Acute cardiovascular failure (ACF) is a severe disorder in which the heart and blood vessels are unable to maintain adequate blood flow.
A malfunction occurs in the metabolic processes that ensure the movement of blood, disturbances in the functioning of organs and tissues develop , and if treatment is not started, this pathological process will end in death.
Vascular insufficiency practically does not occur without disturbances in the functioning of the heart and is a disorder that develops with a rapid reduction in the amount of blood in the vessels due to extensive blood loss, disruptions in the tone of the vascular walls, and pathologies in the contraction of the heart muscle.
Under certain conditions, vascular and heart failure can develop in any person. To help, it is important to know the features and types of vascular insufficiency, the causes: clinic, first aid, initial symptoms - information that can save lives.
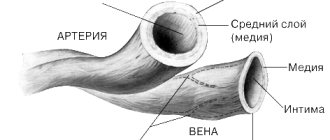
Connection between the vascular and cardiac systems
To know what cardiovascular failure is, you need to understand the mechanism of interaction between the heart and blood vessels.
The heart normally functions as a pump that pumps blood using the capabilities of the heart muscle - the myocardium.
Arterioles, the smallest arteries, transport oxygen to tissues and can change the direction of blood through a spasmodic contraction: the tissues will not receive enough oxygen, and the blood will be directed into the vessels.
If the vascular lumen increases due to the tone of the arteriole walls, blood circulation accelerates.
There are mechanisms that regulate tone:
- The impact of an impulse sent by the nervous system;
- Hormones produced by the adrenal glands (norepinephrine, adrenaline), and others (serotonin, angiotensin II);
- Substances arising from oxidative reactions.
Connection between the vascular and cardiac systems
These mechanisms begin to work in stressful situations, when most of the blood passes into the peripheral vessels. Some toxic substances and medications also change the tone.
Capillaries, which are even smaller vessels, transport blood cells and remove waste products. About 12% of blood is contained in them. If the tone in the vessels is weakened, the amount of blood in the capillaries will increase.
The bulk of the blood is concentrated in the veins, which adapt to changes in blood levels.
Venous pressure controls the flow of blood into the right atrium and increases when:
- Heart failure;
- The presence of an obstruction in the pulmonary artery (blockage by a blood clot);
- Excessive fluid content.
Decreases when:
- Intense blood loss;
- Reducing the tone of the walls of peripheral vessels;
- A sharp decrease in the amount of fluid with diarrhea and vomiting.
Excessive vascular tone in the periphery greatly increases the load on the heart muscle, which requires more effort to pump blood.
If the capillary tone decreases, the bulk of the blood is retained and a sufficient amount does not flow to the heart, which leads to oxygen starvation of the myocardium.
Stages
Classification by severity is based on assessment of peripheral circulation:
- class I (group A, “warm and dry”);
- class II (group B, “warm and humid”);
- class III (group L, “cold and dry”);
- class IV (group C, “cold and wet”).
Depending on the radiological signs and manifestations of acute heart failure (Killip classification), the following are distinguished:
- class I – without manifestations of signs of heart failure;
- class II - moist rales in the lower parts of the lungs, symptoms of pulmonary circulation disorders;
- class III - moist rales in the lungs, pronounced signs of pulmonary edema;
- class IV – cardiogenic shock, peripheral vasoconstriction, impaired renal excretory function, hypotension.
The Killipp classification was developed to assess the condition of patients with acute heart failure that developed against the background of myocardial infarction, but can also be used for other types of pathology.
