Heart valves and their defects
The heart has four chambers: two atria and two ventricles. From the atria, blood enters the ventricles, and then through the valves, with the help of contractions of the heart muscle, enters the arteries. Valves ensure blood flow in the desired direction and quantity. If they close or do not open completely, this prevents normal blood circulation.
As a result, the heart gradually increases in volume and stretches, compensating for blood deficiency and working under constant overload. Exhaustive work of the heart can cause the development of serious cardiovascular diseases, such as arrhythmia or heart failure. In addition, heart valve defects can cause complications due to certain ongoing infectious diseases.
Most often, heart defects are diagnosed in patients over sixty years of age. The reason is that with age, the valves of the valve apparatus lose their elasticity, and the heart increases in size. As a result, blood flow decreases and it unevenly fills the cavities of the heart - heart failure develops.
There are four types of heart valves, and each has a specific function:
- Aortic : prevents blood from flowing from the aorta into the left ventricle of the heart.
- Mitral : prevents the flow of blood from the left ventricle of the heart into the left atrium at the moment when the heart muscle contracts and blood is pushed into the vessels.
- Pulmonary : Prevents the flow of blood from the pulmonary artery into the right ventricle of the heart.
- Tricuspid : valve between the right ventricle of the heart and the right atrium.
If the valves are enlarged, narrowed, loose or torn, it becomes difficult for them to close, and blood flows back with each contraction of the heart. As a result, the heart experiences enormous stress and eventually loses its performance.
Depending on the form of the disease, heart valve defects can manifest as:
- stenosis – narrowing of the lumen (opening) of the vessels through which blood flows. This significantly increases the load on the heart, as it makes it more difficult for blood to be pumped out.
- insufficiency - damage to the heart valve leaflets, resulting in their inability to close completely. In such cases, the blood flows back.
- a combination of stenosis and insufficiency - the affected valves form an obstacle to the passage of blood. In this case, some of the blood passes through the hole, but returns back into the next phase of the cardiac cycle.
Prevention
Prevention of PPS involves treating the underlying disease that caused the valve damage. To prevent the development of defects, a cardiotrophic diet and lifestyle correction are additionally prescribed:
- refusal of salty, spicy, fatty foods;
- complete cessation of smoking and drinking alcohol;
- moderately active lifestyle;
- control of infectious diseases, including colds;
- annual monitoring by a cardiologist.
All prescriptions and dietary adjustments must be prescribed by your doctor during the treatment process. In our center, the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, several programs have been developed that will help identify whether you have a heart defect and determine the method of its treatment. You can learn more about the programs here.
Causes and symptoms
Heart valve defects can be congenital or acquired. The main causes of the development of heart valve defects are rheumatism, infections, myocardial and cardiovascular diseases.
Congenital heart valve defects develop before birth and depend on how the pregnancy progressed. Congenital heart valve defects are an extremely rare diagnosis, diagnosed only in 1% of cases. Congenital defects include defects of the aortic and pulmonary valves, which are treated by surgical intervention in the first years of the patient’s life.
Purchased . Acquired heart valve defects include transformations of the valve structure due to infections, inflammation, previous heart attacks, etc. Most of them arise as a result of a gradual change in the structure of the heart; in some cases, rheumatism leads to the defect. All congenital and acquired defects have related symptoms that can appear at any age:
- increased heart rate,
- dyspnea,
- swelling,
- other manifestations of heart failure.
Initially, they appear during physical activity, but as pathologies develop, they will begin to appear in a calm state. Among the types of heart valve defects, mitral valve prolapse is the most common. It occurs during heart contractions when the valve leaflets in the left atrium sag. The walls of the valve lose elasticity and it “leaks”. Prolapse can be primary or secondary:
- Primary prolapse refers to congenital valve defects. Connective tissue pathologies in this case are a genetic predisposition.
- Secondary prolapse is an acquired defect. It occurs due to chest injury, rheumatism or myocardial infarction.
Prolapse does not have serious health consequences, and its symptoms do not interfere with life. However, they may not appear for a long time and most often bother people in old age, which is why they are written off as “age-related.” If you do not pay attention to the symptoms in time, complications may arise, such as arrhythmia and heart failure.
