Treatment of cardiac arrhythmias (HADs) is one of the most challenging tasks in cardiology. This is due to the wide variety of arrhythmias, imperfection of antiarrhythmic drugs and difficulties in choosing treatment tactics [1].
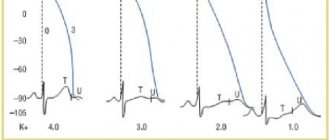
Cardiac arrhythmias develop when the functions of automaticity, excitability and conduction are impaired. As a result of changes in the functioning of potassium, calcium and sodium channels, the cell's action potential and the speed of impulse transmission change. Disruption of ion channels largely depends on the activity of the sympathetic division of the autonomic nervous system, concentrations of acetylcholine, ATP and the functioning of muscarinic-like M2 receptors [2].
The main reasons leading to LDCs:
• myocardial lesions of any etiology, including atherosclerosis of the coronary arteries, hypertrophic and dilated cardiomyopathies, heart defects, myocarditis, myocardial hypertrophy in arterial hypertension and chronic pulmonary heart disease;
• hormonal imbalance in diabetes mellitus, thyroid diseases, menopausal syndrome;
• intoxication with drugs, nicotine, alcohol, narcotic substances, industrial poisons (arsenic, cobalt, mercury, chlorine and organophosphorus compounds);
• disturbances in the metabolism of electrolytes of potassium, calcium, sodium, magnesium, acid-base status;
• neurovegetative imbalance, manifested by a predominance of activity of the sympathetic or parasympathetic part of the autonomic nervous system;
• lesions of the sinus node and cardiac conduction system of congenital or acquired origin;
• heart valve prolapse;
• mechanical irritations of the heart during cardiac surgery, catheterization and angiography [1, 3].
In clinical practice, a large number of drugs with different mechanisms of action are used to prevent and treat arrhythmias. Most antiarrhythmic drugs affect the shape of the action potential of cardiomyocytes, realizing their effects by influencing certain transmembrane ion currents [4].
Based on the effect of antiarrhythmic drugs on the shape of the action potential, they are divided into four classes. For the first time such a classification was proposed by E.M. Vaughan-Williams in 1971. Then, in 1979, it was modified by D. Harrison.
Representatives of class I antiarrhythmic drugs are sodium channel blockers and are divided into three subclasses. The IA subclass includes drugs that moderately slow down conduction and prolong the action potential - procainamide, quinidine, etc. IB subclass includes drugs that minimally slow down impulse conduction and slightly shorten the action potential - lidocaine, mexiletine, etc. Drugs of the IC subclass – propafenone, etacizine, flecainide, etc. – significantly slow down conduction and minimally prolong the action potential. Class II includes β-blockers - atenolol, propranolol, etc. A characteristic feature of class III drugs is the ability to lengthen the repolarization period. The most well-known drugs in this group are amiodarone, bretylium tosylate, and sotalol. The fourth class of antiarrhythmic drugs is represented by calcium channel blockers – verapamil, diltiazem, etc. [4].
However, this classification is not complete. Some drugs with antiarrhythmic activity do not fall within the four classes of antiarrhythmic drugs due to their mechanism of action. This group includes adenosine, cardiac glycosides, preparations of potassium and magnesium salts [4, 5]. Meanwhile, the role of these antiarrhythmic drugs in the treatment of NRS is very significant.
Currently, arrhythmias associated with electrolyte imbalance, in particular with impaired magnesium metabolism in the body, are especially relevant [6].
Magnesium deficiency is common in modern populations. The frequency of hypomagnesemia is quite high and, according to some authors, ranges from 10 to 34% [7]. In other studies, hypomagnesemia was detected among 42% of hospitalized patients [8]. However, even in the absence of hypomagnesemia, the body may experience a lack of magnesium. This phenomenon is explained by the fact that when there is a lack of this macroelement in the body tissues, magnesium can be released from the bones and its serum concentration turns out to be normal.
Therefore, in recent years the term “magnesium deficiency” has often been used. This term refers to a decrease in the total magnesium content in the body, while the concept of “hypomagnesemia” means a decrease in the concentration of magnesium in the serum below 0.8–.2 mmol/l [9].
There are primary and secondary magnesium deficiency. Primary magnesium deficiency is caused by disturbances in the genes responsible for transmembrane magnesium metabolism. More common is secondary magnesium deficiency, which can be caused by poor diet, poor social conditions, environmental conditions, stressful situations and various diseases.
