One of the most common vascular diseases in the modern world is atherosclerosis. Every third resident of our country over the age of 65 suffers from the consequences of cholesterol deposition on the inner walls of the vessels of the heart, brain and limbs, and according to WHO, in developed countries, mortality from diseases caused by atherosclerosis is up to 50% of all cases.
Despite this prevalence, there is no general understanding of the causes of atherosclerosis. This is a complex disease, the study of which uses the latest advances in medical science. Therefore, you should not try to independently diagnose atherosclerosis and self-medicate! The correct diagnosis can only be made by a professional using modern laboratory and instrumental methods.
Diagnosis of atherosclerosis always consists of several main stages:
- studying patient complaints, identifying symptoms of the disease;
- examination of the patient;
- studying the medical history, identifying risk factors associated with the development of the disease;
- The main and most important stage is laboratory and instrumental diagnostic methods.
Clarification of the patient's symptoms and complaints
At the first stage, the doctor compares the patient’s complaints with the symptoms of the disease. Symptoms of atherosclerosis, depending on the location and stage of development of the disease, vary greatly, but a number of common ones can be identified:
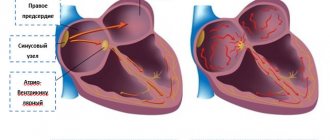
- attacks of angina (pain in the chest, left shoulder, forearm, occurring after physical exertion and stress), arrhythmia. Most often, such symptoms are a sign of atherosclerosis of the heart vessels;
- painful sensations in the limbs , numbness, lameness are signs of atherosclerosis affecting the vessels of the legs and arms;
- headaches, memory and intelligence impairment are symptoms of cerebral atherosclerosis.
Is vascular atherosclerosis visible on MRI of the brain?
Magnetic resonance imaging of intracranial arteries allows us to assess the condition of the walls, lumen, and functionality of the bloodstream. An MRI of the brain with a vascular program will show the following pathological changes:
- narrowing of the artery lumen, impaired blood flow;
- thickening, decreased elasticity of the vascular wall at the site of cholesterol plaque formation;
- foci of ischemia in cerebrovascular accidents;
- artery aneurysm due to deformation of the walls by cholesterol deposits;
- intracranial hematomas formed due to rupture of a vessel;
- violation of the integrity of the arterial wall.
Magnetic resonance scanning is one of the most informative types of instrumental research of the cerebral circulatory system. MRI shows the development of atherosclerosis of cerebral vessels at the stage of slight (from 1 mm) wall thickening.
A non-stenotic process is characterized by the presence of a volumetric compaction without a significant effect on blood flow. In this case, there are no signs of ischemia of the cerebral substance, the disease is asymptomatic.
Cerebral vascular lesions on MRI
When the lumen of the artery narrows by 15-20%, stenosing atherosclerosis is diagnosed. With age, vascular damage intensifies, and signs of insufficient cerebral circulation increase. MRI images of the head show areas of ischemia.
Magnetic resonance scanning of the intracranial space is carried out to assess the state of the circulatory system and brain structures. MR angiography makes it possible to differentiate cerebral atherosclerosis and other vascular pathologies (neoplasms, inflammatory processes, etc.). In some cases, only hardware diagnostics makes it possible to determine the causes of cerebrovascular accidents.
Determination of the ankle-brachial index
The ankle-brachial index (ABI) is an important indicator in the diagnosis of atherosclerotic vascular lesions. This is the ratio of blood pressure in the lower leg to the pressure in the arm. At certain ABI values, a professional physician can detect atherosclerosis of peripheral vessels in the early stages and prevent its development.
At the Center for Pathology of the Circulatory Organs, determining ABI takes no more than 1 minute using the Boso ABI-System 100 system, as well as the Japanese VaSera VS-1000 Fukuda Denshi sphygmomanometer. The procedure is a simultaneous measurement of pressure on the limbs and does not require special preparation of the patient.
For a detailed study of blood vessels, our equipment also measures the speed of propagation of the pulse wave. High speed is a signal to start treatment. This is a characteristic indicator for the development of atherosclerosis.
