatively affect the regulation of its function, which ultimately causes chronic pathologies associated with hypo- or hyperthyroidism. Hypothyroidism manifests itself in the form of symptoms such as weight gain, goiter, dry skin, hair loss, constipation, and increased sensitivity to cold. Hyperthyroidism is accompanied by sweating, rapid heartbeat, anxiety, tremors in the limbs, weakness, sleep disturbances, weight loss, and exophthalmos.
The thyroid enzyme thyroid peroxidase plays a key role in the formation of thyroid hormones. Thyroid peroxidase is involved in the formation of the active form of iodine, without which the biochemical synthesis of thyroid hormones T4 and T3 is impossible. The appearance of antibodies to this enzyme in the blood disrupts its normal function, resulting in a decrease in the production of the corresponding hormones.
Quantitative serum analysis for antibodies to thyroid peroxidase is the most sensitive method for diagnosing autoimmune thyroid diseases. Deviation from the norm of its results is an early sign of Hashimoto’s thyroiditis and diffuse toxic goiter (Graves’ disease). Modern highly sensitive methods for detecting antibodies to thyroid peroxidase make it possible to correctly diagnose 95% of patients with Hashimoto's thyroiditis and 85% of patients with diffuse toxic goiter. During pregnancy, anti-TPO can significantly affect the development of the thyroid gland and the health of the unborn child, since they are able to penetrate the placental barrier from the mother's blood into the fetus. Anti-TPO levels are often elevated in other thyroid diseases, such as idiopathic hypothyroidism, adenoma and cancer, and in all types of autoimmune diseases, including rheumatoid arthritis, systemic lupus erythematosus, insulin-dependent diabetes mellitus, autoimmune adrenal insufficiency and pernicious anemia, which In a number of cases, this indicates the involvement of the thyroid gland in this pathological process. Therapy with certain medications (amiodarone, lithium, interferon) can also cause the appearance of antibodies to thyroid peroxidase and, as a result, hypothyroidism.
What is the research used for?
- First of all, to identify various autoimmune diseases of the thyroid gland: Hashimoto's thyroiditis,
- diffuse toxic goiter,
- postpartum thyroiditis,
- autoimmune thyroiditis,
- hyperthyroidism or hypothyroidism in newborns.
When is the study scheduled?
- For symptoms of disruption of the normal functioning of the thyroid gland.
- When the results of other tests indicate any dysfunction of the thyroid gland.
- When long-term monitoring of the health of a patient with thyroid disease is required, which includes conducting laboratory tests at certain intervals to monitor the effectiveness of treatment.
- If the possibility of prescribing therapy associated with the risk of developing hypothyroidism as a result of the appearance of anti-TPO (lithium drugs, amiodarone, interferon alpha, interleukin-2) is being considered.
- If it is necessary to find out the causes of miscarriage, preeclampsia, premature birth, unsuccessful attempts at artificial insemination - this may be due to the influence of specific antibodies.
- If other test results (T3, T4 and/or TSH) indicate thyroid dysfunction.
- For an autoimmune disease that initially did not affect thyroid function (rheumatoid arthritis, systemic lupus erythematosus, pernicious anemia, systemic autoimmune vasculitis, insulin-dependent diabetes mellitus), if symptoms appear that the thyroid gland is involved in this process.
- If the patient is at high risk for autoimmune thyroiditis (such as pregnant women with a history of this disease in their family).
What do the results mean?
Reference values: 0 - 34 IU/ml.
Reasons for increasing anti-TPO levels
In general, the detection of anti-TPO in blood serum indicates autoimmune aggression against the thyroid gland, and the more the test results deviate from the norm, the higher the likelihood of this type of pathology.
- A slight or moderate increase in thyroid peroxidase levels can be caused by many thyroid diseases and autoimmune disorders: rheumatoid arthritis, systemic lupus erythematosus, insulin-dependent diabetes mellitus, thyroid cancer, systemic autoimmune vasculitis, etc.
- A significant deviation of the results from the norm most often indicates an autoimmune disease of the thyroid gland, for example Hashimoto's thyroiditis, diffuse toxic goiter.
- Positive test results during pregnancy indicate the possibility of hyperthyroidism in the child (during intrauterine development or after birth).
- If the test for antibodies to thyroid peroxidase is used for long-term monitoring of the progress of treatment, and the level of antibodies either remains high throughout the entire observation period, or decreases at the beginning of therapy, and then increases again after a certain period of time, this indicates insufficient effectiveness of the treatment. therapy, as well as that the disease continues or is exacerbating.
