Iron deficiency anemia in children is one of the types of anemia, which is characterized by iron deficiency, leading to impaired hemoglobin synthesis. On average, about 80% of cases of anemia in children are due to iron deficiency. The pathology is quite common: its incidence rate is about 40% among young children.
Treatment of iron deficiency anemia in children can be done at the CELT multidisciplinary clinic. We employ highly qualified specialists who will accurately diagnose and prescribe appropriate treatment. Symptoms and treatment of anemia in children will be discussed in this article. Don't forget: the sooner you seek professional medical help, the more effective the treatment will be.
What is iron deficiency anemia in a child?
Pediatricians around the world deal with this disease every day.
This group of diseases includes those associated with a decrease in the content of hemoglobin and/or red blood cells per unit volume of blood, which negatively affects the oxygen supply to the body’s tissues. Iron deficiency anemia is the most common of all anemias, accounting for 80% of all cases. In our country and Europe, the prevalence of iron deficiency anemia in young children is approximately 50%, and in older children - 20% or more.
Iron deficiency anemia in a child is a syndrome characterized by a lack of iron in the body. It develops against the background of pathological processes and is manifested by signs of anemia and sideropenia.
Iron is one of the main microelements in the body of both children and adults. The body has hemoproteins, which contain about 70% of the total amount of iron, which is associated with porphyrin. Iron is contained in hemoglobin, myoglobin, peroxidases, cytochromes, catalases, etc.
This element is stored in the body in the form of ferritin (the majority) and hemosiderin. In babies, most of the iron is stored in erythroid cells and very little in the muscles.
Diagnostics
Diagnosis of iron deficiency anemia in infants and older children in the multidisciplinary CELT clinic is carried out with the participation of various specialists:
- pediatrician;
- hematologist;
- pediatric gastroenterologist.
The child is examined, a medical history is taken, and a laboratory examination is performed, which makes it possible to establish a diagnosis of anemia and determine its degree. For the purpose of additional examination, it is possible to use an ultrasound diagnostic method (abdominal organs, pelvic organs).
Pathogenesis (what happens?) During iron deficiency anemia in a child:
Iron leaves the body through urine, feces, sweat, as well as through nails, hair and skin. Losses do not depend on gender. In children, about 0.1–0.3 mg is released into the external environment per 24 hours. In adolescents, the loss is a maximum of 0.5–1.0 mg. The child needs to receive 0.5–1.2 mg of iron per day. There is an increased need for infants and preschoolers. In order for a child to develop normally, the diet should contain 1.5 mg of iron per day in newborns, and at least 10 mg in children from 1 to 3 years old.
Iron deficiency provokes a tendency to infectious diseases of the baby's gastrointestinal tract and respiratory system. Without iron, brain structures cease to function normally. With a lack of iron, disruptions occur in the neuropsychic development of the baby. In children who were diagnosed with iron deficiency anemia in infancy, at the age of 3-4 years, disturbances in the transmission of nerve impulses from the centers of the brain to the organs of hearing and vision are found due to impaired myelination and, as a consequence, impaired nerve conduction.
Causes
According to the time of occurrence of anemia there are:
- Intrauterine.
During intrauterine development, the fetus creates an iron reserve, on average 300 mg. Peak iron accumulation occurs in the third trimester. If the period from 28 to 32 weeks is unfavorable (threat of miscarriage, placental abruption, fetoplacental insufficiency), the fetus does not have time to stock up on iron. The likelihood of anemia is high in premature babies and children born from multiple pregnancies. - Intranatal and early neonatal.
During childbirth, prerequisites for the development of anemia can also be created - early placental abruption, rupture of umbilical cord vessels, and fetal injuries. After birth, the main danger is fetal hemolytic disease (destruction of fetal red blood cells by maternal antibodies) and genetically determined bone marrow diseases. - Purchased.
Anemia is subsequently caused by poor nutrition. This happens if there is little iron in breast milk, inappropriate formulas or cow's milk are used. Premature babies and those children whose body weight is higher than normal require more iron than usual. Anemia occurs when there is insufficient supply of B vitamins, macro- and microelements, and when the baby lives in poor sanitary and hygienic conditions.
At risk are children with blood diseases, frequent nosebleeds, food allergies and atomic dermatitis (a childhood form of eczema), impaired absorption in the intestines. In children, anemia develops with any more or less severe infection (pyelonephritis, bronchiectasis), helminthic infestation, connective tissue diseases (rheumatoid arthritis).
