directions
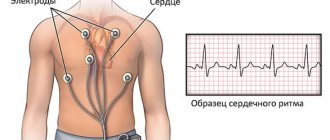
An electrocardiogram is a common non-invasive test to obtain data on the condition of the heart. The reason is general accessibility, simplicity, low cost of use and high information content. An ECG of the heart is a mandatory part of the examination at an appointment with a cardiologist, and is also used by therapists.
An ECG records changes in the heart and determines whether each of its major parts is functioning correctly. The study reveals arrhythmias, heart blocks, pathologies and disruptions in the functions of the heart muscle.
Prices for services
- Interpretation, description and interpretation of data from electrocardiographic studies (ECG) 220a
- Carrying out electrocardiographic studies (ECG) 880a
- Carrying out electrocardiographic studies (ECG) with a load of 1455a
- Appointment (examination, consultation) with a cardiologist + ECG 2070a
- Holter heart rate monitoring (Holter ECG) 2900a
The information and prices presented on the website are for reference only and do not constitute a public offer.
How is the examination carried out?
Typically, an ECG during pregnancy is carried out in a medical institution - a clinic, outpatient clinic, hospital. Since the machine itself that records the cardiogram is portable, this test can be performed almost anywhere.
During the examination:
- You will have to lie down on a couch or bed, exposing the chest, forearm and lower leg area.
- The healthcare professional applies a special gel to the skin of these areas that reduces electrical resistance.
- Electrodes are attached to the skin of the arms, legs and chest, which are connected to a machine that records the electrical activity of the heart on paper.
- During the test, you need to lie still and breathe normally. Sometimes your healthcare provider may ask you to take a deep breath and hold your breath. You cannot speak during the examination.
- You need to relax and not tremble, as any movement can affect the result.
- After recording is completed, the electrodes are removed from the skin and the gel is wiped off.
The duration of ECG recording rarely exceeds 10 minutes. After this, the electrodes are removed from the skin.
Our clinics in St. Petersburg
Structural subdivision of Polikarpov Alley Polikarpov 6k2 Primorsky district
- Pionerskaya
- Specific
- Commandant's
Structural subdivision of Zhukov Marshal Zhukov Ave. 28k2 Kirovsky district
- Avtovo
- Avenue of Veterans
- Leninsky Prospekt
Structural subdivision Devyatkino Okhtinskaya alley 18 Vsevolozhsk district
- Devyatkino
- Civil Prospect
- Academic
For detailed information and to make an appointment, you can call +7 (812) 640-55-25
Make an appointment
Method of measurement
This method is based on tracking the electrical potentials that occur with each heartbeat. Electrodes installed on the patient's body receive signals, conduct it to an electrocardiograph, which records the fluctuations and displays them on a display or paper.
The Nobel Prize was awarded in 1924 for the design of the first device for measuring the ECG of the heart, the details of decoding the electrocardiogram and the description of disturbances in the functioning of the heart. The basis of Willem Einthoven’s developments is also used in modern medicine.
Diseases that can be detected using an ECG
Registration of an ECG during pregnancy helps diagnose many heart diseases in expectant mothers. With this test, doctors can detect:
- fast or slow heartbeat;
- heart rhythm disturbances (arrhythmias);
- disturbances in the passage of electrical impulses in the heart (blockade);
- an increase in the size of the heart and thickening of its walls (hypertrophy);
- the cause of heart disease symptoms (eg, shortness of breath, heart pain, dizziness, fainting);
- signs of congenital heart defects in a pregnant woman;
- signs of electrolyte disturbances (increased or decreased levels of potassium, magnesium, calcium in the blood).
Technique for taking an ECG of the heart
To take an ECG, the patient is positioned in a horizontal or any other position convenient for him. His breathing should be calm, the electrode locations (wrists, ankles, chest) should be exposed. The skin of the subject is degreased at the places where the electrodes are applied; in some cases, electrode paste is used for better contact with the skin. From each sensor there is a marked wire that transmits information to the electrocardiograph.
According to the standard scheme, electrodes are placed on the intercostal spaces at the right and left edges of the sternum; along the left parasternal line; in the intercostal spaces along the left midclavicular line; along the left anterior and middle axillary lines. The doctor is required to correctly determine the location of the sensors and securely attach them to the patient’s body in order to avoid signal distortion.
The doctor sets the same amplification of the electrical signal, the speed mode for ECG recording, and other parameters in accordance with the patient’s age and weight.