Symptoms also include complaints of pain in the heart area. They arise against the background of anxiety, are not associated with physical activity and are not relieved with medication. The pain is not intense, but long-lasting, accompanied by anxiety and rapid heartbeat.
Mitral stenosis
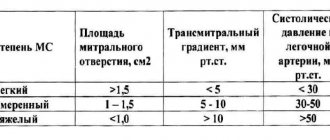
This defect is characterized by a narrowing of the valve opening. The “critical” value of the area is 1–1.5 cm. The smaller the area, the more symptoms of the disease.
Mitral stenosis can lead to
- rheumatic fever;
— calcium deposits on the valve leaflets;
— connective tissue diseases (Marfan syndrome);
— myxoma (benign tumor) of the left atrium.
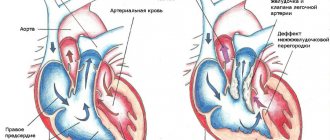
Rice.
1 - tricuspid valve;
2 - aortic valve;
3 - pulmonary valve;
4 - mitral valve;
5 - stenosis of the mitral valve opening.
Through the narrowed mitral orifice, blood from the left atrium to the left ventricle passes with difficulty: the atrium has to work harder and harder to push the blood. This increased work leads to an enlargement of the atrium. Blood stagnation in the lungs gradually develops, and over time the right parts of the heart also enlarge. An enlarged heart works worse, and heart failure develops.
Symptoms
At the initial stages, stenosis does not make itself felt. People feel completely healthy and can perform significant physical activity. As the defect progresses, shortness of breath (blood stagnation in the lungs) appears, at first only when moving, later at rest. Around the same time, a cough with a small amount of sputum may appear; Sometimes hemoptysis is observed. There is unmotivated weakness, rapid fatigue, a feeling of interruptions in the heart, diffuse chest pain. In advanced cases, an enlarged heart can put pressure on the esophagus and larynx - the voice changes and swallowing is impaired.
Diagnostics
People with mitral stenosis are characterized by a specific appearance: a pale face, sharply defined rosy cheeks with a bluish tint, cyanosis of the lips and tip of the nose. On the anterior chest there is a cardiac hump - this is how the enlarged heart sticks out. The pulse is not the same in the arms. With a thorough examination by a doctor, as a rule, there is no doubt about the diagnosis, because heart sounds and changes in clinical and laboratory data are specific changes that are difficult to confuse with other conditions.
Treatment
In the initial stages of development, some medications are used to help improve the functioning of the heart. In later stages and with the progression of the disease, treatment is carried out surgically: dissection of the fused valve leaflets or replacement with an artificial valve.
Prevention
The cause of mitral stenosis in almost half of the cases is rheumatic fever (the old name is rheumatism). You can get it if you do not properly treat a common sore throat (although not all people who have had a sore throat get rheumatism!), caused by streptococcus - it also causes rheumatic damage to the heart valves. The defect can be prevented by proper treatment of sore throat under the supervision of a physician, with the use of antibiotics and subsequent control ECG registrations.
Diagnosis and treatment
If you or your loved ones are experiencing the symptoms described above, we recommend getting tested. During diagnosis, the doctor monitors heart parameters at rest and during exercise.
The patient is prescribed:
- daily ECG monitoring,
- echocardiography (ECHO-CG),
- chest x-ray,
- CT and MRI using special equipment that allows you to examine the heart virtually between beats.
Such diagnostics are carried out not only during the initial examination of patients with suspected disease, but also in dispensary groups of patients with an already confirmed diagnosis.
Depending on the diagnostic results, the doctor prescribes the necessary treatment: therapy or surgery.
- Therapy is aimed at preventing, preventing and alleviating relapses of the disease that became the root cause of the defect, as well as treating heart failure.
- Surgical intervention is an extreme necessity, which due to age or complications may not be prescribed for all patients.
Typically, heart valve disease is a mechanical problem that can only be solved with surgery performed by a surgeon. For stenosis, an operation is indicated to separate the fused valve leaflets and widen the atrioventricular opening - commissurotomy. If there is insufficiency, prosthetics are performed: replacement with a biological or mechanical analogue.
