Etiology of mitral regurgitation:
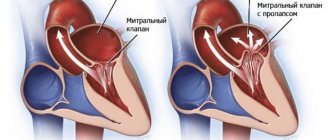
- Congenital pathology: cleft valve, prolapse, etc.
- Ischemic mitral valve dysfunction in ischemic heart disease.
- Degenerative processes: myxomatous degeneration, Marfan and Ehlers-Danlos syndromes, mitral annulus calcification.
- Inflammatory lesions: rheumatism, systemic lupus erythematosus, systemic scleroderma, aortoarteritis.
- Infection: infective endocarditis.
- Injury.
According to the course, mitral regurgitation is divided into chronic and acute and, accordingly, requires a different approach when determining the indications for the urgency of surgical intervention.
Correction of chronic mitral regurgitation must be carried out before left ventricular decompensation develops, taking into account echocardiography criteria for assessing the severity of mitral regurgitation. The development of acute mitral regurgitation, refractory to drug therapy, is an indication for emergency surgery.
The manifestation of clinical symptoms of mitral regurgitation is determined by the severity of mitral valve insufficiency and the functional state of the left ventricle.
Short description
Mitral regurgitation is the inability of the left atrioventricular valve to prevent the reverse flow of blood from the left ventricle into the left atrium during ventricular systole.
Code according to the international classification of diseases ICD-10:
- I05.1 Rheumatic mitral valve insufficiency
- I05.2 Mitral stenosis with insufficiency
- I34.0 Mitral (valve) insufficiency
- Q23.3 Congenital mitral regurgitation
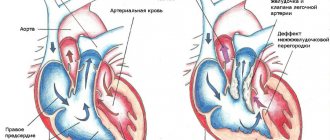
Frequency. Mitral insufficiency is recorded in 50% of patients with various heart defects. In its pure form, mitral regurgitation is a rare disease. It is observed much more often in children than in adults. Often combined with mitral stenosis or aortic valve defects. Congenital mitral valve insufficiency accounts for 0.6% of all congenital heart diseases. In 65% of cases it is combined with septal defects, coarctation of the aorta or patent ductus arteriosus. About 5–6% of healthy women have some degree of mitral regurgitation detected by echocardiography.
Symptoms
The most typical complaint is shortness of breath, which occurs with moderate and severe chronic mitral regurgitation and the clinic of acute left ventricular failure with acute mitral regurgitation. The presence of atrial fibrillation before surgery is an independent predictor of reduced long-term survival after mitral valve surgery for chronic mitral regurgitation.
Symptoms (signs)
Clinical picture and diagnosis . • During chronic mitral regurgitation, three periods are conventionally distinguished: compensation, pulmonary venous hypertension and right ventricular failure. • Complaints •• During the compensation period, an asymptomatic course can be observed for several years •• When clinical symptoms appear in patients, the most common complaints are shortness of breath (98%), fatigue (87%), hemoptysis (15%) •• With severe regurgitation there are symptoms of compression of the recurrent laryngeal nerve by the enlarged left atrium (the most common of them is Ortner's syndrome - hoarseness of voice), and during the period of right ventricular failure - by the pulmonary trunk •• In patients in the third stage - symptoms of stagnation in the systemic circulation (edema, enlarged liver, Plesch's sign, swelling of the jugular veins).
• Peripheral symptoms are due to small output syndrome - see Aortic valve insufficiency. • Valve symptoms •• Mesosystolic click occurs with mitral valve prolapse, separation of chords or papillary muscle •• Weakening of the first tone •• Systolic murmur over the apex of various timbres, carried out to Botkin’s point and the left axillary region; its intensity depends on the volume of regurgitation •• The most specific sign of a mitral regurgitation murmur is intensification or appearance during tests that reduce the volume of the left ventricle (Valsalva maneuver, orthostatic test), or in a clinostatic position when turning to the left side due to the closer location of the apex of the heart to the chest •• Systolic flutter over the apical region - with high velocity (usually a thin jet) of regurgitation •• Coombs' murmur occurs due to relative stenosis of the mitral valve due to an increased volume of blood expelled from the left atrium.
• Symptoms associated with enlargement of the chambers of the heart • Increase in the boundaries of relative dullness to the left, up and to the right (with dilatation of the right sections) • Popov's symptom - different degrees of filling of the pulse in the radial arteries. • Symptoms of the underlying disease (rheumatism, Marfan syndrome, cardiomyopathy).