The whole procedure takes 5-10 minutes . The short duration of the conduction is both an advantage and a disadvantage of the ECG. A 20-second recording is not always enough if a person suffers, for example, from arrhythmia. When data on the work of the heart is needed not at rest, but during the patient’s usual activities, they resort to Holter ECG monitoring.
To assess changes in the myocardium characteristic of coronary heart disease, an ECG test is performed with dosed physical activity (bicycle ergometer, treadmill). According to the doctor’s recommendations, tests are carried out with medications and hyperventilation.
Preparing to take a cardiogram
In order for the test to pass as quickly and efficiently as possible, the following tips may be useful:
- Tell your doctor about all the medications you are taking, as many of them may affect the test results.
- Instead, wear clothes that are easy to take off or unbutton at the chest.
- On the day before the test, no creams should be applied to the skin, as they affect electrical conductivity.
- Remove all jewelry from your neck and arms in advance.
- Ask your doctor any questions you have about this test, its risks, and its results.
No special preparation is needed to record an ECG. Immediately before the test, you should avoid physical activity and do not drink cold water.
Registration and interpretation of ECG
The doctor diagnoses organic and functional changes in the heart by looking at ECG data transferred to paper. The cardiologist analyzes the elements of the cardiogram: leads, waves, segments, intervals and their deviations from the norm.
The main indicator of the ECG is the heart rhythm. The heart rate of a healthy person is 60-80 beats per minute. Deviations from the norm to a lesser extent are diagnosed as bradycardia (this indicator also occurs in athletes); to a greater extent – tachycardia (occurs during physical activity, emotional experiences).
ECG is a universal test that helps diagnose diseases such as chronic heart failure, myocarditis, myocardiosclerosis, myocardial dystrophy, myocardial infarction, and the presence of post-infarction scars. It is worth highlighting the most common problem today - left ventricular hypertrophy; Using an ECG, the problem can be tracked and treatment can be started on time, whereas if not diagnosed on time, the disease often leads to the sudden death of the patient.
It is known that the fetal circulatory system has significant originality, characteristic of its intrauterine existence. This is due to the presence of placental and absence of pulmonary circulation, the anatomy of the heart and blood vessels of the fetus and the features of extracardiac regulation of the functioning of its cardiovascular system [1, 2]. The functioning of the fetal cardiovascular system depends on the demands placed on its body by changing conditions of the external and internal environment [1]. Therefore, we can assume that the fetal body’s responses to any extreme influences should be reflected in changes in its cardiac activity. This makes it possible to consider the indicators of fetal cardiac activity as an operational indicator of these reactions. One of the recently widespread pathological conditions leading to the above changes is the early development of fetal growth restriction syndrome [3]. This pathology is associated with disorders of vasculogenesis, leading to the development of endothelial dysfunction. Diagnosis of this condition is certainly difficult due to the small gestational age (20-30 weeks). There are different methods for assessing fetal cardiac performance. Auscultation, for example, allows one to assess cardiac performance, but does not provide the ability to record the obtained data, unlike biophysical methods for assessing the condition of the fetus, namely: ultrasound (US), electrocardiography (ECG) and cardiotocography (CTG). All of the listed methods for assessing the condition of the fetus make it possible to timely identify existing changes and determine the correct tactics for managing such patients, as well as choose the most suitable method and timing of delivery.
Auscultation.
One of the earliest and most widely used methods for assessing fetal cardiac activity was and continues to be the auscultation method, which allows one to obtain important information about the condition of the fetus, both qualitative and quantitative [4]. Using such a simple method, a large number of pathological conditions of the fetus can be recognized. Moreover, the main advantage of this method is the accessibility and simplicity of the study. However, it has been shown that the auscultation method, compared to technically more accurate methods, in most cases does not provide sufficient reliability and accuracy of data [4].
Ultrasound methods for assessing fetal cardiac activity.
Ultrasound methods for obtaining information about the cardiac activity of the fetus include ultrasound scanning methods that allow obtaining images of the fetus, its heart, as well as methods based on the Doppler effect [5, 6]. The latter make it possible to record the speed characteristics of the movements of the walls and valves of the fetal heart, as well as the heart rate (HR). The relatively large attenuation of ultrasound in tissues and the desire to obtain high resolution determined the choice of the frequency range of the equipment used to locate the fetal heart from 3 to 5 MHz. Ultrasound (US) scanning methods provide information about the geometry of the heart chambers and such indicators as end-systolic and end-diastolic volumes, amplitudes of ventricular contractions, and movements of heart valves.
