Doctors Cost
Price list Doctors clinic
Vegetovascular dystonia (VSD) is now called by doctors somatoform dysfunction of the autonomic nervous system. This is a common disease that affects women 2 times more often than men. VSD is just a syndrome, but it must be taken into account when prescribing treatment for the underlying disease. To talk about pathology, let’s remember how the human nervous system works.
Table 1. Human nervous system - simplified diagram
| Nervous system. | Somatic. Responsible for the work of skeletal muscles. A person can control it. | |
| Vegetative. Responsible for the functioning of internal organs. Does not submit to willpower. | Sympathetic. Strengthens the activity of the heart, constricts blood vessels, increases blood pressure. | |
| Parasympathetic. Relaxes heart rate, dilates blood vessels, reduces blood pressure. | ||
The autonomic nervous system has a central and peripheral division. Its representations are in the cerebral cortex, brainstem, hypothalamus, and spinal cord. The peripheral section is represented by ganglia and nerve plexuses. If there are disturbances in any of these departments, symptoms of VSD appear.
Causes
Vegetative-vascular dystonia in most cases is a secondary pathology that complicates existing somatic and neurological diseases, but requires mandatory treatment. There are causative and provoking factors for its development.
Table 2. Types and causes of VSD
| Factors | Kinds | Examples |
| Callers. | Psychogenic. | Stress. Neurosis. Depression. |
| Infectious. | Chronical bronchitis. Sluggish pyelonephritis. Encephalitis. | |
| Dishormonal. | Pregnancy. Climax. Puberty. | |
| Physical. | Radiation. Vibration. Overwork. | |
| Chemical. | Alcohol. Nicotine. Some medications. | |
| Brain lesions. | Encephalopathy. Consequences of TBI. Parkinson's disease. | |
| Somatic pathology. | Thyrotoxicosis. Diabetes. Hypertonic disease. | |
| Provoking. | Personality characteristics. | Psychovegetative reactions. |
| Constitutional predisposition. | Typical manifestations of VSD. | |
| Socio-economic prerequisites. | Low standard of living. Poor nutrition. Ultraviolet radiation deficiency. | |
| Perinatal factors. | Infections. Hypoxia. Rhesus conflict. |
Vegetative-vascular dystonia occurs as a result of a psycho-emotional reaction, its symptoms are superimposed on existing autonomic abnormalities of the human body, treatment must take this fact into account.
Diagnostics
Diagnosing VSD at home is impossible, due to the fact that to detect the disease it is necessary to examine all organs that are bothering the patient. For diagnosis, the following manipulations are carried out:
- interpretation of urine and blood tests;
- electrocardiography;
- echocardiography;
- breath tests;
- Ultrasound of the abdominal organs;
- electroencephalography;
- echoencephalography.
Also, when identifying a disease, it is important to study the patient’s hereditary information.
Doctors note that with sympathicotonia, patients were found to have hereditary diseases, such as diabetes mellitus or hypertension, and with vagotonia, neurodermatitis, ulcers or asthma. It is genetic predisposition that is the main factor influencing the risk of developing VSD.
Manifestations
VSD is characterized by many different manifestations. Almost all body systems are affected.
- Cardiovascular. Heart rate and blood pressure change, cardiac-type pain and changes in the ECG are noted.
- Pulmonary. There is a feeling of lack of air, inhalation is impaired, blood oxygen saturation deteriorates, and paresthesia appears.
- Nervous. Worrying headaches, tinnitus, weakness, dizziness, fainting. Thinking slows down. I am tormented by fluctuations in body temperature, hyperkinesis, and episodes of depressive mood.
Table 3. Action of the sympathetic and parasympathetic systems
| Sympathetic | Parasympathetic | |
| Pupil | Extension | Narrowing |
| Salivation | Insufficient | Excessive |
| Pulse | Increased frequency | Reduction |
| Arterial pressure | Promotion | Demotion |
| Bronchial lumen | Extension | Narrowing |
| Gastric juice | Decreased secretion | Increased secretion |
| Intestinal peristalsis | Reduced | Reinforced |
| Leather | Pale | Blushed |
| Sweating | Decreased | Increased |
Manifestations of vagotonic syndrome
VSD of the vagotonic type has a very diverse symptomatology, which leads the patient to search for all sorts of causes of disorders, suspicion of the presence of severe organic pathology of internal organs, and depressive disorders.
the predominance of the parasympathetic nervous system over the sympathetic one is a characteristic sign of the vagotonic type of VSD (=parasympathicotonia)
Heterogeneous signs of vagotonia, which do not fit into a single pathological process, force doctors to repeatedly examine patients in order to exclude somatic pathology. Some patients are treated by a psychotherapist, but continue to suffer from dysfunction of the digestive system, bradycardia, etc., others manage to get rid of some subjective symptoms, but apathy and panic attacks do not allow them to live in peace.
