Cholesterol plaques in the vessels of the neck (carotid artery) are dangerous, primarily because they impede blood supply to the brain. Cholesterol (atherosclerotic) plaques in the vessels of the cervical spine are formed as a result of poor nutrition (abuse of fatty foods and foods rich in exogenous cholesterol) and a sedentary lifestyle (together - metabolic syndrome). Often atherosclerotic plaques in the vessels of the neck are accompanied by the same in the legs (varicose veins) and on the heart.
Cholesterol plaques in the cervical spine are well diagnosed by ultrasound examination of the intima media thickness (IMT) of the carotid artery (more on the diagnosis of high cholesterol). The presence of cholesterol plaques in the carotid artery indicates their accumulation in the blood vessels and other organs and tissues of the body, including the coronary vessels of the heart (which can lead to the development of angina and heart attack) and in the brain (stroke).
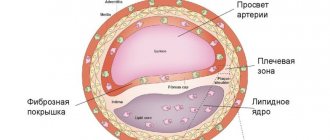
Cholesterol plaques in the neck are formed when there is a high level of low and especially low density lipoproteins (LDL and VLDL) in the blood. In the neck, blood vessels narrow, which facilitates the formation of atherosclerotic deposits here. The resulting plaques can harden over time (atherocalcionosis, calcium accumulation occurs) and burst (if a fresh cholesterol plaque bursts, without calcium, then there is a risk of forming a blood clot - a thrombus).
The main symptoms of cholesterol plaques in the carotid artery are:
- impairment of memory and cognitive functions of the brain;
- headache;
- fatigue and chronic fatigue;
- attacks of dizziness;
- feeling of heaviness in the head;
- deterioration of hearing and vision (including spots before the eyes), speech;
- impaired coordination of movements;
- increased irritability.
Atherosclerosis develops slowly and, as a rule, asymptomatically (there are no symptoms of high cholesterol levels in the blood at all) until a critical mass of atherosclerotic deposits accumulates in the vessels. These symptoms of the formation and accumulation of cholesterol plaques in the carotid artery and vessels of the cervical spine appear only in 60% of observed cases.
The reasons for the formation of atherosclerotic deposits in the blood vessels of the neck are:
- hypertension (high blood pressure) – blood flow acts on the walls of blood vessels like a battering ram, the higher the pressure, the higher the risk of damage to the walls (although hypertension is not the cause of high cholesterol in the blood);
- inflammatory processes in arteries and veins, leading to damage to the endothelium - lipoproteins infiltrate into the appearing “cracks”;
- damage to the vessels of the cervical spine by herpes viruses, cytomegalovirus, microorganisms (for example, chlamydia);
- destruction of blood vessel walls by antioxidants and (or) free radicals;
- obesity and high cholesterol levels in the blood (hypercholesterolemia) – the main building material for atherosclerotic deposits is LDL;
- hormonal disruptions (releases of adrenocorticotropic and gonadotropic hormones, which leads to an increase in the production - synthesis - of endogenous, intrinsic cholesterol).
It should be noted that there are a number of factors that increase the risk that one or more of these causes of cholesterol plaques will lead to their formation. These include physical inactivity (sedentary lifestyle), smoking, alcohol abuse, diabetes, excess weight, high blood pressure, regular stress and emotional stress.
See also:
What kind of alcohol can you drink if you have high cholesterol?
Diet for high sugar and cholesterol
Non-modifiable factors (reasons) for the formation of atherosclerotic deposits in the carotid artery include hereditary predisposition and age.
How is the treatment carried out?
After all the examinations have been carried out and the final diagnosis has been made, the doctor selects a therapeutic course. The first stage is to adjust your lifestyle. It includes giving up harmful habits, dieting and improving physical condition. After this, medications are selected that improve the vascular system and also help the plaques to resolve. Treatment with folk remedies is part of complex therapy, but acts as an auxiliary step.
Return to contents
Drug therapy
With the help of Cardiomagnyl, you can make the patient’s blood more fluid and prevent thrombus formation in the vessels.
In case of carotid artery stenosis, the first step in eliminating the problem is the medicinal method. The following types help to cleanse the vascular system and prevent plaque tearing off:
| Name | Action | A drug |
| Blood thinners | Prevents thickening and blood clots | "Aspirin" |
| "Cardiomagnyl" | ||
| Statins | Normalize lipid levels in the blood and help dissolve plaques | "Atorvastatin" |
| "Cardiostatin" | ||
| Hypotensive | Regulates surges in blood pressure | "Verapamil" |
| "Fosicard" | ||
| "Renipril" | ||
| Painkillers | Eliminate pain | "Paracetamol" |
| "Ibuprofen" |
Return to contents
When is surgery needed?