Currently, ultrasound makes it possible to determine the degree of disturbances of the entire mother-placenta-fetus complex. There are several classifications, the use of which is widely used.
Based on fetometry data, the severity of fetal growth restriction can be determined. In grade I, the fetometry indicators differ from the normative ones and correspond to their indicators, which are typical for pregnancies that are 2 weeks shorter (34.2%), in grade II - shorter by 3-4 weeks (56.6%), and in grade III. - shorter period of more than 4 weeks (9.2%). The severity of intrauterine growth restriction correlates with the severity of placental insufficiency and adverse perinatal outcomes [3, 7–9].
In most cases of complicated pregnancy and extragenital diseases, the initial stage of development of the pathological process is disturbances of the uteroplacental blood flow with the gradual involvement of the fetal-placental blood circulation and the cardiovascular system of the fetus in the pathological process. The indicated sequence of pathogenetic links of hemodynamic disorders is presented in the one developed by A.N. Strizhakov et al. [10] classification of blood flow disorders in the mother-placenta-fetus system:
— IA degree — violation of uteroplacental blood flow with preserved fetal-placental blood flow;
— IB degree — violation of fetal-placental blood flow with preserved uteroplacental blood flow;
- II degree - simultaneous disturbance of uteroplacental and fetal placental blood flow, not reaching critical values (preservation of positively directed diastolic blood flow in the umbilical cord artery);
- III degree - critical disturbance of fetal-placental blood flow (absence or retrograde direction of end-diastolic blood flow) with preserved or impaired uteroplacental blood flow.
A decrease in blood flow velocity in the umbilical cord artery in diastole to zero values or the appearance of retrograde blood flow indicates a significant increase in vascular resistance in the placenta, which is usually combined with a critically high level of lactate accumulation, hypercapnia, hypoxemia and acidemia in the fetus [5, 11].
With fetoplacental insufficiency, disturbances in the intracardiac hemodynamics of the fetus occur, consisting in a change in the maximum speeds of blood flow through the valves in favor of the left parts of the heart, as well as in the presence of regurgitant flow through the tricuspid valve. In case of critical condition of the fetus, the following changes in fetal hemodynamics are detected:
- zero or negative blood flow in the umbilical cord artery;
- regurgitation through the tricuspid valve;
— absence of the diastolic component of blood flow in the fetal aorta;
- increase in the diastolic component of blood flow in the middle cerebral artery;
- disturbance of blood flow in the ductus venosus and the inferior vena cava, while the Doppler criterion for disturbance of blood flow in the ductus venosus is a decrease in blood flow velocity in the late diastole phase, down to zero or negative values.
When the fetus is critically ill, the pulsation index in the ductus venosus exceeds 0.7. Doppler criteria for blood flow disorders in the inferior vena cava are an increase in the rate of reverse blood flow of more than 29% and the appearance of zero or reverse blood flow between the systolic and early diastolic flows [12].
Cardiotocography.
No less widespread for assessing the rhythm of the fetal heart is fetal cardiotocography - registration of heart rate using ultrasound Doppler sensors with simultaneous recording of contractile activity of the uterus. Despite the relatively short history of the use of CTG in obstetric practice, a large amount of phenomenological material has already been accumulated, including qualitative and quantitative criteria for assessing cardiotocograms, an empirical connection between the type of recordings, their individual components and the intrauterine state of the fetus [2].
Currently, the assessment of fetal CTG is based not only on the heart rhythm parameters themselves for 25-30 minutes of recording, but also on the nature of changes in fetal heart rate in response to physiological stimuli. Such stimuli include sound stimuli, palpation of the fetal head, or the response of the fetal heartbeat to uterine contractions [13]. However, changes in fetal heart rate are most often assessed in response to one’s own physical activity [13]. This assessment is called a “non-stress test”. The stress test refers to the reaction of the fetal heartbeat to uterine contractions caused by intravenous administration of an oxytocin solution to the mother. A connection has been demonstrated between a successful birth outcome and the presence of a fetal heart rate response (in the form of increased rhythm and increased variability) to physical activity [14]. Along with motor activity, the presence of respiratory activity is also a reliable indicator of fetal well-being. Recent studies have shown that fetal respiratory movements are a necessary component of development and can also be considered as a sign of normal fetal development [15]. An ultrasound study of this phenomenon showed that for a normally developing human fetus, the frequency of respiratory movements (at gestational age of 39-40 weeks) is about 40 per minute, and the proportion of periods of respiratory activity from the total recording time (fetal respiratory index) can vary from 35 up to 65% [5]. Moreover, it was shown that during the development of the initial stage of fetal hypoxia, respiratory activity disappeared first, while motor activity could not change or even increase [5]. However, the presence of respiratory activity can only be detected by ultrasound. Knowing that in adults and children there is a connection between respiratory movements, the activity of the respiratory center and changes in heart rhythm (respiratory cardioarrhythmia), one can imagine that such a connection theoretically exists in the human fetus. However, until now no convincing evidence of the existence of such a connection and its quantitative characteristics have been obtained.