Diagnosis of mitral insufficiency
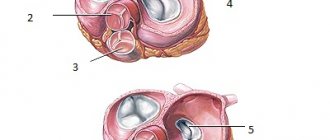
Echocardiography (ECHOCG)
occupies a leading place in the diagnosis of mitral valve insufficiency and determination of indications for patient management tactics. If transthoracic echocardiography is insufficiently informative and the possibility of reconstructive surgery on the mitral valve is clarified, transesophageal echocardiography should be performed.
Echocardiography allows you to determine the etiology of mitral regurgitation, its severity - the compensatory capabilities of the left ventricle, the presence of complications (left ventricular failure, pulmonary hypertension, right ventricular failure), and identify other heart defects.
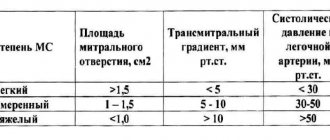
An echocardiography study allows one to assess the degree of mitral valve insufficiency based on the ratio of the area of regurgitation flow to the area of the left atrium:
- Minor mitral valve insufficiency less than 20%
- Moderate deficiency 20-40%
- Severe deficiency 40%
If ischemic heart disease is not the cause of mitral regurgitation and there is no evidence of concomitant ischemic heart disease, indications for surgery can be determined without cardiac catheterization.
The use of invasive examination methods is indicated for patients with ischemic mitral valve dysfunction:
Coronary angiography makes it possible to clarify the presence of stenotic lesions of the coronary arteries and determine indications for myocardial revascularization in combination with surgical correction of mitral regurgitation.
Indications for surgical treatment of mitral insufficiency
Classification of recommendations and levels of evidence in ACC/AAC format:
- Class I: Conditions for which there is evidence and/or general agreement that a procedure or treatment is beneficial, useful and effective.
- Class II: Conditions for which there is conflicting evidence and/or differences of opinion about the usefulness/efficacy of a procedure or treatment.
- Class IIA: Weight credibility/opinion in favor of usefulness/effectiveness.
- Class IIB: Benefit/effectiveness less well established by evidence/opinion.
- Class III: Conditions for which there is evidence and/or general consensus that the procedure/treatment is not beneficial, not effective, and in some cases may be harmful.
In addition, the levels of evidence to support the recommendations are outlined as follows:
- Level of Evidence A: Data are from multiple randomized clinical trials.
- Level of Evidence B: Data are from single randomized trials or non-randomized trials.
- Level of Evidence C: Expert consensus only, individual case studies and standards of care.
Diagnostics
Special studies • ECG •• Signs of hypertrophy and overload of the left parts of the heart, primarily the left atrium, and in the third stage of the disease and the right parts of the heart •• Supraventricular tachyarrhythmias (atrial fibrillation and flutter, supraventricular extrasystole and tachycardia).
• X-ray of the chest organs •• Pronounced signs of pulmonary venous hypertension • Bulging of the arch of the left atrium and deviation of the contrasted esophagus along an arc of a large radius •• Bulging of the arch of the left ventricle •• In the third stage of the disease - signs of pulmonary hypertension and bulging of the arches of the right parts of the heart •• With compression of the pulmonary trunk by the dilated left atrium - weakening of the pulmonary pattern on the left •• With fluoroscopy in direct projection - a symptom of a “rocker arm” between the arches of the left ventricle and the left atrium.
• Echocardiography •• Hypertrophy and dilatation of the left heart, especially the left atrium •• Visualization of a flapping leaflet when the chordae or papillary muscle is avulsed •• Increased end-diastolic index (EDI = [end-diastolic volume of the left ventricle] / [body surface area]), degree which has prognostic significance: an increase in CDI above 30 ml/m2 is associated with postoperative left ventricular failure, above 90 ml/m2 - with high postoperative mortality •• In Doppler mode - the flow of mitral regurgitation, the volume of which (estimated in the color mapping mode) corresponds to the degree severity of the defect •• In the third stage of the disease - hypertrophy and dilation of the right heart, increased systolic pressure in the right ventricle •• Transesophageal echocardiography is performed to detect thrombosis of the left atrium in the presence of atrial fibrillation.
• Catheterization of the left and right ventricles •• Increase in end-diastolic pressure of the left ventricle, pressure in the left atrium, systolic pressure in the right atrium, pulmonary artery wedge pressure •• “Ventriculization” of the pulmonary capillary pressure curve (increase in wave V more than 15 mm Hg. ).
• Left ventriculography •• The presence and degree of regurgitation is determined by the degree of filling of the left atrium in one contraction with contrast injected into the left ventricle •• Combined valvular lesions are also diagnosed.