In this regard, in patients with probable hypotension, all complaints should be carefully weighed, correlating them with objective examination data, in order to avoid overdiagnosis of somatic pathology and incorrect treatment prescriptions.
Vagotonia can be of varying degrees of severity - from mild to severe. Along the flow they distinguish:
- Paroxysmal form, when symptoms appear in attacks due to stress, exacerbation of a chronic infection, overwork or lack of sleep;
- Constant;
- Hidden.
Depending on the systems involved in the pathological process, there is a generalized form of VSD of the vagotonic type (disorders of many organ systems), systemic, when complaints are limited to one of the organ systems, and localized (local) - disturbed by the dysfunction of one organ.
The most characteristic symptoms of vagotonia are:
Cardiac group - rare contractions of the heart (bradycardia), a tendency to low blood pressure (hypotension), pain and a feeling of constriction in the heart, freezing in the chest;- A complex of respiratory disorders - shortness of breath, reminiscent of an asthma attack, respiratory arrhythmia, a feeling of lack of air, inexplicable attacks of a dry, painful cough;
- Dysfunction of the digestive system - a feeling of a lump in the throat, difficulty swallowing, loss of appetite to its complete absence, rumbling in the stomach, belching, heartburn, nausea, diarrhea or constipation;
- Brain disorders - heaviness and pain in the head, weakness, drowsiness during the day and insomnia at night, a tendency to apathy, depression, hypochondria, lethargy and lethargy, poor concentration, memory loss, episodes of panic attacks, a feeling of the unreality of what is happening;
- Vestibular disorders - dizziness and fainting.
In addition to the above, patients with VSD of the vagotonic type also experience other symptoms - poor tolerance to heat and cold, chilliness, severe sweating, fluctuations in body temperature towards its decrease, itchy skin and a tendency to allergies, runny nose without an obvious infectious cause, excess body weight with decreased appetite, weather dependence and deterioration of health during sudden changes in weather conditions.
The most common symptoms of vagotonic syndrome are weakness, hypotension, bradycardia, shortness of breath, non-localized pain in the abdomen and chest, dizziness and decreased resistance to any type of stress, and fatigue. Vagotonia is accompanied by sleep disturbances - patients have difficulty falling asleep, sleep restlessly, or suffer from insomnia, but are drowsy during the day.
In adults and children with vagotonia, the appearance changes: the skin becomes pale or even cyanotic, the limbs are often cold to the touch, severe sweating is bothersome, weight increases with a small amount of food consumed.
A typical vagotonic person is apathetic, indecisive, unsure of himself, prone to self-examination, listens sensitively to the extremely varied symptoms of VSD and strives to visit as many doctors as possible, often trying to convince them of the presence of a terrible and incurable illness. The vagotonic person describes his complaints quite colorfully, paying maximum attention to each manifestation. Fear of a serious illness and constant search for it lead to deep depressive disorders and even suicidal tendencies.
Vagotonics quickly get tired, lack initiative, are extremely sensitive to criticism from outside, and at the same time tend to plunge into a state of daydreaming and purely personal internal experiences, which further complicates their social adaptation, learning, and work activity.
Often changes in character and psycho-emotional status come to the fore among other manifestations of vagotonia. Patients experience difficulty remembering any information, especially specific facts, while imaginative thinking remains quite good.
Many find it difficult to work both mentally and physically due to a constant feeling of fatigue and weakness, and drowsiness during the daytime. Subjective discomfort can lead to serious neurosis and neurasthenia, irritability, causeless mood swings, tearfulness and incontinence.
Vagotonia can occur chronically, when the symptoms are constantly disturbing, but crises with a sudden sharp deterioration in well-being are also possible. A mild crisis lasts about a quarter of an hour and is characterized by one symptom - sweating, bradycardia, fainting. A crisis of moderate severity is longer, takes up to 20 minutes and is accompanied by various manifestations - dizziness, pain in the heart, decreased pressure, freezing of the heart or slowing down of its work, abdominal pain, diarrhea, etc. Severe crises occur with pronounced vegetative symptoms, affecting many organs, convulsions and loss of consciousness are possible. After a severe attack, the patient feels exhausted, weak, and apathetic for the next few days.