How to prepare for analysis
Three days before the test, you should avoid fatty foods rich in cholesterol (meat products, especially fatty ones, sausages, sausages, dumplings, etc.)
Blood for analysis for atherosclerosis must be taken strictly on an empty stomach (i.e., at least 8-10 hours must have passed since the last meal).
What does atherosclerosis risk screening consist of?
The essence of this diagnosis is a comprehensive study of the patient’s blood to determine biochemical markers of the development of atherosclerosis.
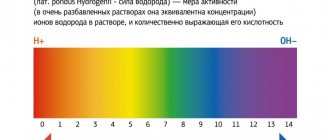
Extremely important indicators in screening are lipidogram or lipid profile data:
- total cholesterol;
- high density lipoproteins (HDL);
- low density lipoproteins (LDL);
- triglycerides (TG).
Cholesterol - the concentration of this substance in the blood is considered one of the most informative indicators of the lipid profile. But cholesterol itself is not found in the body, but is part of lipoproteins - complex compounds of fats and protein.
of lipoproteins - HDL, LDL, VLDL (high, low and very low density lipoproteins).
The last two groups are atherogenic; the cholesterol content in such compounds can reach 45% or higher. These lipoproteins transport cholesterol from the liver to cells, where it is involved in the production of cell membranes.
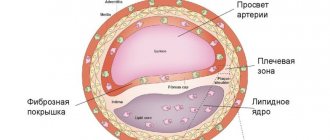
LDL and VLDL cholesterol is a key risk factor for the development of atherosclerosis, since these compounds easily pass into the vessel wall and form an atherosclerotic plaque.
High-density lipoprotein (HDL) has much less cholesterol. And they are able to “take” cholesterol from the walls of blood vessels and other tissues and transport it to the liver for “utilization.” Therefore, HDL cholesterol is considered “healthy” or “good.”
Triglycerides are another form of fat. Their high concentration in the blood can also contribute to the development of atherosclerosis.
In some cases, an extended lipid profile is performed. In addition to the above parameters, it includes:
- lipoprotein(a);
- apolipoprotein A1;
- apolipoprotein B.
Lipoprotein (a), like triglycerides, is a transport form of fat. In composition, it is closest to LDL, and, accordingly, an increased content of this substance in the blood also indicates the risk of developing atherosclerosis.
Apolipoprotein A1 is a protein that is one of the main components of the source of “good” cholesterol - HDL. Normal values of this indicator create optimal conditions for reducing cholesterol in the walls of the arteries.
Apolipoprotein B is the main protein component of LDL and VLDL involved in cholesterol metabolism. This is a key marker in assessing the risk of atherosclerotic lesions of the coronary vessels.
Interpretation of lipid profile results. Normally, total blood cholesterol should be less than 5.0 mmol/l; HDL level be more than 1.2 mmol/l in women and more than 1.0 mmol/l in men; and LDL - less than 3.0 mmol/l in both sexes; The triglyceride content in a healthy person should not exceed 1.7 mmol/l.
Important! The interpretation of the screening results should be carried out by a doctor who will correlate the test results with the individual characteristics of the person (age, weight, gender, existing diseases, medications taken, etc.).
Having studied the diagnostic results, the cardiologist will draw up a conclusion about the individual risks of developing atherosclerosis for the patient, give recommendations for prevention or prescribe additional examination if alarming signs are detected.
Early detection of pathology will allow you to begin the necessary treatment and avoid unwanted health consequences!
Screening for the risk of developing atherosclerosis at MedicCity
- Biochemical blood tests;
- Apolipoprotein A-1;
- Apolipoprotein B;
- Lipoprotein (a) (Lipoprotein (a);
- Triglycerides;
- High-density lipoprotein cholesterol;
- Low-density lipoprotein cholesterol;
- Cholesterol total.
In the laboratory and diagnostic department of our multidisciplinary clinic, you can undergo atherosclerosis risk screening and any other examination at a convenient time, without queues and as quickly as possible. We guarantee the reliability of the results, anonymity, and speed of data processing!