Causes of acute cardiac
The development of pathology is influenced by various factors, including ischemia, hypertension, intoxication, and heart defects. Typically, deficiency develops due to a combination of several factors and the lack of proper treatment for precipitating diseases.
| Name | Description |
| Cardiac ischemia | It occurs when there is a disruption in the blood supply to the heart arteries, accompanied by a decrease in the strength of the heart muscle due to lack of blood flow, and without treatment leads to acute cardiovascular failure. |
| Hypertension | With hypertension, resistance increases at the periphery of blood vessels, which causes the myocardium to function more actively. This gradually leads to an increase in the thickness of the left ventricular myocardium and a decrease in myocardial strength. |
| Cardiomyopathy | Thickening of the walls of one of the ventricles develops for various reasons, including infections, genetics, myocarditis, intoxication, and hormonal imbalance. Against the background of this pathology, many heart diseases develop, including heart failure. |
| Blockage of pulmonary artery embolus | With PE (pulmonary embolism), the heart begins to experience an intense lack of oxygen, which undermines its functioning and leads to the development of acute failure. |
| Myocarditis | An inflammatory disease of the myocardium, accompanied by the development of a number of complications. Occurs under the influence of viral, fungal, bacterial and parasitic infections. Acute myocarditis, which occurs in severe form, often causes the development of heart failure. |
| Chronic intoxication | Toxic substances that gradually accumulate in the body during chronic intoxication negatively affect the functions of the heart and blood vessels, worsen vascular tone and myocardial activity. Acute intoxication can also provoke OSSN. |
| Myocardial infarction | Damaged areas of the myocardium become scarred, the heart muscle loses flexibility, elasticity and performs its functions worse. |
| Aortic aneurysm | A dangerous pathology in which there is a risk of aortic rupture. If this happens, massive blood loss will trigger the development of CHF. |
| Arrhythmia | Severe arrhythmias gradually worsen the functioning of the myocardium, and after a while, OSHF manifests itself. |
| Heart defects | Defects in various cardiac mechanisms over time lead to chronic or acute failure. |
| Alcoholism | Long-term exposure to alcohol on the body leads to a deterioration in the tone of the vascular walls, weakening of the myocardium and other cardiac mechanisms, and affects the development of other provoking diseases (hypertension, encephalopathy). |
| Intense stress and depression | Long-term severe depression increases the likelihood of developing deficiency by 40%. Stress also disrupts the functioning of the heart, as it creates an increased load on it due to the excessive release of adrenaline. |
| Taking certain medications | Some drugs can aggravate existing heart pathologies, especially when self-medicated and uncontrolled. These include certain antibiotics, potassium, muscle relaxants, and tranquilizers. |
In addition to these reasons, cardiovascular failure develops with skull injuries, intense bleeding, burns with a large area of damage, dehydration, acute allergic reactions, and hormonal imbalances.
Forecast
With cardiogenic shock, the mortality rate reaches 80%.
The five-year survival rate for patients who have suffered acute heart failure is 50%.
The long-term prognosis depends on the presence of concomitant diseases, the severity of heart failure, the effectiveness of the treatment used, the general condition of the patient, his lifestyle, etc.
Timely and adequate treatment of pathology in the early stages gives positive results and provides a favorable prognosis.
If heart failure appears first
Symptoms depend on what pathology—cardiac or vascular—is underlying.
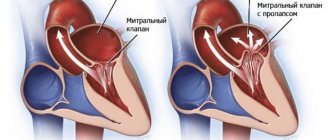
Heart failure is divided into two types:
- Left ventricular failure;
- Right ventricular failure.
Left ventricular failure is a disorder in which the left ventricle is unable to pump the required amount of blood into the vessels.
Develops in the following myocardial diseases:
- Mitral valve prolapse;
- Mitral-aortic disease;
- Arterial hypertension;
- Atherosclerotic lesion of the heart arteries;
- Benign or malignant neoplasms.
Also, acute left ventricular failure often occurs during myocardial infarction or several days after it.
Symptoms increase rapidly:
- Irregularities in heart rhythm;
- Pain in the chest, similar to pain during myocardial infarction;
- Nausea;
- Vomit;
- Respiratory failure: rapid breathing due to lack of oxygen;
- The breathing rate doubles;
- Bronchial whistling is felt when breathing;
- Breath gurgling, bubbling;
- Intense, painful cough;
- When coughing, foamy, pink sputum is produced;
- Blood pressure drops;
- The skin is pale;
- The fingertips become bluish;
- The nasolabial triangle becomes bluish;
- Intense sweating, cold and sticky sweat;
- Marked feeling of weakness;
- Fainting.
