© Author: Sazykina Oksana Yuryevna, cardiologist, especially for SosudInfo.ru (about the authors)
Counting the pulse in the neck in the area of the carotid artery is the fastest and most easily accessible method that allows you to suspect clinical death in an unconscious person and begin timely measures to resuscitate the victim. In other words, the presence of a pulse in the carotid artery indicates that the person is alive. That is why a medical worker of any specialty, and just an ordinary person, should know how to quickly feel the carotid artery.
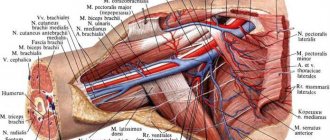
Anatomy of the carotid artery
The carotid artery, along some of its length, is adjacent rather superficially to the skin, so it can be easily and quickly palpated, and thus assess the presence or absence of cardiac activity in a person. This technique allows you to avoid wasting valuable resuscitation time trying to get to the chest and listen to heartbeats on the anterior chest wall.
So, the carotid artery is a paired blood vessel originating directly from the aorta on the left (more precisely, from its arch), and from the truncus brachiocephalicus on the right (brachiocephalic trunk). On both sides, the carotid artery, at this length called the common carotid artery, heading upward, passes to the right and left of the esophagus and trachea, and also slightly anterior to the cervical vertebrae.
Closer to the upper surface of the thyroid cartilage of the larynx (the most protruding part of the larynx, also called the “Adam's apple”), the common carotid artery divides into two branches - external and internal. From this level, the external branch is accessible to palpation, since it is covered only by the skin, subcutaneous fat and fascia, in contrast to the internal branch, which extends into the thickness of the muscles. It is on the external carotid artery that you can feel the pulsation by lightly pressing it against the deeper muscles of the neck.
anatomy of the carotid arteries and cervical arteries
1
Technology for rapid assessment of the condition of victims in a state of clinical death and coma
In cases where the victim is unconscious, it is necessary to immediately begin determining the pulse in the carotid artery. You should not waste time identifying signs of breathing. Signs of breathing are often subtle. Even if a volunteer takes a breath of artificial ventilation (ALV) while maintaining breathing, this cannot harm the victim in any way. A real threat to life can arise only in two cases: 1. The rescuer’s chest is significantly larger in volume (2-3 times) than the victim’s chest (for example, a child under 5 years old). 2. The ventilation was inhaled at the moment of pressing chest compressions on the victim’s chest.
To identify signs of clinical death or the development of coma in an unconscious victim, it is enough to verify the absence or presence of a pulse in the carotid artery.
Pressing your fingers on the neck in the area of the carotid artery causes very severe pain.
If the unconscious victim does not respond to this painful effect, and he has a pulse in the carotid artery, then this means that he is alive and in a state of coma. In this case, he should be immediately turned onto his stomach. At any second he could choke on vomit or choke on his tongue.
If the victim is unconscious and has no pulse in the carotid artery and there are no signs of biological death, this means that he is in a state of clinical death. It is necessary to begin resuscitation immediately.
When using this tactic to identify signs of clinical death or the development of coma, there is no need to waste time on:
- Questions like: are you okay?
- “braking” the shoulder or putting pressure on pain points;
- detecting signs of breathing.
Signs of breathing are elusive and very often deceptive, which can lead to tragic mistakes. For example, fogging of a shiny object brought to the mouth of a deceased person can be observed several hours after the onset of biological death. Finding out why the villi move around the mouth of the deceased can take hours. Looking for the rise of the chest in men with abdominal breathing, and even in winter in outerwear, is a waste, or rather, a fatal waste of time when every second counts.
If we take into account that artificial respiration inhalation (AI) under no circumstances can cause any harm to an adult, then determining the signs of breathing can be considered doing more harm than good in situations of coma or clinical death. In the case of a coma, a victim lying on his back may choke on vomit at any second, and if clinical death develops, the chance to save him will be missed.
Thus, in order to make the most of all the chances of saving victims in a state of coma or clinical death, it is enough to ensure only the absence of consciousness and the presence or absence of a pulse in the carotid artery. It is the presence or absence of a pulse in the carotid artery that makes it possible to differentiate coma from clinical death.
Without determining the pulse in the carotid artery, it is practically impossible to distinguish the state of coma from clinical death! Focusing only on identifying signs of breathing is a fatal mistake.