ECG, stress ECG and EchoCG
An ECG is used if coronary heart disease is suspected, the consequence of which is most often atherosclerosis. This is a universal method in cardiology, and no doctor can prescribe treatment without it.
In order to make the heart work in a stressful situation, for example, during physical activity, a stress ECG is used. For this purpose, our center is equipped with a special General Electric bicycle ergometer. Simulating cycling gives the doctor an understanding of how the vessels that supply the heart with blood work during exercise.
Echocardiography (EchoCG) is an informative way to examine the heart and coronary vessels with ultrasound. A diagnostician can assess in real time the nature of wall damage, the presence of blood clots, and the speed of blood flow.
Success in the treatment of atherosclerosis depends entirely on timely diagnosis . Since this disease cannot be cured, the patient needs to monitor his health for the rest of his life, see a doctor and undergo periodic examinations of the vascular system. At the Center for Pathology of the Circulatory Organs, we use only the most modern equipment from European, American and Japanese manufacturers. Our experienced specialists will provide you with all the necessary assistance, prescribe the correct diagnosis and treatment of atherosclerosis.
What does vascular atherosclerosis look like on an MRI image?
As a result of magnetic resonance imaging, the doctor receives monochrome images of thin sections of scanned tissue. The pitch thickness can be adjusted individually (minimum 1 mm). Layer-by-layer images are taken in three projections. Based on the obtained photos, a 3D model of the vascular system of the studied area is reconstructed.
Contrast enhancement used in MR angiography visualizes the structural features of the bloodstream. The advantage of scanning is the ability to assess the condition of the arterial network and surrounding tissues.
Signs of atherosclerosis on MRI images:
- the presence of a characteristic thickening of the inner wall (intima-media complex);
- narrowing of the lumen of the vessel;
- there are no areas of signal loss due to the flow effect (a sign of severe stenosis or occlusion of the artery);
- the presence of cholesterol formation (plaques);
- the effect of “loss of flow” is possible - with stenosis over 95%);
- signs of hemorrhage in case of rupture of the vascular wall;
- symptoms of blood clot formation at the site of the lesion;
- foci of necrosis, tissue ischemia due to impaired blood supply.
Fat-suppressed T1-weighted images show the composition of the cholesterol plaque. The photographs show hemorrhages, a necrotic core, and an increase in the amount of lipids in the thickness of the deposits. Thinning of the fibrous capsule of the plaque is possible (even to the point of rupture). Such formations are called “high risk” deposits.
Arterial stenosis and occlusion on MRI images
Spatial reconstruction of the network of blood vessels in atherosclerosis reflects changes in the lumen and disturbances in blood flow. Three-dimensional images make it possible to assess the localization of pathological deposits, the intensity of the process and the consequences of deterioration of blood circulation in the tissues.
How to determine cholesterol plaques in blood vessels by measuring carotid artery IMT
To determine cholesterol plaques in the carotid artery (which is incomparably easier to reach than the coronary vessels), the patient only needs to lie quietly on the couch for 10 to 12 minutes. The procedure itself boils down to an ultrasound examination of the carotid artery: a special gel is applied to the neck, and the doctor takes about 12 photographs of the right and left arteries from different angles.
The resulting images are processed on a computer. The measurement accuracy is several hundredths of a millimeter. The obtained values are compared with the average statistical values - and from this comparison one can, for example, estimate the age of the circulatory system. The procedure for high blood cholesterol levels should be repeated every 1 to 2 years (to assess changes in plaque size).
Regular observations make it possible to predict the risks of complications and adjust diet and lifestyle to the needs of the cardiovascular system. An alternative to changing IMT in terms of accuracy is only invasive (internal) angiography procedures.