The most common is nutritional magnesium deficiency. In modern refined products, fast food, vegetables and fruits grown using intensive technologies, the magnesium content is minimal. Magnesium deficiency is also aggravated by physical overexertion, stress, and alcohol abuse. Increased consumption of this macronutrient is observed during pregnancy and lactation [10].
Magnesium is one of the key elements of metabolic reactions for the formation, accumulation and utilization of energy; it is involved in the synthesis of proteins, including connective tissue collagen, and the exchange of nucleic acids and lipids. It plays an important role in regulating the state of the cell membrane and the processes of transmembrane transport of calcium and sodium ions. Therefore, magnesium primarily determines the normal functioning of nervous tissue, including the conduction system of the heart [6, 11, 12].
Clinical manifestations of magnesium deficiency are varied. There may be a decrease in mental and physical performance, increased anxiety, irritability, headaches, skeletal muscle cramps, spastic contractions of the intestines and other symptoms [9].
One of the characteristic manifestations of magnesium deficiency is LDCs. The effect of magnesium on heart rhythm is carried out through its effect on the transport of potassium, sodium and calcium ions, i.e., on the ions responsible for the formation of the action potential. When the content of magnesium ions in tissues is insufficient, transmembrane metabolism is disrupted and the electrical excitability of cardiomyocytes increases. This can lead to tachycardia and ectopic arrhythmias [13].
With long-term magnesium deficiency, other disorders in the cardiovascular system develop. In biological environments with a lack of magnesium, calcium salts accumulate over the years, and therefore the likelihood of calcification of atherosclerotic vascular plaques increases (potentiated by pyridoxine deficiency). The consequences of chronic magnesium deficiency include the development of arterial hypertension, endothelial dysfunction, accelerated progression of atherosclerosis, and increased risk of myocardial infarction and stroke [6, 9, 11, 13, 14].
The Framinghem Heart Study showed a correlation between long-term hypomagnesemia and a high incidence of ventricular extrasystoles, tachycardia, and ventricular fibrillation. The results of the PROMISE Study also indicate a higher frequency of ventricular extrasystoles and high mortality in the group of patients with hypomagnesemia [9].
The effectiveness of treating NRS with magnesium preparations has been proven in clinical studies. As an antiarrhythmic drug, magnesium salts are the drug of choice for congenital and acquired long QT syndrome and torsades de pointes. The effectiveness of magnesium preparations has also been shown for arrhythmias resulting from therapy with amiodarone and class I antiarrhythmic drugs. The effectiveness of magnesium preparations is associated with its ability to inhibit the development of trace depolarizations, shortening the duration of the QT interval [15, 16].
Magnesium preparations are also prescribed for the prevention and treatment of arrhythmias provoked by glycoside intoxication. Under the influence of magnesium ions, the function of the potassium-sodium pump of cardiomyocytes is restored [17].
In the treatment of NRS, both parenteral forms of magnesium salts and oral medications can be used, while for prevention it is most advisable to use dosage forms intended for oral administration. However, the possibilities of oral administration of inorganic magnesium salts are limited, since they cause diarrhea, and the percentage of magnesium absorption from them is about 5% [9].
In this regard, to correct magnesium deficiency, prevent and treat NRS, oral medications are currently mainly used, in which magnesium is usually combined with organic acids. Oral magnesium preparations are included in combination therapy regimens for many cardiovascular diseases. They are effective, well tolerated by patients and affordable.
One of the most successful organic compounds for use in clinical practice is magnesium orotate (OM) [18, 19]. Not only is it a source of magnesium, but it also has its own metabolic effects.
OM introduced from the outside accelerates biosynthetic processes, which at the level of the heart muscle is expressed in an increase in the synthesis of ATP and protein. It is OM that is optimal for fixing magnesium to ATP in the cell [19].
It has been established that OM has cardioprotective properties: it increases myocardial resistance to ischemia, accelerates its regeneration and increases survival during myocardial infarction. In addition, OM has a protective effect on the central nervous system during hypoxia, intoxication, injury, and helps reduce the level of total cholesterol, which in turn inhibits the development of atherosclerosis [18,19].
OM, due to the enhanced formation of pyrimidine nucleotides, stabilizes metabolic processes in damaged myocardial cells. Due to this, the loss of magnesium is reduced, which has a stabilizing effect on the myocardium and has significant clinical significance [13, 19, 20].