Less known clinical manifestations of iron deficiency include:
- neurotic reactions and neurasthenia;
- decreased muscle performance and general exercise tolerance;
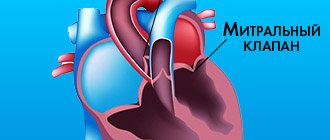
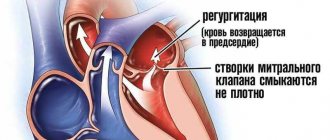
- disturbances of metabolic processes in the myocardium;
- disorders of peripheral circulation and microcirculation.
The diagnosis of IDA is based on the characteristic clinical picture, changes in the blood and absolute iron deficiency.
Prevention of anemia
Prevention begins with good nutrition for the pregnant woman, allocating sufficient time for walking and sleeping. Children of the first year of life need to add complementary foods to breast milk after 6 months of age; for older children, a varied, balanced diet should be organized. It is important that during the warm season the baby spends as much time outdoors as possible and takes sunbathing. The team of doctors at the SM-Doctor clinic will help your baby cope with anemia and develop individual preventive measures. Contact professionals to create ideal conditions for the growth and development of your child!
Medical Internet conferences
Early diagnosis of oncohematological diseases in children is extremely difficult due to the nonspecificity of primary symptoms, which are often hidden under the “masks” of other diseases [2, 27]. Oncological alertness and knowledge of probable symptoms will allow the practitioner to diagnose this pathology earlier and, therefore, significantly improve the prognosis for the patient [1, 3, 4, 5].
In most children, acute lymphoblastic leukemia (ALL) manifests rapidly and is characterized by clinical polymorphism. The preleukemia stage does not have characteristic clinical symptoms [6, 7], and the analysis of the symptoms of the initial period is carried out retrospectively [7], and therefore the diagnosis is not made on time. Despite the progress of laboratory diagnostics, it is difficult to detect leukemia in children in the early stages, because For characteristic changes in the hemogram to appear, the tumor must reach a critical mass [4], and the manifestation of ALL is associated with blast infiltration of various organs with disruption of their function [8]. Clinical symptoms in this case are ahead of laboratory changes, and the child is not hospitalized in a specialized hematology hospital [55].
ALL occurs predominantly in children aged 0–15 years, with a peak incidence observed at the age of 2–5 years [54]. A more favorable prognosis and effect of therapy is observed in children from 1 to 10 years of age, while in children younger than 1 year and older than 10 years, ALL has an unfavorable course and is difficult to treat [46].
Gender differences:
Studies aimed at studying gender differences in ALL showed that in B-ALL the gender distribution was the same: boys - 51%, girls - 49%, while the T-variant was found predominantly in boys (90%).
Constitutional features. There is data in the literature on the connection between the onset and course of the initial period of ALL with the constitutional type of the child (asthenoid, thoracic-muscular, digestive): the most severe course is observed in children with a digestive body type [55].
Predisposing factors. When diagnosing ALL, the doctor must take into account a wide range of predisposing factors that can lead to the development of ALL: socio-economic status of the child’s family, chromosomal abnormalities, Down syndrome, neurofibromatosis, variable immunodeficiency, Ig A deficiency, Fanconi anemia, Shwachman syndrome, congenital X- linked agammaglobulinemia [56].
In the clinical picture of acute lymphoblastic leukemia, 5 main syndromes are most common (Table 1):
- Intoxication syndrome. Most often, patients are concerned about prolonged fever of unknown origin, intoxication of varying degrees, weakness, fever, malaise, and weight loss. Fever may also be associated with the presence of a bacterial, viral, fungal or (less commonly) protozoal infection, especially in children with neutropenia [7].