It is not always possible to remove cholesterol plaques with conservative treatment. In advanced cases, carotid artery blockage may require surgery. To do this, a carotid endarterectomy is performed, which involves making a small incision and removing the growth. The operation is performed in easily accessible places. In case of complications, doctors prescribe angioplasty and stenting, when the artery is artificially expanded with the help of a stent.
Return to contents
Does diet help get rid of atherosclerosis?
With the help of a nutritionist, the patient will be able to put his diet in order and improve his condition.
Removing plaques in the carotid arteries is important for normalizing human health. Treatment of atherosclerosis begins with a review of lifestyle. First of all, the patient is sent to a nutritionist’s office for nutritional correction. Low cholesterol foods are often included. It is recommended to eat vegetables and fruits rich in fiber and steamed fish. Diet and lifestyle make up 80 percent of the entire treatment process, so neglecting this stage is not recommended.
Return to contents
Cleaning blood vessels with folk remedies
Plaques in blood vessels can be overcome using an integrated approach. Alternative medicine is an integral part of any therapy. However, it is recommended that you first confirm all prescriptions with your doctor. This will help avoid unwanted side effects. The principles of traditional therapy include:
- Internal carotid artery (segments according to Bouthillier)
- Hirudotherapy. Thanks to leech saliva, you can influence blood thinning. It also improves well-being, relieves unpleasant clinical manifestations, and the effect of such a procedure lasts for a long period of time.
- Juice therapy. Beetroot juice helps reduce plaque in the arteries of the cervical spine. It is recommended to add it to any drinks, as it helps dissolve lipids.
- Honey. Take 2 tsp. during the day, as it improves the chemical composition of the blood.
If there are allergic reactions to any component, traditional recipes should be reviewed.
Return to contents
Causes of high cholesterol
Approximately 80% of cholesterol in the body is synthesized in the liver, the remaining 20% comes from food. If this balance shifts in one direction or another, an increase in the atherogenic index is possible.
Increased levels of cholesterol in the body are usually associated with the following predisposing factors and circumstances:
- overweight and obesity, with waist size playing a special role, because indirectly reflects the amount of abdominal fat in the body (the norm for this indicator for women is up to 88 cm, and for men – up to 102 cm);
- eating fatty foods - we are talking mainly about animal fats, which are rich in saturated fatty acids (the daily diet should contain up to 15% fat, but most of it should be in the unsaturated fraction - vegetable oils, seafood and fish);
- sedentary lifestyle - the less a person moves, the higher the likelihood of “bad” cholesterol attaching to the walls of blood vessels and an increased risk of atherosclerosis;
- age 50+ - women who have entered menopause are especially at risk, because during reproductive age, estrogens had an additional protective effect on blood vessels, but men are also vulnerable, so prevention is important for both sexes;
- complicated heredity - if immediate relatives suffered from atherosclerosis or early strokes/heart attacks, you should regularly check the level of cholesterol in the blood and, if the concentration is elevated, even in the absence of clinical signs, follow a diet and more;
- smoking (passive and active) – the vascular wall is damaged by both nicotine and combustion products.
Obviously, age and heredity cannot be influenced - these are non-modifiable risk factors. However, all the others can be influenced to reduce their adverse effects to a minimum. This is what prevention is all about. Proper nutrition, quitting smoking and physical activity (at least 30 minutes of walking a day) will help blood vessels function normally.
Symptoms
Carrying out complex diagnostic measures to determine plaques in the carotid artery (atherosclerosis) is based on medical history and patient complaints. In the early stages of the disease, symptoms may be mild or similar to other pathologies. That is why the patient himself and even the attending physician may not realize that atherosclerosis is developing until the blood supply to the brain is significantly impaired.
The following symptoms are characteristic of oxygen deficiency in brain tissue:
- migraine;
- insomnia;
- decreased performance;
- memory problems;
- speech disorders;
- difficulty concentrating;
- feeling of heaviness in the head, as if you have a cold;
- noise in ears;
- sudden darkening of the eyes;
- increased physical and mental fatigue.
Precursors of a stroke may include sudden weakness or numbness, usually on one side of the body, slurred speech, poor coordination, and sudden blindness in one eye. If any of these symptoms occur, you should consult a doctor immediately. This condition is called a transient ischemic attack and can last from several tens of minutes to a day. The most dangerous consequence of TIA, which occurs as a result of a significant decrease in the lumen of the carotid artery, rupture of an atherosclerotic plaque in the carotid artery and blockade of small vessels or blood flow, can be a stroke. More extensive brain damage has the risk of becoming irreversible.