If vascular tone is maintained, then blood pressure does not fall, and this is a positive sign: the chances of survival increase. If there is a violation of vascular tone, then it is difficult to eliminate pulmonary edema and restore normal breathing.
Right ventricular failure is a disorder in which the right ventricle is unable to push the required volume of blood into the pulmonary artery.
Develops with:
- Myocardial infarction involving the right ventricular zone;
- Pulmonary embolism or PE;
- Excessive intravenous fluids.
Signs:
- Rapid breathing;
- Feeling short of air;
- Cyanotic skin;
- Swelling of the veins in the neck;
- Swelling of the lower extremities;
- Frequent, weakly palpable pulse;
- Irregularities in heart rhythm;
- Pain in the liver area;
- Enlarged liver, pain when palpated;
- Pressure on the liver area increases the swelling of the veins in the neck;
- Accumulation of ascites fluid in the abdominal cavity.
Heart failure
Also, acute symptoms are characterized by dizziness and a decrease in body temperature.
Chronic form
It should be noted that there are no obvious signs of decompensated chronic insufficiency. Each of the symptoms may indicate that the patient has some other disease.
Usually the pathology is characterized by the occurrence of:
- shortness of breath at any time of the day, even without physical exertion;
- loss of strength;
- edema that affects the limbs, scrotum;
- increase in weight and abdominal volume of the patient;
- increased pressure in the jugular vein;
- pathological noise in the lungs;
- heart contraction disorders;
- decreased diuresis;
- lowering the temperature of the hands and feet.
Often the painful condition is preceded by myocardial pathology or heart failure.
The occurrence of even one symptom inherent in pathology requires immediate contact with a cardiologist, who will prescribe an additional examination.
This type of decompensation can also be right or left ventricular, the symptoms of which are identical.
It is possible that a mixed form of the disease may occur with damage to both ventricles.
If vascular insufficiency appears first
It develops if the tone of the vascular walls is disrupted under the influence of hormones and nerve impulses. The cause of the tone disturbance is a malfunction in the systems of the vasomotor center, which is located in the medulla oblongata, as well as in the areas where the vascular receptors are located.
Due to the deterioration of vascular tone, the movement of blood slows down and it accumulates in the vessels located in the abdominal cavity. A large volume of blood is retained in the hepatic vein and spleen, and the heart ceases to receive it in sufficient volume.
When the tone of the vascular walls is disturbed, three key conditions develop: loss of consciousness, shock and collapse, and their intensity depends on the severity of vascular insufficiency.
Loss of consciousness develops due to a lack of blood circulating in the brain. People with increased nervous excitability and a tendency to arterial hypotension are susceptible to it.
Signs of fainting:
- Sharp pallor of the skin;
- The appearance of cold sweat;
- Weak pulse;
- Heart rate is either fast or slow;
- Reflexes disappear or are not intense;
- Arterial hypotension;
- The pupils narrow.
Loss of consciousness does not last long: less than a minute. If fainting lasts more than 5-6 minutes, convulsions occur and urine is released involuntarily.
Consciousness will be restored if you lay the person so that his head is below the level of the body (place pillows under the main part of the body and lower his head).
Collapse is a dangerous condition in which blood pressure drops sharply and internal organs are not fully saturated with blood.
Signs:
- Feeling weak;
- Retardation of consciousness;
- Pallor of the skin;
- Drop in blood pressure;
- Cold sweat.
Shock is an acute condition that occurs upon contact with extremely dangerous irritants and is accompanied by the rapid development of a number of functional disorders affecting most of the body's systems.