- Osteoarticular syndrome. Manifestations from the musculoskeletal system are detected mainly in children with B-cell ALL, which is characterized by less involvement of extramedullary organs and unclear changes in the peripheral blood [18]. Osteoarticular syndrome is often the first manifestation of ALL in children [9, 10]. Studies have shown that in patients with ALL, osteoarticular syndrome was recorded in 54% of cases, with a higher frequency in children from 1 to 9 years of age. The presence of joint pain was noted in 16.2% of children with ALL, arthritis in 26.6%, and changes in gait in 32.8%. Large joints were most often affected: knees - 10.6%, ankles - 9.4%, elbows - 4.4%, shoulders - 3.6% [11]. Upon examination, swelling of the joints, the presence of effusion, and dysfunction of the affected limb were revealed [12]. Patients often complained of frequent and multiple fractures, which may be due to osteoporosis [13]. Clarifying diagnosis is also necessary if recurrent multifocal osteomyelitis is suspected [14]. Acute lymphoblastic leukemia in rare cases manifests itself as osteoarthritis, the incorrect interpretation of which can lead to errors in differential diagnosis with juvenile rheumatoid arthritis (JRA). Children with ALL have asymmetric oligoarthritis, which is manifested by fever, pallor, arthritis, night pain, and bone pain [19]. Damage to the skeletal system at the onset of ALL is characterized by polymorphism of radiological manifestations. In some cases they are uninformative (only a slight periosteal reaction is revealed) [15], in other cases osteolysis, osteopenia, osteosclerosis, pathological fractures, periosteal reactions and mixed lesions in the form of lysis-sclerosis were detected [16]. An important symptom is the discrepancy between clinical symptoms and radiological data. The combination of hyperthermia, intoxication and articular syndromes can mimic septic arthritis. However, the lack of an adequate response to antibacterial therapy allows one to suspect ALL. The pathological process in this case develops as a result of metaphyseal sclerosis [3]. Intractable pain and joint syndromes characteristic of juvenile idiopathic arthritis must be considered from the standpoint of differential diagnosis with ALL [16]. Similar clinical symptoms in combination with pancytopenia are characteristic of necrosis of the bone marrow substance [17]. These data highlight the importance of including ALL in the differential diagnosis of musculoskeletal disorders even in the presence of apparently normal peripheral blood findings.
- Lymphoproliferative syndrome. Enlarged lymph nodes are associated with leukemic tissue infiltration [57]. The most often enlarged cervical, inguinal, axillary lymph nodes, which have a dense elastic consistency, are painless on palpation, are not fused with the surrounding tissue, are mobile, the skin over them is not changed. Some children may experience Mikulicz's symptom complex (simultaneous enlargement of lymph nodes in the submandibular, parotid and periorbital region). There may be a significant increase in the lymph nodes of the mediastinum, up to compression of the superior vena cava (shortness of breath, cyanosis, puffiness of the face, pasty eyelids, bulging of the jugular veins). Along with lymphadenopathy, in 75% of cases hepatosplenomegaly is detected, which is not accompanied by pain [2, 6].
- Anemic syndrome is characterized by increasing pallor with worsening general condition, dizziness and headache, shortness of breath, tachycardia [2].
- Hemorrhagic syndrome is associated with both thrombocytopenia and intravascular thrombosis (especially with hyperleukocytosis) [46]. Patients may complain of polymorphic hemorrhages (from petechiae to large hemorrhages) on the skin and subcutaneous tissue of various locations. Bleeding from the mucous membranes (nasal, gingival, gastrointestinal, renal, uterine) is observed [2, 58].
, clinical manifestations from other organs may be observed, and in some cases predominate [27] (Table 1).
- Lesions of the mucous membranes. One of the early symptoms of ALL in children is lesions of the oral mucosa in the form of erythema, ulcers and swelling of the lips, tongue, palate and gums [21]. Often the diagnosis is accompanied by difficulties in differential diagnosis with surgical pathology of the face. Thus, a case of ALL was described in a girl with swelling of the nasolabial area, which was regarded as phlegmon. The changes described above were associated with infiltration of the mucosa and soft tissues by blast cells [22].
- Skin manifestations. ALL in children in some cases manifests itself in the form of various skin manifestations, which are usually based on a leukemic infiltrate with damage to the skin and subcutaneous tissues. Localization can be different: the head area is affected in the form of small nodules [23], or other areas of the skin [24]. A case of skin lesions in the external auditory canal is described, in which the child was initially diagnosed with diffuse external otitis media [25].
- Eye lesions. Ophthalmological manifestations in patients suffering from acute lymphoblastic leukemia may also be its first manifestation [26, 27]. Complaints and clinical manifestations differ in polymorphism [28]. The most common sign of eye damage in ALL is hemorrhages in various parts of the eyeball: retina, subconjunctival hemorrhages [29]. When examining the fundus, swelling of the optic nerve nipple and vascular infiltration may be detected.
- Abdominal syndrome. Abdominal syndrome manifests itself in the form of abdominal pain of unknown etiology, alternating diarrhea and constipation, which is associated with lymphoid infiltration of parenchymal organs and the intestinal wall. In rare cases, ALL can be hidden under the “mask” of acute pancreatitis, which is difficult to treat [30], as well as typhlitis [31], which requires additional differential diagnosis.
- Damage to the genitourinary system. Clinical manifestations of kidney disease caused by malignant infiltration may be the primary manifestation of the disease in patients with ALL and are represented by acute renal failure [32, 33], renal arterial hypertension [34], palpable mass syndrome and bilateral nephromegaly, which must be differentiated from Wilms tumor [ 35, 36]. A feature of the clinical picture of acute renal failure in such cases is the absence of oliguria against the background of severe nephromegaly [37, 38]. In addition, there is evidence of the primary manifestation of ALL in the form of nocturnal enuresis in a child [39].