Complications
The most serious complication of carotid atherosclerosis is stroke. The increased risk of stroke in patients with carotid artery disease is due to the following factors:
- Decreased blood flow. Carotid arteries with atherosclerosis often narrow to such an extent that they do not provide sufficient blood flow to the brain.
- Plaque rupture. There is a risk that part of the plaque will break off and penetrate the small arteries of the brain (cerebral arteries). A fragment lodged in one of these small arteries will block it. This will impede blood flow to the area of the brain that is supplied by this artery.
- Thrombosis. Some plaques are prone to cracking and forming an uneven surface on the artery wall. The body reacts to these changes as if it were damaged and sends platelets to this place - blood cells that participate in the process of blood clotting. A blood clot may form that is large enough to block or slow blood flow through the carotid or cerebral artery, causing a stroke.
A stroke causes permanent brain damage and muscle weakness, and in severe cases, death.
Removal of cholesterol plaques in the carotid artery
Removal of cholesterol plaques on the carotid artery at the second stage (fibrosis) and at the third stage (calcionosis) can occur in several ways:
- increasing blood (arterial) pressure - but this path is fraught with the formation of new damage to blood vessels and, as a consequence, the formation of new atherosclerotic deposits;
- dilatation of blood vessels, however, this method is ineffective on the carotid artery and is used more often for varicose veins of the extremities;
- increased tone of blood vessels;
- cleansing the blood of cholesterol - however, this method does not so much destroy existing plaques as prevent the formation of new ones.
The cost of removing cholesterol plaques on the carotid artery using medications is entirely determined by the cost of the drugs used. The cost of surgical treatment (carotid endarterectomy, angioplasty, stenting) is even higher if it is not done according to the insurance policy. Surgical treatment is resorted to when conservative methods fail.
Conservative methods of removing cholesterol plaques include taking specialized medications, increasing the proportion of foods in the diet that cleanse blood vessels of cholesterol, performing (daily) therapeutic exercises for atherosclerosis, and taking statins or other medications for high cholesterol.
How to remove cholesterol plaques from the carotid artery safely? Surgery has some risks, and drug treatment has contraindications and side effects. Drug treatment can be aimed at reducing the level of cholesterol synthesis by the liver, increasing energy metabolism in cells - this is how it is possible to remove excess cholesterol from the blood and carotid arteries. An alternative is infusions and herbs for cholesterol plaques, but their effectiveness remains unproven.
Diagnostic methods
- Medical checkup. A “whooshing” sound (murmur) above the carotid artery in the neck when auscultated indicates a narrowing of the carotid artery. Your doctor will examine your physical and mental health, such as muscle strength, memory, and speech function. To begin treatment for arterial stenosis, one examination is not enough: instrumental examination methods will help to assess the condition.
- Ultrasonography. A non-invasive method for detecting atherosclerosis of the carotid arteries is Doppler ultrasound. This test evaluates blood flow, pressure, and constriction of a blood vessel by recording high-frequency sound waves (ultrasound) bouncing off red blood cells.
- Computed tomographic angiography (CTA). This imaging test uses a contrast agent to highlight the carotid arteries in the images. A contrast agent is injected into a blood vessel. Once it enters the carotid arteries, a computed tomography (CT) scanner takes X-rays of the neck and brain from different viewing angles.
- Computed tomography (CT) of the head. This imaging method allows you to examine brain tissue without the introduction of contrast agents and exclude the presence of bleeding and other disorders.
- Magnetic resonance angiography (MRA). Like CTA, this imaging test uses a contrast agent (without iodine) to highlight the arteries in the neck and brain. A magnetic field and radio waves are used to create three-dimensional cross-sectional images.
- Magnetic resonance imaging (MRI). This imaging technique looks at brain tissue to help detect early signs of stroke or other problems.
- Angiography of cerebral vessels. This traditional invasive method is rarely used because this examination increases the risk of stroke. As with cardiac angiography, during the procedure a contrast agent is injected using a catheter placed directly into the carotid arteries. Then x-rays are taken.
Risk factors
There are also risk groups. In patients belonging to at least one of them, the risk of developing vascular atherosclerosis is significantly higher. Risk factors are:
- Anatomy. Common carotid artery
- Age. The older a person gets, the lower the elasticity of blood vessels due to low collagen production.
- Increased blood pressure. Excessive pressure on the walls of blood vessels can lead to microtrauma and decreased elasticity.
- Diabetes. With this disease, the body's ability to break down LDL and glucose is significantly reduced.
- Unfavorable heredity. The risk of deposition of cholesterol plaques in blood vessels increases if relatives have had cases of atherosclerosis or coronary heart disease.
The reason for regular monitoring by a specialist is belonging to a risk group and exposure to several provoking factors at once. Otherwise, there is a high risk of critical conditions.