In Russia, the only drug containing OM today is Magnerot®. Our country has accumulated extensive experience in its use by cardiac patients. The main indication for the use of Magnerot® is Mg2+ ion deficiency and associated NRS. The ability of Magnerot® to prevent ventricular arrhythmias torsades de pointes in long QT syndrome, including in pregnant women and children, has been proven. Magnerot® is also effective for other types of ventricular and supraventricular extrasystole and can be used as a supportive agent after stopping an attack of atrial fibrillation. However, in case of severe cardiac arrhythmias, it is better to combine it with other antiarrhythmic drugs [21].
In recent years, a number of studies have been published on the positive effect of using magnesium preparations for cardiac rhythm and conduction disturbances in patients with congenital connective tissue dysplasia and mitral valve prolapse (MVP). According to epidemiological studies, in patients with MVP, magnesium deficiency is detected in almost 2/3 of cases. After treatment with magnesium drugs, patients with MVP experience a decrease in the number of ventricular extrasystoles, and therefore some authors consider this therapy to be etiopathogenetic [22].
The antiarrhythmic effects of magnesium orotate are widely used in pediatric practice. It was shown that in children with connective tissue dysplasia syndrome, Magnerot® therapy led to a decrease in echocardiographic signs of MVP and the frequency of detection of ventricular arrhythmias. In children, the level of intraerythrocyte magnesium increased, which was accompanied by a decrease in the severity of clinical manifestations of autonomic dysfunction. After 6 months from the start of using magnesium orotate, complaints decreased in more than half of the patients, and mitral regurgitation decreased in 33% of patients. An antiarrhythmic effect was also noted among the majority of patients [23].
The use of Magnerot® is also indicated for pregnant women. A relative deficiency of magnesium ions not only leads to an increased risk of developing tachyarrhythmias, but also increases the incidence of gestosis, fetoplacental insufficiency, miscarriage, and discoordinated labor. The use of OM increases the bioavailability of pure magnesium without exposing the mother and fetus to additional exposure to other substances. The inclusion of Magnerot® in complex therapy of pregnant women with MVP led to normalization of neuromuscular conduction and myocardial contractility, increased resistance to stress and improved uteroplacental blood flow [24].
One of the important indications for prescribing magnesium orotate is the correction of the proarrhythmogenic effects of class I and III antiarrhythmic drugs. Due to its ability to prevent excess calcium entry into cardiomyocytes, Magnerot® is also recommended for use to correct the toxic effects of cardiac glycosides. In patients receiving cardiac glycosides, serum magnesium levels should be monitored and, as necessary, magnesium orotate should be prescribed to such patients for prophylactic purposes [21].
When analyzing Holter ECG monitoring parameters during Magnerot® therapy, a decrease in the maximum heart rate, a decrease in episodes of supraventricular and especially ventricular extrasystole, tachy- and bradycardia were revealed. Treatment with Magnerot® also showed a decrease in the number of patients with late ventricular potentials, which are a marker of an increased risk of developing ventricular extrasystole and tachycardia, and a decrease in endothelial dysfunction [13, 20, 21, 25].
The prescription of Magnerot® is also justified in the following clinical situations (as a component of combination therapy):
• combination of arterial hypertension with hyperlipidemia and manifestations of myocardial ischemia, including in patients with diabetes mellitus;
• heart rhythm disturbances due to chronic alcohol intoxication and chronic stress [20];
• chronic heart failure.
Currently, there is no solid evidence of the positive effect of Magnerot® on echocardiographic parameters of patients with chronic heart failure, but there is no negative effect on indicators of central hemodynamics, contractility, remodeling and left ventricular myocardial mass.
At the same time, in patients who did not receive Magnerot®, there was a significant deterioration in many echocardiogram parameters: a decrease in ejection fraction, an increase in the end-diastolic and end-systolic dimensions of the left ventricle. There was also a decrease in such indicators of central hemodynamics as stroke volume, stroke and systolic indices. It has been established that with the use of Magnerot® there is an improvement in the quality of life of patients with chronic heart failure, and the relative risk of death is significantly reduced [13].
Almost all researchers note the good tolerability of Magnerot® and the extremely rare occurrence of any unwanted side effects when using it [9, 20].