Surgical treatment of mitral valve insufficiency
CLASS I
- 1. Patients with acute severe mitral regurgitation (Level of Evidence: B)
- 2. Patients with chronic severe mitral valve insufficiency and NYHA class II, III, IV heart failure, in the absence of severe LV dysfunction (severe LV dysfunction is defined as an ejection fraction less than 30%) and/or ESR greater than 55 mm. (Confidence level: B)
- 3. Asymptomatic patients with chronic severe mitral regurgitation and mild to moderate LV dysfunction, ejection fraction 30-60% and/or ESR greater than or equal to 40 mm. (Confidence level: B)
- 4. Mitral valve repair is preferred over mitral valve replacement in most patients with severe chronic mitral regurgitation who require surgery, and patients should be referred to surgical centers with extensive experience in MV repair. (Confidence level: C)
CLASS IIA
- 1. MV repair is indicated in asymptomatic patients with severe chronic mitral regurgitation and normal LV function (ejection fraction greater than 60% and ejection fraction less than 40 mm), in whom the probability of good results of valve repair is greater than 90%. (Confidence level: B)
- 2. Intervention on MV is indicated in asymptomatic patients with severe chronic mitral regurgitation with normal LV function and paroxysmal atrial fibrillation. (Confidence level: C)
- 3. Intervention on MV is indicated in asymptomatic patients with severe chronic mitral regurgitation with preserved LV function and pulmonary hypertension (systolic PA pressure more than 50 mm Hg at rest or more than 60 mm Hg during exercise). (Confidence level: C)
- 4. Intervention on MV is indicated in patients with severe chronic MR*, which developed as a result of primary pathology of the mitral structures, symptoms of NYHA class III-IV and severe LV dysfunction (ejection fraction less than 30% or ESR more than 55 mm), for whom restoration is more suitable MK. (Confidence level: C)
CLASS IIB
- Mitral valve repair is possible in patients with chronic severe mitral valve regurgitation due to severe LV dysfunction (ejection fraction less than 30%), who, despite optimal HF therapy, including a biventricular pacemaker, have symptoms of NYHA class III-IV. (Confidence level: C)
CLASS III
- 1. Mitral valve intervention is not indicated for asymptomatic patients with mitral regurgitation and normal LV function (ejection fraction more than 60% and ejection fraction less than 40 mm), who have significant doubts about the possibility of MV repair. (Confidence level: C)
- 2. Isolated MV surgery is not indicated for patients with mild or moderate mitral regurgitation. (Confidence level: C)
In many cases, the type of operation—plasty or prosthetic valve replacement—is important in choosing the timing of the operation. Although the type of surgical intervention is never actually determined before surgery, in many cases the choice of surgical intervention can be determined in advance. Mortality during planned operations for mitral regurgitation after mitral valve replacement is 2–7%, after mitral valve repair 1–4%. Currently, three main methods of correcting mitral regurgitation are used: valve plastic surgery, mitral valve replacement with partial or complete preservation of the chordal apparatus, and mitral valve replacement without preservation of the chordal apparatus. In most cases, valve repair is the procedure of choice and should be performed whenever possible.
Timely surgical intervention allows one to achieve good results in surgical correction of heart defects, reduces the degree of surgical risk and improves long-term results of surgical treatment.
Publications in the media
Mitral regurgitation is the inability of the left atrioventricular valve to prevent the reverse flow of blood from the left ventricle into the left atrium during ventricular systole.
Frequency. Mitral insufficiency is recorded in 50% of patients with various heart defects. In its pure form, mitral regurgitation is a rare disease. It is observed much more often in children than in adults. Often combined with mitral stenosis or aortic valve defects. Congenital mitral valve insufficiency accounts for 0.6% of all congenital heart diseases. In 65% of cases it is combined with septal defects, coarctation of the aorta or patent ductus arteriosus. About 5–6% of healthy women have some degree of mitral regurgitation detected by echocardiography.
Etiology • Rheumatism • Isolated mitral valve prolapse (myxomatous degeneration, Barlow's disease) • Idiopathic rupture of chordae (14–23% of cases of severe insufficiency, of which degenerative changes of the chordae are detected in 73–93% of cases) • Ischemic dysfunction or rupture of papillary muscles (5 % cases of transmural MI, more often with lower MI) • Infective endocarditis • Annular calcification of the elderly • Connective tissue diseases (Marfan and Ehlers-Danlos syndrome) • Complication of mitral valvuloplasty • Relative failure due to dilatation or submitral aneurysm of the left ventricle • Congenital forms of failure (e.g. due to splitting of the anterior leaflet of the mitral valve with a fully open AV canal).