Considering that sudden death in front of an eyewitness is extremely rare, and fainting and coma are tens of thousands of times more common (approximately 1:10,000), then when doubt arises about the presence of a pulse in the carotid artery, you should immediately turn the victim onto his stomach.
To begin resuscitation of victims and patients in a coma with diabetes mellitus, alcohol poisoning and strokes, traumatic brain injury, including concussion (the most common sports and household traumatic brain injury) is 100% murder! Incorrect resuscitation of a comatose victim lying on his back and pressing on the sternum with a frequency of up to a hundred times per minute will certainly lead to death in a matter of minutes from vomit entering the respiratory tract and suffocation with one’s own tongue.
2
EXAMPLE
USING TECHNOLOGY for rapid assessment of the condition of victims in a state of clinical death and coma
CONCLUSION 1 Determining the pulse in the carotid artery will allow a volunteer to distinguish a coma from clinical death within 10-15 seconds, without unnecessary loss of time, and save many people who find themselves in extremely critical condition.
CONCLUSION 2 Without determining the pulse on the carotid artery, it is practically impossible to distinguish the state of coma from clinical death! Focusing only on identifying signs of breathing is a fatal mistake. Considering that sudden death in front of an eyewitness is extremely rare, and fainting and coma are tens of thousands of times more common (approximately 1:10,000), then when doubt arises about the presence of a pulse in the carotid artery, you should immediately turn the victim onto his stomach.
CONCLUSION 3 Start resuscitation of victims and patients in a coma with diabetes mellitus, alcohol poisoning and strokes, traumatic brain injury, including concussion (the most common sports and household traumatic brain injury) - this is 100% murder! A victim lying on his back, and even under pressure on the lower third of the sternum up to a hundred times a minute, will certainly choke on his tongue and choke on vomit, which will certainly lead to death in a matter of minutes.
19
| GRADE |
Remote detection of wounds, signs of damage to bones and joints
First you should pay attention to the posture of the victim and the position of his limbs:
- frog pose is a sign of damage to the pelvic bones and hip joints;
- unnatural position of a limb or its deformation - fracture of the bones of the limb;
- the presence of a wound with bone fragments protruding from it is a sign of an open fracture.
If the wounded person is conscious, then any complaints of pain in the extremities should raise suspicion of bone damage. At the slightest suspicion of damage to bones and joints, give the wounded painkillers and, if necessary, apply transport splints.
What is important is not the speed of identifying wounds and damage, but the careful attitude towards the victim. The main thing is to protect him from unnecessary pain and injury. Prevention of the development of traumatic shock and its complications begins with a gentle examination of the victim.
To do this, you should avoid palpating the head, neck, chest, abdomen, pelvic bones, arms and legs in order to make a diagnosis: “crunches-not-crunches”, “hurts-not-hurts”. There is no need to mention how the slightest displacement of the temporal bones, fragments of ribs or pelvic and femur bones can result. Such an examination can only be carried out by medical personnel, after mandatory practical training under the supervision of specialists. Any careless touch to the damaged area can be fatal.
For people without medical education (volunteers), it is enough to suspect the presence of a particular injury and act on the principle of overdiagnosis. A neck brace, a forearm splint, an ankle splint, or a pad placed under the knees will never be superfluous.
| GRADE |
EXAMPLE remote detection of wounds, signs of damage to bones and joints
CONCLUSION 1 The use of examining victims by palpation should be excluded from mass training of volunteers in first aid skills, as a technique that leads to unnecessary traumatization of victims and poses a threat to their lives
CONCLUSION 2 Remote detection of the presence of wounds, signs of damage to bones and joints (hyper-diagnosis) is one of the factors in preventing the development of traumatic shock.
How to determine the pulse in the carotid artery?
The technique for determining the pulse consists of the following manipulations. Before palpation begins, it is necessary to free the neck from clothing and visually determine the area of the carotid triangle, the edges of which are the lower jaw, the midline of the neck and the sternocleidomastoid muscle. In this case, it is better to turn the victim’s head in the opposite direction. The side of palpation does not matter, and palpation can be carried out both on the right and on the left. In order to feel the pulse, you need to place two or three fingers (II, III and IV) at the point between the angle of the lower jaw and the anterior surface of the sternocleidomastoid muscle. Next, when pulsation is detected, the main characteristics of the pulse are assessed - rhythm, filling, tension, and the pulse rate per minute is calculated.