For an objective quantitative assessment of the occurrence of fetal hypoxic conditions during a CTG study, various scoring scales are proposed, focused on the use of cardiac monitoring [2]. One of the most popular is the Fisher scale. With this method of assessing the condition of the fetus, each of the CTG indicators (basal rhythm, the presence of accelerations or decelerations) is assigned a score from 0 to 2 points (depending on compliance with their standard value). The total score can be a quantitative indicator of the condition of the fetus. In 1977, Oxford University professors G. Dawes and C. Redman developed certain parameters for automatic analysis of a cardiotocogram [21]. The convenience of this analysis system lies in minimizing the observation time - 10 minutes. During this time, the following parameters are assessed: 1) STV (short term variability) with a duration of 3 ms or more; 2) absence of signs of sinusoidal rhythm; 3) at least one episode of high variability; 4) absence of significant and prolonged decelerations; 5) the presence of accelerations and/or fetal movements; 6) absence of incorrect position of the basal line; 7) normal basal heart rate. These criteria were developed for a specific CTG monitoring device (Oxford Sonicaid). The monitor monitors fetal heart rate and uterine activity using an external uterine contraction sensor using 1-2 (depending on the number of fetuses) ultrasonic sensors. The sensitivity of these sensors to register the fetal heartbeat begins approximately at 24 weeks, and the accuracy of the analysis of the Dawes/Redman criteria begins at 32 weeks of gestation, which, of course, complicates the analysis of CTG monitoring at earlier times. In this regard, such an analysis method cannot always be used. Firstly, CTG analysis cannot give an absolute guarantee of the safe condition of the fetus in the short term. In addition, this study is inconvenient for the patient due to her forced position and limited movement, and therefore the duration of the recording depends on the patient’s condition. In addition to all of the above, records made before 32 weeks are assessed worse according to the Dawes/Redman criteria, which makes it very difficult to manage these patients.
Fetal electrocardiography.
A more informative alternative to cardiotocographic research is an electrocardiographic study.
The first non-invasive recording of a fetal electrocardiogram (ECG) was carried out by the German obstetrician-gynecologist M. Cremer in 1906 using a string galvanometer, invented by W. Einthoven 3 years earlier [cit. according to 18]. He placed one of the electrodes on the anterior abdominal wall of the pregnant woman above the fundus of the uterus, and the second electrode was applied transvaginally to the cervix. However, high-quality recordings allowing analysis of the fetal QRS complex could not be obtained without appropriate amplification until the 50s of the last century. Then, fairly successful results of recording the ECG of a human fetus through the anterior abdominal wall of the mother were demonstrated [18].
The ECG of the fetus, like the ECG of an adult, consists of the atrial and ventricular complexes, which are associated with the progress of the spread of electrical excitation through the myocardium of the atria (P wave) and ventricles (QRS complex). With the simplest abdominal lead of the fetal ECG through the anterior abdominal wall of the mother, the electrocardiosignal is most often represented only by the ventricular complex.