Pathophysiology • Hemodynamics in acute regurgitation are significantly different from those in the chronic course of the disease, when compensatory hypertrophy and dilatation of the left ventricle, the degree of which depends on the severity of mitral regurgitation, maintain cardiac output, sometimes for many years • In acute mitral regurgitation (for example, due to rupture of the papillary muscle or chordae) the left ventricle does not have time to adapt to a sharp increase in preload. As a result of this, and also due to the low compliance of the normal left atrium, acute left ventricular failure occurs, leading to pulmonary edema and arterial hypotension • With chronically existing regurgitation, due to an increase in the volume load of the left atrium, its hypertrophy and dilation occurs, more pronounced than with mitral stenosis, leading to chronic stagnation in the pulmonary circulation • Often, with dilatation of the left atrium, paroxysmal or permanent form of atrial fibrillation occurs, as well as thrombosis of the left atrium.
Clinical picture and diagnosis . • During chronic mitral regurgitation, three periods are conventionally distinguished: compensation, pulmonary venous hypertension and right ventricular failure. • Complaints •• During the compensation period, an asymptomatic course can be observed for several years •• When clinical symptoms appear in patients, the most common complaints are shortness of breath (98%), fatigue (87%), hemoptysis (15%) •• With severe regurgitation there are symptoms of compression of the recurrent laryngeal nerve by the enlarged left atrium (the most common of them is Ortner's syndrome - hoarseness of voice), and during the period of right ventricular failure - by the pulmonary trunk •• In patients in the third stage - symptoms of stagnation in the systemic circulation (edema, enlarged liver, Plesch's sign, swelling of the jugular veins).
• Peripheral symptoms are due to small output syndrome - see Aortic valve insufficiency. • Valve symptoms •• Mesosystolic click occurs with mitral valve prolapse, separation of chords or papillary muscle •• Weakening of the first tone •• Systolic murmur over the apex of various timbres, carried out to Botkin’s point and the left axillary region; its intensity depends on the volume of regurgitation •• The most specific sign of a mitral regurgitation murmur is intensification or appearance during tests that reduce the volume of the left ventricle (Valsalva maneuver, orthostatic test), or in a clinostatic position when turning to the left side due to the closer location of the apex of the heart to the chest •• Systolic flutter over the apical region - with high velocity (usually fine jet) regurgitation •• Coombs murmur occurs due to relative stenosis of the mitral valve due to the increased volume of blood expelled from the left atrium.
• Symptoms associated with enlargement of the chambers of the heart • Increase in the boundaries of relative dullness to the left, up and to the right (with dilatation of the right sections) • Popov's symptom - different degrees of filling of the pulse in the radial arteries. • Symptoms of the underlying disease (rheumatism, Marfan syndrome, cardiomyopathy).
Special studies • ECG •• Signs of hypertrophy and overload of the left parts of the heart, primarily the left atrium, and in the third stage of the disease and the right parts of the heart •• Supraventricular tachyarrhythmias (atrial fibrillation and flutter, supraventricular extrasystole and tachycardia).
• X-ray of the chest organs •• Pronounced signs of pulmonary venous hypertension • Bulging of the arch of the left atrium and deviation of the contrasted esophagus along an arc of a large radius •• Bulging of the arch of the left ventricle •• In the third stage of the disease - signs of pulmonary hypertension and bulging of the arches of the right parts of the heart •• With compression of the pulmonary trunk by the dilated left atrium - weakening of the pulmonary pattern on the left •• With fluoroscopy in direct projection - a symptom of a “rocker arm” between the arches of the left ventricle and the left atrium.
• Echocardiography •• Hypertrophy and dilatation of the left heart, especially the left atrium •• Visualization of a flapping leaflet when the chordae or papillary muscle is avulsed •• Increased end-diastolic index (EDI = [end-diastolic volume of the left ventricle] / [body surface area]), degree which has prognostic significance: an increase in CDI above 30 ml/m2 is associated with postoperative left ventricular failure, above 90 ml/m2 - with high postoperative mortality •• In Doppler mode - the flow of mitral regurgitation, the volume of which (estimated in the color mapping mode) corresponds to the degree severity of the defect •• In the third stage of the disease - hypertrophy and dilation of the right heart, increased systolic pressure in the right ventricle •• Transesophageal echocardiography is performed to detect thrombosis of the left atrium in the presence of atrial fibrillation.