How to treat acquired heart disease
Treatment of acquired heart defects is a comprehensive approach, including drug treatment, a special diet, and lifestyle adjustments. If conservative treatment is not enough, surgical intervention is resorted to.
When you contact the center of the Federal Scientific and Clinical Center of FMBA, our doctors will quickly diagnose your disease and prescribe therapeutic treatment. The center has a therapeutic department, where you will be under the constant supervision of specialists. If after the examination it is determined that surgical correction is needed, you will be referred for a consultation with a cardiac surgeon, who will determine whether you need surgery.
Surgical methods:
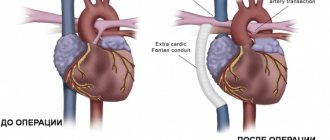
- Catheter balloon valvuloplasty is the expansion of a narrowed lumen by inserting a balloon catheter. As a result of the operation, the fusion between the valve leaflets is separated, and the obstruction to blood flow is eliminated;
- Valvotomy (commissurotomy) – dissection of fused valves;
- Valve replacement is the replacement of a damaged valve with an implant. Open heart surgery using a machine that temporarily replaces the work of the heart;
- Percutaneous aortic valve replacement.
The main thing in treatment is timely diagnosis. Don’t put off your health for later, seek advice right now.
Infectious and prosthetic endocarditis.
The etiology of infective endocarditis has changed significantly due to the active use of antibiotics throughout the world. Currently, the main role is given to staphylococci and gram-negative flora, as well as fungal infections.
From the point of view of surgery, in the pathogenesis of infective endocarditis, the fact of rapid destruction of the valvular apparatus of the heart is of greatest importance. This leads to a catastrophic increase in heart failure, since the myocardium does not have time to adapt to the sudden disruption of hemodynamics. The decision on the need for surgical treatment arises, as a rule, with the development of “complicated infective endocarditis”: changes in hemodynamic status; persistence and prevalence of infection; development of metastatic foci of infection; systemic embolisms. In these cases, surgical treatment is more successful than a therapeutic approach. The main problem of surgical treatment is to prevent recurrence of infection and the development of prosthetic endocarditis. The basis for the choice of tactics is the anatomical changes identified on the operating table: the degree of damage to the fibrous ring and surrounding tissues, as well as the presence of vegetations, abscesses, fistulas, and prosthetic separations. In recent years, particular importance has been given to reconstructive operations, especially when the mitral or tricuspid valves are affected by endocarditis. To replace valve defects after surgical treatment, plastic surgery with one’s own tissue, auto- or xenopericardium is used.
Congenital heart defects
They are formed in utero. About 2% of children are born with various PS: from mild to severe, incompatible with life. The main reasons for their development:
- chromosomal abnormalities (Down syndrome, Patau);
- the effect of alcohol, nicotine, and drugs on the fetus;
- infection of the mother during pregnancy with rubella viruses, herpes simplex, chickenpox, cytomegalovirus, toxoplasma;
- maternal diabetes;
- exposure to radiation on a pregnant woman;
- taking certain medications during pregnancy (tetracycline, sulfonamide, antitumor antibiotics).
Symptoms of heart defects
Impaired hemodynamics (blood circulation) leads to a lack of blood supply to some organs and venous stagnation in others. The heart has to work harder to pump blood, it increases in size, this temporarily compensates for the pathology, symptoms do not appear. But over time, compensatory reserves are depleted, the heart muscle stretches, weakens and can no longer effectively perform its job.
This gives rise to a number of typical signs:
- shortness of breath (at the initial stages after physical activity, then at rest);
- dizziness, fainting;
- cyanosis of the nasolabial triangle, mucous membranes, fingertips;
- swelling in the legs (appears in the evening, disappears in the morning);
- symptom of “drumsticks” - club-shaped expansion of the fingertips (appears with a long course of the disease);
- rosy cheeks against a background of general pallor ー mitral face (with mitral stenosis).
If such symptoms appear, you should contact a cardiologist for further diagnosis.