- Sometimes the level of anti-TPO is elevated in practically healthy people, more often in women, and this probability increases with age. Most of them are never bothered by thyroid disease, but in any case, the patient’s health condition is monitored for some time.
Reasons for decreased anti-TPO levels
A decrease in the concentration of anti-TPO to low or even more undetectable values indicates that the treatment is successful.
What can influence the result?
- A large amount of fat in the blood serum.
How is an antibody test done?
To detect antibodies, tests use antigens - areas on the surface of the virus to which these same antibodies bind. They are fixed in the wells of special tablets, or dies, and the patient’s blood is added to the wells. Staining then reveals the antibodies that would have attached to the antigens. If the sample changes color, this should mean that antibodies are present.
Rapid antibody tests are typically used to provide a simple yes/no result. They have two lines, like a pregnancy test. There are also those who look separately for proteins of classes M (which are formed during illness) and G (which remain in the blood after recovery). In this case, there are already three stripes in the test.
There are also quantitative tests. They already make it possible to determine not only the presence of antibodies, but also their concentration. It can be used to judge both the state of the immune system and the stage of the infectious process: is it in an acute form or is it heading towards recovery. To conduct quantitative tests, developers build on the established antibody norm, which corresponds to different stages.
Indications for research
Frequent indications for immunoglobulin analysis are recurrent and chronic infectious diseases. The study is prescribed for patients with bacterial damage to the respiratory tract - sinusitis, pneumonia, tonsillitis. Also, suspicion of reduced activity of humoral immunity arises with prolonged and frequently recurring otitis, with meningitis, with symptoms of gastrointestinal infections. Immunoglobulin M is used to detect intrauterine infections. In addition, a blood test for immunoglobulins is performed for tumor diseases of the lymphoid system - myeloma, leukemia, lymphoma, reticulosarcoma, as well as for autoimmune diseases and liver pathologies.
The advantage of the analysis is its high information content - the results reflect several parts of the humoral immune response at once: the body’s ability to quickly recognize a foreign agent, the formation of antigenic “memory”, and the activity of protecting the mucous membranes. Sometimes some decrease in indicators is transient and reversible. To differentiate such a deviation from a truly existing violation of the body's anti-infective defense, this study is prescribed together with a test for CEC and phenotyping of lymphocytes.
Preparation for analysis and collection of material
Immunoglobulins are determined in venous blood; sampling is recommended to be done in the morning, before meals. If the procedure is scheduled for another time, then at least 4 hours should pass after eating. The day before the test, you need to avoid alcohol, cancel sports training and other types of intense exercise. 3 hours before donating blood, you must refrain from smoking; the last 30 minutes should be spent in a calm environment. Some medications change the level of immunoglobulins in the blood, so you should tell your doctor about all medications you use. Blood is taken from the cubital vein, stored and transported in tubes with an anticoagulant.
The level of immunoglobulins is examined in the blood serum. Before the analysis procedure, the tubes are placed in a centrifuge, and then clotting factors are removed from the separated plasma. A common research method is immunoturbidimetry. Its essence lies in the fact that antigens are introduced into the serum, which form complexes with immunoglobulins. The density of the test sample increases, which is measured using a photometer; based on the obtained indicators, the level of immunoglobulins is calculated.
Should you always trust test results?
The result largely depends on the set of antigens that the developers used. If the selected antigens are not specific enough, proteins produced in response to other pathogens, such as related coronaviruses that cause the common cold, will latch on to them. In this case, the test gives a false positive result.
There are also false negative results - when a person has antibodies to an antigen that is not presented in the test. For example, this happens with viruses that have been discovered recently, as in the case of SARS-CoV-2. A false negative result can also occur when the blood was taken too early and there are not enough antibodies in it yet.
Normal values
Immunoglobulins G penetrate through the placenta to the fetus, so their level in newborns is high, and during the first year it decreases, as maternal immunoglobulins are replaced with their own. The normal limits depend on the age and gender of the patient.