• Catheterization of the left and right ventricles •• Increase in end-diastolic pressure of the left ventricle, pressure in the left atrium, systolic pressure in the right atrium, pulmonary artery wedge pressure •• “Ventriculization” of the pulmonary capillary pressure curve (increase in wave V more than 15 mm Hg. ).
• Left ventriculography •• The presence and degree of regurgitation is determined by the degree of filling of the left atrium in one contraction with contrast injected into the left ventricle •• Combined valvular lesions are also diagnosed.
TREATMENT • Drug therapy •• Chronic mitral regurgitation ••• Asymptomatic mild and moderate mitral regurgitation does not require treatment, and the advisability of taking vasodilators is controversial ••• Asymptomatic severe compensated regurgitation (CDI less than 50 ml/m2, absence of pulmonary hypertension and normal left ventricular systolic function , negative stress tests): invasive studies of hemodynamics at rest and during stress tests are indicated, as well as continuous use of ACE inhibitors •• Acute mitral regurgitation ••• Vasodilators (sodium nitroprusside or ACE inhibitors) and IV diuretics ••• Intra-aortic balloon counterpulsation ••• In case of infective endocarditis, absence of progression of sepsis or severe refractory heart failure, preoperative antibiotic therapy is permissible for no longer than 3 days ••• In case of severe failure due to MI without rupture of the papillary muscles - intra-aortic balloon counterpulsation, vasodilators.
• Surgical treatment •• Indications ••• Severe mitral regurgitation, asymptomatic or functional class II, if the end-diastolic size of the left ventricle is more than 40 mm or the CDI is more than 40 ml/m2, or the left ventricular ejection fraction is less than 55–60% (with mitral insufficiency, if the contractile function of the left ventricle is not impaired, the left ventricular ejection fraction should not be lower than 65%) ••• Severe mitral regurgitation, functional class III–IV ••• Severe asymptomatic mitral regurgitation in combination with severe pulmonary hypertension ••• Symptomatic moderate failure with preserved systolic function of the left ventricle in case of positive results of an invasive hemodynamic study •• Contraindications ••• Severe concomitant pathology that threatens the patient’s life ••• End-stage circulatory failure ••• Negative test result with aminophylline and oxygen •• Methods of surgical treatment ••• In the absence of calcification and preserved mobility of the leaflets and valve apparatus, it is permissible to perform valve-sparing interventions (annuloplasty with the Alain Carpentier ring or using the “double hole” technique, excision of the flapping portion of the posterior leaflet, shortening of the chordae) ••• Despite the greater physiology of valve-sparing operations and relatively low incidence of thrombosis and infective endocarditis, due to the high frequency of relapses of the defect and the need for repeated operations, plastic interventions on the valves are actually performed only in cases of prolapse, ruptures of valve structures, relative valve insufficiency during dilatation of its ring and before a planned pregnancy ••• Mitral valve replacement valves under conditions of artificial circulation using biological prostheses are performed on children or before a planned pregnancy ••• In other cases, the affected valve is replaced with a mechanical prosthesis.
Specific postoperative complications • Thromboembolism • Secondary infective endocarditis of prostheses • Atrioventricular block • Dystrophic changes in biological prostheses and the need for repeated prosthetics. Prognosis • Only 5–10% of patients with mitral valve prolapse progress to mitral regurgitation • 5-year survival rate is more than 80%, 10-year survival rate is more than 60% • With ischemic genesis of the defect, 5-year survival rate does not exceed 30% • Surgical treatment improves survival and exercise tolerance if the initial left ventricular ejection fraction is more than 35%, cardiac index is more than 1.5 ml/min/m2 • Surgical treatment is ineffective for secondary mitral regurgitation due to dilated cardiomyopathy and primary - for left ventricular ejection fraction less than 30% • Surgical treatment is often effective for ischemic cardiomyopathy when coronary artery bypass grafting and annuloplasty are performed simultaneously • Mortality with mitral valve replacement is 2-7%, with annuloplasty - 1-4% • 5-year survival rate averages 90%.
Synonyms • Left atrioventricular valve insufficiency • Mitral valve insufficiency
Abbreviations. EDI - end diastolic index.
ICD-10 • I05.1 Rheumatic mitral valve insufficiency • I05.2 Mitral stenosis with insufficiency • I34.0 Mitral (valve) insufficiency • Q23.3 Congenital mitral insufficiency