Anesthesia during surgery
In the preoperative room, the patient is fitted with a urinary catheter, an intravenous catheter, and a monitor is connected to monitor the ECG during the operation.
In our clinic, for carotid endarterectomy, local anesthesia with a weak solution of lidocaine is most often used, but with the mandatory supervision of an anesthesiologist. Local anesthesia has enormous advantages over anesthesia in terms of preventing cerebral complications. Local anesthesia provides good pain relief throughout the operation.
A conscious patient is the best neurological monitor. To ensure the safety of carotid endarterectomy, it is necessary to understand how the brain responds to temporary compression of the carotid artery. For this we use local anesthesia. After identifying the carotid bifurcation, we temporarily clamp it, but maintain contact with the patient and give him a number of tasks. If the patient understands and performs the tasks well, then we perform the operation without using a temporary shunt. If we notice that the patient begins to “float away,” we use a special tube to perform the operation under a temporary shunt. Blood flows through this tube during clamping.
How does atherosclerosis develop?
In a healthy body, blood circulates freely through the arteries, delivering oxygen and nutrients to all parts of the body. When the amount of cholesterol exceeds the norm, it begins to deposit on the inside of blood vessels, thereby forming an atherosclerotic plaque.
It is a mixture of fats and calcium. Gradually, the plaque loses its strength and defects form on it. Over time, platelets and blood proteins accumulate at the site of injury, a mixture of which is commonly called a blood clot. It complicates the course of the disease and poses a serious threat to life because:
- further narrows the lumen of the artery;
- a thrombus or part of it can break away from the plaque and, with the flow of blood, clog the vessel at the point of its greatest narrowing.
As a result of this pathological process, a stroke can develop, because blockage of blood vessels leads to a cessation of blood supply.
The formation of atherosclerotic plaque in blood vessels and arteries goes through 3 main stages:
- Lipoidosis. Formation of lipid stripes and spots on the vascular wall. They are small in size, no more than 1.5 mm, and outwardly look like yellowish spots. Over time, their size increases due to the fact that the spots merge. Following this, lipid strips are formed, which rise slightly above the surface of the cells.
- Liposclerosis. The appearance of a fibrous plaque. At the sites of lipid deposits, connective tissue with a lipid core in the center is formed.
- Formation of a full-fledged atherosclerotic plaque. As the disease progresses, the lipid core increases by more than 30% of the total plaque volume.
By nature, stable and unstable atherosclerotic plaques are distinguished. This condition depends on the size, configuration and structure of such a lipid formation. Stable plaques are static or characterized by slow growth. They are mainly composed of collagen, while unstable ones are rich in lipids. Cholesterol plaques, forming in various parts of the vessels, cause circulatory disorders of two types: acute and chronic.
Acute circulatory disorders develop as a result of a sudden cessation of blood flow in an artery. This happens when the contents of the plaque breaks into the lumen of the vessel, and then thrombosis occurs. The detached blood clot eventually reaches narrower vessels, through which it can no longer pass and gets stuck there. This condition is fraught with ischemic stroke.
Chronic circulatory disorders are recurrent in nature and manifest themselves in the fact that the vessels affected by sclerotic and degenerative processes narrow significantly, but do not completely overlap. As a result, cerebral circulation is disrupted. It should be noted that the blood vessels of the brain are very vulnerable to blockage. This is due to the peculiarity of their anatomical structure.
How is the operation performed?
After anesthesia, a 5-10 cm long incision is made along the inner edge of the sternocleidomastoid muscle. The internal, common and external carotid arteries are isolated from the surrounding tissues and rise onto the supports.
During the operation, we perform a test with temporary clamping of the lumen for 3 minutes. The patient is asked to count to 100, shake hands, and move a leg. If there are no signs of circulatory failure in the brain, then we open the vessel and perform an endarterectomy. Otherwise, a special temporary shunt is installed in the lumen.
After arteriotomy, endarterectomy is performed - removal of the atherosclerotic plaque. The removal method may vary. With a longitudinal section, the atherosclerotic plaque peels off from the outer wall of the vessel. With the eversion technique, the internal carotid artery is divided transversely, after which it is everted, and the hard plaque moves away from the wall and comes off. After removal of the atherosclerotic plaque, the vessels are sutured. After a longitudinal dissection, to expand the lumen of the vessel, it is necessary to sew a special patch into the incision, but with the eversion endarterectomy technique, a patch is not required.
After starting the reconstructed artery, ultrasound monitoring of blood flow is mandatory. After this, the wound on the neck is closed with stitches after eliminating all possible bleeding. The skin is closed with an absorbable suture that will not need to be removed. Additionally, to control bleeding, a drainage tube with a bulb is installed, which is removed the next day.