- Neurological symptoms. Neurological symptoms are not only a sign of the development of neuroleukemia in children with ALL, but may also be the only early clinical manifestation of the disease. The clinical picture is predominantly associated with damage to the cranial nerves (CN). In one case, with damage to the motor branch of the trigeminal nerve in a child, the only symptom was trismus of the masticatory muscles [40], and in another, with damage to the sensory branch, sensory neuropathy (Numb chin syndrome) was noted [41]. The primary manifestation of ALL in a number of cases was an isolated lesion of the abducens nerve with corresponding oculomotor symptoms [42, 43]. In addition to lesions of the cranial nerve, manifestations of neurodegeneration (Louis-Bar ataxia-telangiectasia) with corresponding immune and hematological disorders can also be observed in the clinic [44]. ALL can debut as a paraneoplastic neurological syndrome (PNS), manifested by acute muscle weakness of the proximal muscles of the upper and lower extremities [20].
- Lung damage. Respiratory system disorders may be associated with enlarged mediastinal lymph nodes, characteristic of T-cell leukemia, leading to the development of superior vena cava syndrome or respiratory failure. There may be leukemic infiltration of the lung tissue and/or hemorrhages into it. It is sometimes difficult to differentiate these complications from an infectious process [45].
- Disorders of mineral metabolism. Disorders of mineral metabolism that develop in ALL are characterized by hypercalcemia, which can be the first symptom of the disease [50, 51] or its complication [52]. In patients with hypercalcemia, complaints from the gastrointestinal tract and osteoarticular system prevail [53].
- Infectious diseases. In some cases, the onset of ALL can occur under the “mask” of some infectious diseases, for example, acute respiratory viral infection, infectious mononucleosis, tonsillitis, whooping cough, parawhooping cough, pneumonia, mumps [59, 60, 61, 62].
Hematological changes. The most important diagnostic test to suggest ALL is a complete clinical blood test with a leukocyte count.
Hematological changes in ALL do not have clear patterns, and often their severity may not correspond to clinical symptoms; changes in blood tests characteristic of ALL may be absent, which indicates a comprehensive assessment of clinical and laboratory data.
Most often, a hemogram reveals pronounced leukocytosis, while the number of leukocytes varies widely and depends on the type of ALL. Thus, the average number of leukocytes in children with the B-variant ALL was 37.1 ± 12.2*109/l, and in the T-variant ALL – 123.3 ± 36.5*109/l [63]. It is noted that forms of ALL with hyperleukocytosis have a more unfavorable prognosis [46].
Along with leukocytosis, blastemia is observed up to 80-90% [27], and a small percentage of blast cells does not provide grounds for making a diagnosis of ALL, while their absence does not allow it to be completely excluded [47, 64].
In rare cases, persistent unexplained hypereosinophilia (up to 80%) is observed at the onset of the disease, which can be combined with skin manifestations [48], and in 25-30% of cases - lymphocytosis. The cytopenic variant of ALL is characterized by leukopenia and absolute neutropenia [4]. An increase in the leukocyte pool leads to inhibition of other hematopoietic germs, which is accompanied by a decrease in the number of red blood cells and hemoglobin, as well as thrombocytopenia [27, 46, 65, 66].
A number of studies contain data on the development of metabolic lactic acidosis in the initial period of ALL [49].
Thus, the primary clinical manifestations of acute lymphoblastic leukemia in children are characterized by pronounced polymorphism, which requires doctors of all specialties to be oncological vigilant, a comprehensive assessment of the anamnesis, consistent analysis of clinical data from all body systems, and the use of an adequate set of laboratory and instrumental studies. In doubtful cases, the child should be referred for consultation to a pediatric hematologist-oncologist.
Treatment of anemia
Methods for correcting anemia depend on age.
When breastfeeding, it is necessary to introduce vegetable, fruit and meat complementary foods on time, and spend a lot of time in the fresh air, including in the sun. The room must be well ventilated, kept clean, and sanitary rules for child care must be observed. For older children, it is enough to streamline their diet and daily routine to improve their blood tests. The diet includes beef liver, legumes, seafood, fresh vegetables and fruits, and herbs. If necessary, the timing of vaccination is postponed, massage and ultraviolet irradiation are used.
Medicines are prescribed by a doctor. Iron supplements and vitamins are indicated. The minimum duration of drug treatment is 1 month.