The electrocardiographic signal of the fetus is fundamentally different from the phonocardiographic (recording of vibrations and sound signals emitted during the activity of the heart and blood vessels) and ultrasonic Doppler signal [1, 3]. The ECG signal is based on the processes of excitation propagation throughout the myocardium. The nature of phonocardiographic and ultrasonic Doppler signals is phenomena associated with cardiac contractions. Thus, the ECG signal, in fact, is the primary controlling influence in relation to the signals caused by the mechanical manifestations of cardiac activity. This served as the basis for the development of such combined methods for studying fetal cardiac activity as phase analysis (synchronous recording of ECG and fetal PCG) [16] and registration of electromechanical intervals (simultaneous recording of ECG and ultrasound Doppler signals of the fetal heart) [1, 17]. These methods made it possible to determine such intervals of the cardiac cycle as the presystolic period (the time between the Q wave on the ECG and the moment of opening of the aortic valve), the time of ejection of blood from the left ventricle (the period between the opening and closing of the aortic valve) [12]. The relationship between these intervals and heart rate, fetal age, contractile state of the myocardium and other indicators has been shown [12]. For example, the presystolic period and ejection time turned out to be very sensitive to changes in diastolic pressure in the aorta, which makes it possible to quite clearly diagnose pathologies such as compression of the fetal umbilical cord and impaired fetoplacental circulation. Thus, data on the fetal heart rate obtained from its ECG mainly reflect the function of the control part of the fetal cardiac regulation circuit, and the parameters of PCG and ultrasound Doppler signals mainly depend on the functioning of the executive part of this circuit.
The benefits of objective methods for studying cardiac activity are most effectively realized with long-term monitoring of the fetus [2, 18].
Summarizing the opinion of most researchers, it can be argued that the study of fetal heart rate records contributes to the early detection of its hypoxic conditions [2, 19, 20].
The main locations for installing electrodes are given in the works of various researchers [14, 15, 25]. It is believed that for reliable identification of fetal electrocardiographic signals, one should strive to ensure that the electrodes are strictly located over the areas of the fetal head and buttocks.
Along with obvious advantages (direct recording of the electrical activity of the fetal heart), the ECG method has several disadvantages. Firstly, in the interval from the 28th to the 33rd week of pregnancy, registration of the fetal ECG signal is complicated by the insulating effect of the fetal cheese-like lubricant, which has low conductivity for electric current [18, 22]. The second point is the mother’s own electrical activity of the heart. Maternal ECG signals are superimposed on fetal signals, which significantly complicates automatic processing of fetal ECG [6, 18, 22, 23]. Thus, recording a fetal ECG is a rather complex operation that requires special methods for isolating the electrocardiographic signal [13, 14, 17, 20, 22, 24]. However, the ECG method also has one undeniable advantage - it allows you to accurately determine the moment of the onset of the fetal QRS complex, and therefore obtain significantly more accurate (compared to other registration methods) information about the duration of the fetal cardiac cycle.
To register the fetal ECG, special equipment and measures are used to neutralize additional noise and stray electrical potentials.
The currently existing apparatus for electrocardiographic examination of the fetus passively records electrical impulses coming from the fetus and, accordingly, it is possible to obtain the result of a reliable recording in earlier stages of pregnancy. The device is also able to respond to the contractile activity of the uterus, to the movements and movements of the mother, and therefore allows you to assess the condition of the fetus and mother fully, in a single complex. The device assesses the heartbeat of the fetus, mother, contractile activity of the uterus, motor activity of the mother (stirring and movement), and therefore gives a more complete picture of the condition of the mother and fetus together. The advantage of such a device is also the ability to record an ECG of the fetus from 20 weeks of gestation. This system is capable of recording for 24 hours or more, regardless of the mother's position. Electrodes are installed on the patient’s abdomen, which receive signals and translate them into a CTG monitoring recording, which allows for daily monitoring and control of the condition of the suffering fetus [12, 22]. An additional advantage of such a system is that it passively records electrical signals, and no ultrasonic effect on the fetus, unlike other systems, occurs.
Thus, ECG examination of the fetus has an advantage over other methods of assessing the condition of the fetus due to the accurate objective assessment of indicators of its condition over a long period of time in the absence of external influence on the fetus. This system can be used in the earliest stages of gestation (20 weeks) for the purpose of timely detection of pathological changes in the condition of the fetus. The use of Doppler ultrasound in combination with a fetal ECG provides a more complete picture of changes in cardiac activity and the condition of the fetus.
The authors declare no conflict of interest.
*e-mail; ORCID: https://orcid.org/0000-0002-7224-3453
ECG during pregnancy
During pregnancy, a woman's heart is subject to increased stress, because... The volume of circulating blood increases and the concentration and composition of hormones changes. An ECG test is performed for every pregnant woman upon registration. When developing a labor management plan (at a later date), a repeat study is carried out. These measures help to identify disturbances in the functioning of the heart muscle and prevent the development of complications. If any changes are detected on the ECG, the woman is referred for consultation and, possibly, treatment to a cardiologist.