- in the first month of life – 3.97-17.65 g/l for boys, 3.91-17.37 g/l for girls
- from 1 month to one year – 2.05-9.48 g/l for boys, 2.03-9.34 g/l for girls
- from one year to 2 years – 4.75-12.10 g/l for boys, 4.83-12.26 g/l for girls
- from 2 to 80 years – 5.40-18.22 g/l for boys and men, 5.52-16.31 g/l for girls and women
Immunoglobulins A are unable to cross the placental barrier; in newborns, their concentration in the blood is very low. Self-synthesis of antibodies is fully established by the age of 5 years. The normal values for immunoglobulin A are:
- in the first 3 months of life – 0.01-0.34 g/l
- from 3 months to a year – 0.08-0.91 g/l
- from one year to 12 years – 0.21-2.91 g/l for boys, 0.21-2.82 g/l for girls
- from 12 to 60 years – 0.63-4.84 g/l for boys and men, 0.65-4.21 g/l for girls and women
- after 60 years – 1.01-6.45 g/l for men, 0.69-5.17 g/l for women
Immunoglobulins M have a large molecular weight and do not cross the placenta during pregnancy. In children, the concentration of antibodies increases gradually, reaching adult values by the age of 7-12 years:
- in the first 3 months of life – 0.06-0.21 hl
- from 3 months to one year – 0.17-1.43 g/l for boys, 0.17-1.50 g/l for girls
- from one year to 12 years – 0.41-1.83 g/l for boys, 0.47-2.40 g/l for girls
- after 12 years – 0.22-2.40 g/l for boys and men, 0.33-2.93 g/l for girls and women
A physiological decrease in the level of immunoglobulins can be detected during pregnancy, an increase - during intense physical activity or the experience of strong emotions.
Level up
Immunoglobulins are markers of an infectious process in the body; the most common reason for an increase in their level in the blood is respiratory and gastrointestinal infections. An increase in the concentration of IgG and IgA antibodies is characteristic of chronic processes; the number of IgM antibodies increases in both acute and chronic forms of diseases. Other reasons for increased levels of immunoglobulins include autoimmune pathologies, liver damage, as well as multiple myeloma and other monoclonal gammopathies.
Level reduction
The most common reason for a decrease in immunoglobulin levels is acquired deficiency. The concentration of antibodies decreases when their production is disrupted - with neoplasms of the lymphatic system, lymphoproliferative diseases. In addition, the level of immunoglobulins decreases with their increased breakdown and rapid elimination of protein - during irradiation, the use of drugs (for example, cytostatics), enteropathies, nephropathies and burns. Less commonly, the cause of a decrease in immunoglobulin levels is congenital deficiency. It develops with congenital agammaglobulinemia, ataxia-telangiectasia (IgA), Wiskott-Aldrich syndrome (IgG) and selective IgM deficiency.
full list of articles
How to choose a quality antibody test?
Look at the sensitivity and specificity rates. Sensitivity is the agreement between positive test results and actual diagnoses. Specificity is the ability of a test to detect exactly those antibodies that relate to a specific pathogen. A test that is not sensitive enough may miss some cases, while a test that is not specific enough may suspect the virus in those who do not have it.
According to the results of a recent meta-analysis, the ELISA test, an enzyme-linked immunosorbent test, turned out to be the most reliable in determining antibodies to SARS-CoV-2. Its specificity is 99% and sensitivity is 90–94%. It is done in a laboratory and takes one to two days. The ICA (immunochromatographic) rapid test is less accurate, but it takes about ten minutes. Sensitivity/specificity may be different for different types of antibodies.
It is important to remember that the antibody test does not show the presence of the virus, but only the body’s possible reaction to it. The WHO (World Health Organization) considers the PCR test to be the most accurate and reliable method for diagnosing a viral infection. It allows you to detect the presence of genetic material of the virus in the blood. Remember that in making a final diagnosis, it is not the test that is decisive, but the clinical picture.
Ig G - interpretation of the test for antibodies to coronavirus
To determine class G immunoglobulins in the blood, a qualitative and quantitative method for determining antibodies is used. Below is a table with a breakdown of the enzyme immunoassay for coronavirus (igG indicator for coronavirus).
Coronavirus antibody index - transcript of captions
| Result | Index | Meaning |
| Negative | Less than 0.8 | The patient either did not encounter the disease or underwent the procedure in the acute phase. |
| Border | 0,8-1,1 | You need to do a repeat test after 14 days. Perhaps the test was done at the onset of the disease or during the recovery process. |
| Positive | More than 1.1 | This level of antibodies to coronavirus in adults is normal. The person had coronavirus infection several months ago, and humoral immunity had time to develop. |
Class G antibodies to coronavirus - interpretation of results
An antibody titer to coronavirus of 1,800 (positive result) is normal. In this case, immunoglobulins of class A and M should be absent in the blood. Their presence indicates the stage of recovery.