Causes of atherosclerosis
The root cause of the development of atherosclerosis is not fully understood. There is no single theory of the occurrence of this disease. It is believed that the disease develops as a result of genetic disorders, pathological changes in the cells of the vascular walls, autoimmune reactions, viral or chlamydial infections, and hormonal changes. Elevated levels of cholesterol in the blood, especially its atherogenic fraction, significantly contribute to the early development of atherosclerosis.
have been identified that significantly increase the risk of atherosclerosis
:
- bad habits, among which smoking is the most dangerous;
- hereditary predisposition: the presence of the disease in parents, close relatives;
- poor diet with a predominance of fatty foods of animal origin;
- sedentary lifestyle;
- hormonal and metabolic disorders, excess body weight, menopause in women;
- frequent stress;
- hypertonic disease;
- diabetes.
Where do they look for cholesterol plaques in blood vessels?
During the IMT study, cholesterol plaques are looked for in the carotid artery, with angiography - in the coronary vessels of the heart (the procedure is invasive), with computed tomography of the thoracic region - in the coronary vessels (without internal intervention, but using x-rays).
With traditional ultrasound - in blood vessels (possibly the carotid artery). Indirect methods, such as, for example, measuring pressure under load, do not involve searching for atherosclerotic plaques at all, but provide an assessment of indirect signs. This also includes monitoring heart rate after exercise and assessing energy consumption during physical work.
See also:
Is it possible to play sports with vascular atherosclerosis?
How to detect cholesterol plaques yourself
How to detect cholesterol plaques at home? The methods, of course, are not at all effective, because... There are no symptoms of high cholesterol levels in the blood and the presence of atherosclerotic plaques, but if it is not possible to undergo a carotid IMT study, CT coronography or even angiography, you can monitor your condition:
- level of physical endurance (the higher the better);
- amount of fiber consumed (more is better);
- frequency of fish consumption (more is better);
- systolic (upper) pressure (ideal - around 120, and always no more than 140);
- body mass index and excess body fat (less is better, BMI should be no more than 24).
Energy expenditure as a way to independently measure the number of cholesterol plaques
In the gym (gym) or at home, but on sports equipment, you can assess the level of physical fitness by energy expenditure (calorie consumption) during physical exercise. For example, race walking burns about 240 - 300 kcal per hour under normal conditions, if much more is burned, this is already a reason to think about studying the condition of the blood vessels.
The methodology for assessing the level of cholesterol plaques in blood vessels based on measuring the body's energy expenditure is based on the concept of metabolic equivalent (MET). 1 MET corresponds to the amount of oxygen burned that is consumed at rest, lying down.
- 1.5 - 4 MET is spent on work in the garden or around the house.
- For construction and installation work - 4 - 8 MET.
- When jogging (up to 5.4 km/h or 1.5 m/s) and walking uphill (with an incline of no more than 14%) - 8 - 8.3 MET.
- When exercising on a treadmill (depending on speed) – 5 – 18 MET.
The MET scale is used in stress texts. Extremely poor fitness is when a person is unable to reach the 4 MET level of exercise. The norm is considered to be the unimpeded achievement of a value of 10 - 12 METs, 15 is a good result. People who are able to achieve 15 METs almost never perform poorly on IMT.
Monitoring blood pressure is another indirect sign of the level of atherosclerotic plaques
Normal pressure, as indicated above, is 120/80, excellent - 110/70, however, after physical activity, the upper pressure can increase to 150, 160 and even 170. The lower pressure is 10 - 20 points less (in trained people - by 40 or more). Those. a trained person with intense training can have a blood pressure of 170/40! And it will be normal.
If the resting pressure is elevated (between 120/80 and 140/90), then during training the systolic pressure can reach 180 - 200, and the diastolic (lower) pressure can increase by 5 - 9 points or remain unchanged. High blood pressure itself is one of the reasons that accelerates the growth of atherosclerotic plaques. But the conditional norm in the described case will be its value under load up to 190/85.
If the resting pressure exceeds 140/90 mmHg. Art., then under load the systolic pressure can exceed 200, and the diastolic pressure increases by 10 points or more. This causes the blood vessels to contract, which is an undesirable reaction. Blood pressure can reach 200/105.