The absolute safety and simplicity of the study serves as a recommendation for its use in pregnant women and children of any age.
Pregnancy management after IVF in the 1st trimester
The pregnancy management program after IVF in the 1st trimester may differ slightly from the usual one. Firstly, the woman continues to be observed at the IVF center by a fertility specialist until 6-7 weeks, when the doctor can record the heartbeat of the embryo. Only after this can the expectant mother contact an obstetrician-gynecologist. At the first stage, the doctor decides on the advisability of maintenance hormonal therapy
, prescribed earlier at the IVF center. Whenever possible, we try to either reduce or eliminate additional hormonal therapy.
Thus, monitoring of pregnancy after IVF begins at an earlier stage, and the program can be adjusted depending on the characteristics of the individual case: is it a singleton or multiple pregnancy, what problems should be taken into account, etc.
Where to do an ECG of the heart
In the problem of competently taking and interpreting an ECG, the main role is played by the choice of a specialist and a clinic. This measurement is quite common - the device is available in all free public clinics, but there are many arguments in favor of private ones.
Reasons to have an electrocardiogram done at the Medicenter:
No queues . By making an appointment at a time convenient for you, you will quickly receive results and a professional transcript and go about your business.
Professional doctors. Medicenter employs highly qualified cardiologists with extensive experience. They have knowledge and specificity in taking cardiograms in children and adults.
Possibility to conduct research at home. Not many medical centers offer such services to patients. This offer is especially relevant for elderly patients and children.
The latest equipment. To take an ECG, the Medicenter uses a 3-channel ECG machine “Cardiomax” (Japan), which has the full range of capabilities of modern cardiac equipment.
Low price.
When is a Holter ECG needed for a pregnant woman?
Some women need a pregnancy recorder for diagnosis or heart rate monitoring, set to 24-hour recording. In this way, the possible causes of the symptoms that a pregnant woman is struggling with can be assessed. Indications for such a procedure are:
- symptom check
- assessment of the risk of symptoms and their impact on the life of the expectant mother and unborn child
- assessment of the effectiveness of treatment
- assessment of the heart stimulating system
- determining changes in rest and exercise parameters and comparing them
One thing is for sure, a cardiac ECG during pregnancy is one of the most frequently chosen methods for monitoring the functioning of the heart and cardiovascular system. And although other additional tests can also play an extremely important role, it is the ECG during pregnancy that is of paramount importance. Using ECG machines, the entire heart function can be imaged, identifying normal or abnormal ECG results.
Indications for ECG
Everyone needs to check their heart function from time to time. Data on the condition of the heart muscle is necessary in the following cases:
- arterial hypertension;
- age over 40 years;
- smoking;
- increased cholesterol levels in the blood;
- pregnancy;
- past infections;
- upcoming surgery;
- other diseases with suspected involvement of the heart in the pathology;
- deterioration of the condition of patients with “heart disease” (pain, arrhythmia, shortness of breath);
- occupational risk factors (shift work at different times of the day, nervous overstrain, occupational hazards);
- expert assessment of the working capacity of drivers, sailors, pilots.
Make an appointment for an ECG or consultation with a cardiologist.
Documentation
At 28–30 weeks, the doctor gives the woman a so-called exchange card, where all the data regarding the course of pregnancy, test results and opinions of medical specialists are entered.
The exchange card contains:
- past illnesses
- Features of the course of previous pregnancies, childbirth, and the postpartum period
- abortions
- premature birth
- last normal menstruation
- gestational age at the first consultation visit number of consultation visits
- first fetal movement
- pelvic dimensions, height, weight
- fetal position, presenting part, heartbeat
- laboratory tests: RW (Wassermann reaction - blood tests for syphilis), Rh factor and blood group - Rh affiliation of the husband’s blood
- general blood test, general urinalysis, vaginal smear
- weight gain during pregnancy
- blood pressure, etc.
The exchange card must always be with you. Be sure to take it with you when leaving home. And if for some reason you suddenly have to end up in the maternity hospital earlier than expected, the exchange card will help doctors act correctly, taking into account the characteristics of your body.
The second part of the exchange card is filled out in the maternity hospital and contains information about the course of labor and the postpartum period, as well as data about the newborn:
- gender, height, weight (at birth and at discharge)
- assessment of the child's condition
- the day of the first breastfeeding and the day the umbilical cord falls off
- carrying out anti-tuberculosis vaccination and vaccination against hepatitis B.