In children, vagotonic dysfunction manifests itself:
- Pallor, cyanosis of the peripheral parts of the body;
- Increased sweating and swelling;
- Allergic mood;
- Chilliness and sensitivity to changes in weather.
Among the complaints of children with VSD of the hypotonic type, shortness of breath, a feeling of lack of air, and weakness predominate. These symptoms are especially pronounced in the presence of obstructive bronchitis and frequent respiratory infections.
Vagotonic children suffer from poor appetite, nausea, abdominal pain, spasms in the esophagus and pharynx. Babies in the first year of life are prone to regurgitation; the first few years are bothered by constipation and diarrhea for no apparent reason. With age, stool normalizes, but abdominal pain may persist into adolescence.
Pediatricians consider vagotonia with low blood pressure to be an independent pathology that manifests itself by the age of 8-9 years of a child’s life. Among the complaints of such children are pain in the head, in the heart area, and fatigue. Increased levels of anxiety, inattention, poor memory and sleep problems were also noted.
Vagotonia affects the general and intellectual development of a child who is overweight, does not tolerate sports well, and therefore does not engage in them. Constant fatigue and lack of adequate sleep make it difficult to learn and assimilate information, the child may fall behind the program at school, and there is no talk of attending additional classes and sections.
Vagotonic dysfunction does not have clear diagnostic criteria, including those established using objective research methods. The ECG in such patients shows bradycardia, conduction blockades up to severe forms cannot be ruled out. An ultrasound examination can detect dilated chambers of the heart due to a decrease in its tone. General and biochemical studies of blood and hormonal status usually do not show obvious deviations from the norm.
Vascular dystonia. Symptoms and treatment
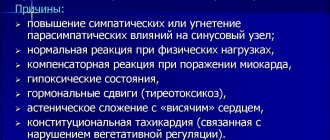
- Sympathicotonia is the predominance of the tone of the sympathetic nervous system. It is characterized by: pale skin, vasoconstriction, hypertension, tachycardia, dilated pupils, intestinal lethargy, heightened anxiety, and a feeling of fear.
- Vagotonia is the reverse state of sympathicotonia. Accompanied by redness of the skin, dilation of blood vessels, sweating, hypotension, bradycardia, constriction of the pupils, acceleration of bowel function, and irritability.
Sometimes the symptoms of VSD are mosaic; in this case, sympathetic and parasympathetic disorders are present simultaneously.
Therapy is selected individually, taking into account the main manifestations and the predominance of one or another department.
Causes of vagotonia
hypertonicity of the vagus nerve – the cause of vagotonia
The vagus nerve (paired) goes from the brain to the organs of the chest and abdominal cavity. It carries not only motor and sensory fibers, but also vegetative ones, which provide impulses to the lungs, digestive system, glands, and heart. An increase in its tone provokes a spasm of smooth muscles, increased motor activity of the intestines and stomach, and a slowdown in heartbeat, which is what is observed with vagotonia.
There is no single cause that causes vagotonic disorders. As a rule, this is a whole complex of unfavorable factors affecting a person simultaneously. In a number of cases, hereditary predisposition and constitutional features have been noted, which “result” in vagotonia under the influence of external causes.
Women are susceptible to vagotonia several times more than the male population. The disorder may first appear in childhood or adolescence, and by the age of 20-40 it will acquire the character of a persistent and pronounced disorder. According to some reports, signs of vagotonia are found in more than half of all people on the planet.
The most likely causes of vagotonic syndrome are:
- Head injuries, concussions, intrauterine hypoxia and birth injuries;
- Increased intracranial pressure;
- Emotional overload, stress, strong and prolonged experiences;
- Functional disorders of the digestive and respiratory organs;
- Physical inactivity;
- The presence of chronic foci of infection;
- Metabolic disorders, diabetes mellitus;
- Heredity;
- Change of climatic zones;
- Age: children, teenagers, menopausal women.
Vagotonia in children is associated with the natural immaturity of some elements of nervous regulation, rapid physical growth and hormonal changes during adolescence, and in women it is often provoked by pregnancy and childbirth, and the onset of menopause. These conditions are not a disease, they are natural, but can manifest themselves as a variety of autonomic disorders.
Vegetovascular dystonia. Symptoms
Sleep disturbance.
The most common problem for people suffering from a disorder of the autonomic nervous system. There are two extremes: increased drowsiness, when you constantly want to sleep, and insomnia due to disruption of biorhythms. In both cases, sleep is superficial and it is rare to get a good night's sleep. Conventional treatment has no effect.
Instability of the psycho-emotional sphere.