Thus, magnesium deficiency is a pressing problem today and can lead to both NRS and many other pathological conditions. To correct it, it is necessary to use drugs that have proven their high clinical effectiveness and good tolerability.
Such a drug is Magnerot®, which has cardioprotective properties. Magnerot® is one of the main means of treatment and prevention of cardiac arrhythmias and a good addition to complex pharmacotherapy of other cardiovascular pathologies.
Magnesium deficiency?
Magnesium is among the top most popular dietary supplements. There are at least three reasons for this.
- This metal really plays a very important role in the life of the body. It is needed by mitochondria to produce energy. Neurons - for transmitting electrical impulses. Cell ribosomes - for protein synthesis. With its help, damaged DNA molecules are restored, muscles contract and cholesterol is removed. Magnesium is involved in 500+ intracellular biochemical reactions and activates 300+ enzymes. And at the same time it is not produced inside the body. This means that we depend on its supply from the outside.
- According to frequently cited information, about 30% of Russians receive less than 70% of their daily dose of magnesium. But don't panic! We have found the original epidemiological study and hasten to reassure: it is not about all Russians, but only about 2,000 patients from several clinics.
- Anyone can suspect magnesium deficiency, even if a standard plasma or serum test shows that everything is normal. The catch is that 99% of magnesium is found inside cells (about 60% in bone tissue, the rest in muscles, brain, kidneys and liver), from where it is released into the blood when necessary to maintain optimal concentrations. So a normal level of magnesium in the blood does not exclude its deficiency at the cellular level. Therefore, popular health publications often advise focusing on external signs of deficiency. And there are so many of them (from apathy and high blood pressure to irritability and caries) that making a “diagnosis” is as easy as shelling pears.
The true diagnosis of magnesium deficiency is a battery of tests, including ECG, myography, bone density testing, saliva, urine, nails and hair analysis. Therefore, even if your legs often cramp, goosebumps appear, or your eyelid twitches (these are the most characteristic signs of magnesium deficiency), only a specialist can determine the real cause.
Transdermal magnesium
Despite all the efforts of manufacturers, the bioavailability of magnesium from dietary supplements remains quite low. Hence the idea of delivering it to the body in other ways. For example, through the skin.
Creams and sprays
And also gels, soaps, oils and lotions, mainly with magnesium chloride (it has the second highest concentration of magnesium after oxide - 30%). American naturopath Norman Shealy was the first to speak about their effectiveness. In 2005, he published a comparison table that showed that by rubbing magnesium cream into the skin, you can correct the deficiency much faster than using nutritional supplements (in a month and a half, rather than in six months). It is this research that is usually meant when it is repeated like a mantra that magnesium is absorbed better through the skin. The problem is that there is no study - only a short abstract with conclusions is available. But several screening tests with animals and people did not confirm them. Apparently, the author rubbed in not only magnesium. So a large review of current research on this topic does not recommend transdermal use.
Magnesium baths
This practice dates back to the 18th century, when a resort with unusual mineral water opened in the English town of Epsom - a natural solution of Epsom salts (magnesium sulfate). Now this mixture is credited with various healing properties: it helps to relax and lose weight, relieves pain, and among the most toxic, it “removes toxins.” But initially it was believed that it simply had a laxative effect, which is closer to the truth: taking capsules or tablets with magnesium sulfate sometimes causes diarrhea.
The only study on the effects of magnesium baths was conducted in England, involving 19 students at the University of Birmingham. They lay in a solution of magnesium sulfate (1 g/100 ml) for 12 minutes a day at temperatures up to 55 degrees. At the end of the study, the majority of subjects had increased magnesium concentrations in their blood, although only slightly. This did not affect their health in any way. But questions remain.
Magnesium molecules are small enough to penetrate the skin barrier. Magnesium ions labeled with fluorescent markers actually penetrate into the top layer of the skin, using the openings of the hair follicles as a loophole. But for the cellular absorption of magnesium, special transport channels are needed, and they are not present in the skin. How could magnesium get into the blood of students? There are several assumptions. The first is boring, but the most plausible: through the lungs with steam. The second is much more fun: thanks to the absorption of magnesium ions by the mucous membrane of the anus. In the same way, the body could absorb alcohol from a hot bath. But, as Paul Ingram rightly notes, if you really want to take magnesium (or alcohol), then it’s more pleasant and easier to do it by mouth.