Pulse assessment along the entire length of the carotid artery on both sides is used in patients with suspected thrombosis, atherosclerosis, carotid aneurysm, as well as in cases of suspected heart disease such as aortic insufficiency. In the latter case, rhythmic pulsation in the area of the carotid artery is visually noticeable and is called carotid dancing.
In a person who has suddenly lost consciousness, checking the carotid pulse is necessary to determine whether cardiac arrest has occurred and whether immediate resuscitation is required. In this case, the pulse in the carotid artery is not detected on both sides.
What is a normal heart rate?
For a person over 18 years of age, the normal resting heart rate is between 60 and 100 beats per minute
. The more trained the cardiovascular system is, the fewer heartbeats are required for the body to receive the necessary nutrients and oxygen from the blood. Professional athletes have a resting heart rate of about 40 beats per minute. A normal resting heart rate is considered to be: - For a newborn - 120-160 beats per minute, - For a baby from 1 month to a year - 80-140 beats per minute, - For a child aged 2 to 6 years - 75-120 beats per minute minute, - For a child aged 7 to 12 years - 75-110 beats per minute, - For people over 18 years old - 60-100 beats per minute, - For adult athletes - 40-60 beats per minute.
Absence of carotid pulse
A situation where a person has no consciousness and no pulse in the carotid artery indicates that the person has had a decrease in blood pressure to 0 mmHg due to cardiac arrest. Further actions in this case consist of immediately performing cardiopulmonary resuscitation (CPR) according to the ABC protocol - A (Airway) - ensure airway patency, B (Breathing) - start artificial respiration, C - (Circulation) - start chest compressions. It is necessary to carry out artificial respiration and cardiac massage at a rhythm of 2:15 until blood flow is restored and a pulse appears in the carotid artery or until rescuers (medics) arrive, or within 30 minutes from the heartbeat stopping.
Figure: performing cardiopulmonary resuscitation in the absence of a pulse in the carotid artery
What affects heart rate?
The heart rate is influenced by several factors: - training, - ambient temperature, - body position (standing, sitting, lying), - emotional state: excitement, anger, fear, anxiety lead to an increase in heart rate, - excess weight, - intake medications, alcohol or smoking. If an untrained person's heart beats too slowly - less than 60 beats per minute - this is called bradycardia
.
If, at rest, in an untrained adult, the heart beats faster than 100 beats per minute - this is called tachycardia
.
If you experience similar symptoms, which are accompanied by dizziness, shortness of breath or fainting, consult a doctor immediately
.
Causes of other deviations from the norm
Feeling the pulse in the carotid artery can reveal many hidden diseases that have not yet been diagnosed in the patient. But for this it is necessary to palpate the external carotid artery along its entire length, and not just at the angle of the lower jaw. For this technique, it is necessary to line up all four fingers of the hand, except the thumb, between the trachea and the sternocleidomastoid muscle. After palpating one area, the fingers are smoothly moved upward to examine another area.
carotid artery stenosis due to atherosclerosis
Thus, with stenotic narrowing of the lumen of the carotid artery caused by an atherosclerotic plaque, the pulse becomes tense (that is, it is difficult for the doctor to compress the artery until the pulse completely disappears), and the artery itself can be palpated as a lumpy, compacted formation.
A low (not full) and soft (not tense) pulse in the carotid artery on both sides may indicate the patient is developing acute myocardial infarction or myocarditis. A thread-like pulse is detected in cases of severe myocardial damage and is a sign that cardiac arrest may occur at any time.
With a carotid artery aneurysm, you can feel a pulsating round formation, characterized by a high-fill pulse, that is, a high “height” of pulse fluctuations.
With hypertension, with vegetative-vascular dystonia of the hypertensive type, as well as with hyperfunction of the thyroid gland, the pulse in the carotid artery becomes frequent, full (high filling) and tense.
What is maximum heart rate?
This indicator tells you how many beats per minute your heart can make maximum - during physical activity. When playing sports, it allows you to evaluate how intense the load you are receiving. Typically, the maximum heart rate is calculated using a mathematical formula that takes into account the person’s age. For adult men, MHR = 220 – age
. That is, a 25-year-old man would have a maximum heart rate of 195 beats per minute. For adult women, the calculation is the same, but sometimes an adjusted formula is used: MHR = 226 – age. That is, for a 25-year-old woman this figure will be 201 beats per minute.
Tags:
- Workout
- Pulse
- Diagnostics