As a result of insomnia, the ability to concentrate is impaired and memory decreases. A person cannot do his job efficiently. Nervous breakdowns and mood swings occur. Periods of unbridled fun are replaced by apathy, depression, and sometimes directed aggression.
Dermographism.
If you run your fingernail over the patient’s skin, a white stripe will appear in sympathotonics, and a red stripe in vagotonics. This is due to the reaction of blood vessels. In the first case they narrow, in the second they expand. This is exactly how the skin reacts to stress and sports. These features must be taken into account when engaging in physical education and sports.
Breathing disorders
appear with parasympathetic VSD. As the load on the bronchi increases, shortness of breath develops. Triggering factors include stress, physical activity, and ARVI. The well-being of patients worsens over the years, shortness of breath gives way to attacks of suffocation. Some patients develop bronchial asthma.
Meteosensitivity.
The human body reacts extremely violently to changes in atmospheric pressure, windy or rainy weather. Weakness appears, severe headaches sometimes put you to bed, and a complete lack of performance.
Digestive problems
with VSD, the symptoms are varied and opposite: increased and decreased appetite, diarrhea and constipation, abdominal pain, nausea, food selectivity. Treatment by a gastroenterologist helps little.
Disorders of the genitourinary system.
Increased or decreased urination, pain in the perineum, lower abdomen in the absence of pathology, menstrual irregularities, libido, erectile dysfunction.
Headache and dizziness
caused by impaired cerebral vascular tone. They are provoked by mental and emotional overload and stress. Sometimes fainting, tinnitus, and nausea may occur.
Table 4. Severity of VSD
| Degree | Manifestations |
| Easy. | Functionality has been preserved. The discomfort is minimal and occurs periodically. |
| Average. | Periodically, the ability to work is lost due to the occurrence of vegetative crises. |
| Heavy. | Inability to work due to persistent and long-term vegetative disorders, frequent crisis conditions. |
Causes of VSD
External factors causing the development of VSD are acute and chronic psycho-emotional stress; iatrogeny; infections (tonsillogenic, carious, bacterial, viral); physical and chemical effects (brain injuries, chronic intoxication, hyperinsolation, vibration, ultra-high frequency currents, ionizing radiation), alcohol abuse; overwork.
The interaction of internal and external factors leads to disruption at any level of the complex neurohumoral and metabolic regulation of the cardiovascular system, and the leading link in the pathogenesis of VSD is damage to the hypothalamic structures of the brain, which play a coordinating and integral role in the body. Neurologists, neuropathologists and reflexotherapists believe that the leading role in the development of VSD is given to hereditary-constitutional factors, which manifest themselves in the form of functional insufficiency of the regulatory structures of the brain or their excessive reactivity; features of the course of a number of metabolic processes and altered sensitivity of the peripheral receptor apparatus. Dysregulation manifests itself in the form of dysfunction of the sympathoadrenal and cholinergic systems, histamine-serotonin and kallikrein-kinin systems, disorders of water-salt and acid-base states, oxygen supply to physical activity, and decreased oxygen in tissues. All this leads to the activation of tissue hormones (serotonin, histamine, catecholamines) with subsequent metabolic disorders, microcirculation with the development of degenerative processes in the myocardium.
Crises with vascular dystonia. Symptoms and treatment in adults
Panic attack
– sympathoadrenal crisis. A huge amount of adrenaline is released into the blood. A sharp headache occurs, blood pressure rises, the heart “jumps out of the chest,” the skin turns pale. Fingers and toes become cold and numb. A person feels a strong feeling of anxiety and fear. The crisis passes on its own. After it, the patient feels exhausted for a long time.
Vagoinsular crisis
occurs when insulin is released into the blood. As a result, glucose levels drop sharply and heart failure occurs. It seems to stop. The patient feels short of breath. The pulse slows down, the pressure drops, and the vision becomes dark. Fainting may develop. The skin turns red and there is increased sweating. There may be diarrhea and flatulence.
VSD classification
Signs of the disease depend on the condition of the blood vessels. Depending on this, several types of vegetative-vascular dystonia are distinguished - hypertonic, hypotonic, cardiac, mixed, vagotonic.
This disease occurs in the form of attacks, in the form of two or three pathologies. Depending on the severity of VSD, the following forms are distinguished:
- Mild – working capacity remains, symptoms of VSD do not cause discomfort. There are no vegetative crises.
- Moderately severe – periods of loss of ability to work appear from time to time. This is associated with relapses of vegetative-vascular dystonia and the appearance of a vegetative crisis.
- Severe – represents a long and persistent course of VSD; acute conditions and crises are common. Then the inability to work for a long time is diagnosed.