Develops with:
- Burns with extensive damage;
- Peritonitis;
- Massive blood loss;
- Severe traumatic injury;
- Intense poisoning with toxic substances.
Symptoms:
- Prolonged loss of consciousness;
- The skin is pale;
- Lips are bluish;
- Weak breathing;
- Cardiopalmus;
- Severe decrease in blood pressure;
- The pulse can only be felt on the carotid artery (information - how to find it).
At the first signs of OSHF, you need to call an ambulance: the body is not able to recover without timely treatment. In the hospital, resuscitation measures will be carried out and diagnostics will be made.
Diagnostics
When collecting anamnesis, the doctor pays special attention to the presence of complaints of shortness of breath and fatigue. Collects information about the existence of other diseases. If heart failure is suspected, the patient is referred for instrumental studies and laboratory tests.
The Cardiology Center of the Federal Medical and Clinical Center of the Federal Medical and Biological Agency carries out a full range of diagnostic measures:
- ECG in 12 leads;
- ECHO-KG;
- Holter monitoring;
- ECG with dosed physical activity;
- transesophageal ECHO-CG;
- ABPM (24-hour blood pressure monitoring);
- Ultrasound of the abdominal organs;
- general blood analysis;
- biochemical blood test (lipid spectrum, blood glucose, liver and kidney function indicators);
- thyroid hormones;
- coagulogram (a test to determine blood clotting);
- general urine analysis;
- spirometry (respiratory function test);
First aid
To alleviate the condition of the victim, you should:
- Lay it horizontally so that the head is below body level;
- Remove anything that may impede breathing (unfasten the top buttons, remove a tie, jewelry);
- Spray your face with water;
- Give ammonia.
For symptoms of collapse, you must:
- Place the victim horizontally, raise his head slightly;
- Remove elements squeezing the neck;
- Give hot tea, put hot water bottles on to warm it up;
- If possible, introduce caffeine or corglycone.
High arterial tone
Treatment
Treatment of OSHF takes place on an inpatient basis using a wide range of medications:
- Sympathomimetic drugs help increase blood movement in the veins;
- Nitrates dilate blood vessels and have a positive effect on cardiac activity;
- Anticoagulant drugs thin the blood and speed up its movement through the vessels;
- Diuretic medications eliminate swelling and reduce cardiac stress;
- Analgesic drugs reduce pain and alleviate the general condition.
If necessary, resuscitation measures are carried out. After relief of the main symptoms, the patient is prescribed medications for regular use and a diet with a reduced amount of salt. In some cases, surgical intervention is required.
To reduce the risk of developing OSHF, you should treat all heart and vascular diseases in a timely manner, avoid stress, lead a healthy lifestyle and undergo regularly scheduled medical examinations.
How to treat?
If cardiopulmonary failure has entered an acute form, treatment is carried out in a hospital under the supervision of cardiologists. Often the patient is admitted to intensive care. Here the patient remains completely at rest and breathes enriched oxygen.
If thromboembolism is detected, streptokinases and actilises are used to help dissolve the thrombotic mass. When using these drugs in the first two to three hours from the onset of an exacerbation of the disease, excellent results can be achieved. In some cases, surgery is performed. However, given the serious condition of the patient, this method is not always appropriate.
If pulmonary heart failure has become chronic, antibiotics and hormone-containing drugs are used to avoid the development of infectious diseases.
Simultaneously with the treatment of pulmonary disease, therapy is carried out aimed at maintaining cardiac activity. Diuretics are prescribed to remove excess fluid from the body, and drugs that stabilize blood pressure.
Thus, cardiopulmonary failure is a serious disease that requires an integrated approach to treatment. In addition to medicinal maintenance of the body, it is important that the patient himself follows all the recommendations of cardiologists, adheres to a certain diet, and gives up drinking alcohol and smoking. At the first manifestations of the disease, you should immediately seek medical help. In case of detection of serious diseases, timely treatment and subsequent prevention play an important role.