Hypertensive type
Symptoms and treatment are associated with pronounced vascular tone. It is accompanied by an increase in blood pressure. Main criteria for VSD:
- cardiopalmus;
- hot flashes;
- headache;
- increased fatigue of the body and psychological mood;
- nausea and vomiting;
- loss of appetite;
- increased sweating;
- strong feeling of fear;
- floaters before eyes.
Hypotonic type
Characteristic symptoms of the disease leading to a decrease in vascular tone and blood pressure include:
- darkening of the eyes;
- fainting;
- weakness in the body, arms and legs;
- a sharp drop in pressure;
- pale skin;
- nausea;
- gastrointestinal dysfunction - diarrhea or constipation;
- heartburn, belching;
- respiratory disorders;
- cold feet and palms.
Mixed type
It is characterized by variability in vascular tone, so blood pressure parameters fluctuate. It rises sharply, then suddenly falls.
With this type, the symptoms of VSD change. This negatively affects the quality of life of patients; weakness, increased sweating, and fainting are replaced by headaches, hot flashes, and symptoms of tachycardia.
Attacks during VSD are accompanied by fear of death and breath holding. This provokes aggravation of the situation. There is pain in the heart.
Cardiac type
Accompanied by aching, throbbing pain in the heart muscle. It has no effect on well-being. Sometimes patients with VSD develop symptoms of arrhythmia and severe sweating, but studies do not reveal pathologies of the cardiovascular system.
Vagotonic type
This type of vascular dystonia is characterized by respiratory abnormalities. The person is unable to take a deep breath and feels tightness in the chest. There is a high probability of low blood pressure and slow heartbeat. Increased salivation is observed, and gastrointestinal problems appear.
VSD in men
A distinctive feature of VSD in male patients is considered to be erectile dysfunction. Then they go to the doctor. When vascular dystonia is detected, symptoms and treatment (taking pills) will differ significantly.
VSD in women
In women, VSD develops due to hormonal instability. Such problems are observed during menopause or pregnancy. A hereditary tendency becomes a risk factor.
Vegetative-vascular dystonia. Treatment
A neurologist selects a treatment regimen based on complaints, gender, age, examination and diagnostic results. No two people with VSD are treated exactly the same. Therefore, you should not self-medicate.
Sedatives, tranquilizers, antidepressants, nootropics and some other drugs are used as drug therapy.
Good help: psychotherapy, physiotherapy, reflexology, sanatorium treatment.
But the main thing is to normalize the rest and work regime, to create a comfortable psycho-emotional environment.
Prevention
Vegetative vascular dystonia is a long-term disease, the symptoms worsen periodically. Every year new treatment methods appear for adults and children. However, it is very important to follow the rules to minimize the risk of exacerbations.
- Provide sufficient, but not excessive, physical activity.
- Give up bad habits and excessive coffee consumption.
- Avoid stress, if it arises, immediately work through it with a psychotherapist.
- Maintain a balance of work and rest.
- Eat rationally, preferring foods of plant origin.
- Take massage courses twice a year.
- Try to go to a sanatorium every year or take preventive therapy courses at a clinic.
Treatment
Despite the genetic predisposition to the disease, its development can be prevented, subject to compliance with the regime, dosage time for work and rest, as well as proper nutrition. So, if a patient has high blood pressure, it is worth reducing the amount of salt, confectionery, fatty foods, and fried foods consumed. With low blood pressure, doctors recommend not to indulge in foods containing iodine, sodium and potassium in large quantities, to maintain a sleep schedule, not to overwork, and to avoid stressful conditions.
In the fight against the disease, experts focus on a non-drug method, namely:
- massage;
- acupuncture;
- physiotherapy;
- water procedures.
To reduce and alleviate symptoms, medicinal herbs are used:
- Eleutherococcus;
- ginseng root;
- lure;
- Aralia;
- motherwort;
- valerian;
- hawthorn.
In case of low effectiveness of the described methods, doctors resort to the use of pharmaceuticals, which are selected separately for each patient. In addition, antidepressants, sedatives, vitamin-mineral complexes, and drugs that restore blood supply to the brain can be used.
For successful recovery, regular examination is required - once every 3-6 months. Neurocircular dysfunction, as a rule, intensifies in spring and autumn, so it is better to prescribe all therapeutic measures at this time of year.
In case of untimely or poor-quality treatment, dystonia progresses and leads to the appearance of a variety of pathologies in the body, but if you follow the doctor’s instructions and monitor the course of the disease, the prognosis is favorable.