A coagulogram is a graphical expression of the results of a study of the hemostatic system. It is otherwise called a hemastosiogram. This is a fairly complex blood test that allows you to evaluate the functioning of the blood coagulation and anticoagulation systems and identify possible disorders. A coagulogram during pregnancy is a mandatory examination. Any deviations in the hemostatic system can cause miscarriage or premature birth.
For the health of the woman and the unborn child, it is important that the coagulation and anti-coagulation systems work in a balanced manner. If this balance is disturbed, any of the systems is more active, and various pathologies can develop in the woman and fetus. If the anticoagulant factor is more active, a woman may experience spontaneous bleeding, placental abruption is possible, and there is a danger of large blood loss during childbirth and after its completion.
If the activity of the coagulation component of hemostasis predominates, the blood becomes thick and there is a risk of developing blood clots, which can cause fetal hypoxia. The woman herself may develop blood clots, deep vein thrombosis of the lower extremities and pelvis, as well as pulmonary embolism.
Coagulogram parameters
During the analysis, the following parameters are examined:
- Fibrinogen. This special protein is synthesized in the liver and takes part in blood clot formation. Fibrinogen is considered one of the main components of a blood clot. When a vessel is damaged, it turns into insoluble fibrin strands, which ultimately form a blood clot. It closes the vessel defect, thereby preventing blood loss. The fibrin clot remains at the site of injury until complete healing only if the components of the clot are present in sufficient quantities. A deficiency of prothrombin and fibrinogen leads to bleeding; an excess amount of these factors can result in the formation of blood clots without damaging the vessel walls.
- Prothrombin. Production occurs in the liver with the participation of vitamin K. One of the main blood clotting factors. This indicator makes it possible to prevent placental abruption, bleeding during childbirth, and the development of thrombosis. It allows you to identify pathologies of the liver and digestive system.
- APTT. This is the time during which the formation of a blood clot occurs. With its help, the functioning of the coagulation system is assessed according to the internal mechanism and it is determined whether there is a lack of plasma blood factors.
- Thrombin time. During this time, a blood clot forms after the blood plasma mixes with thrombin.
- Prothrombin time. During this time, a thrombin clot is formed when thromboplastin and calcium are added to the plasma.
- RFMK. These are intermediate products of fibrin thrombus breakdown as a result of fibrinolysis (soluble fibrin-monomer complexes). They are difficult to detect because they are removed from the plasma very quickly.
- Antithrombin III. This complex protein is produced by liver and vascular cells. It prevents blood clotting and the formation of clots.
- Lupus anticoagulant. These are immunoglobulins M and G, which in case of autoimmune lesions of platelets (thyroiditis, rheumatoid arthritis, lupus erythematosus) are produced against their membranes. Normally, it is not present in the blood of a pregnant woman. Determined in the presence of autoimmune diseases or gestosis. Lupus anticoagulant complicates pregnancy and can lead to miscarriage.
- D-dimer. This is an indicator of the process of clot formation and fibrin dissolution.
A coagulogram is a comprehensive study of hemostasis that allows you to assess the state of different parts of the coagulation, anticoagulation and fibrinolytic blood systems and identify the risk of hypercoagulation (excessive coagulation) or hypocoagulation (bleeding).
Synonyms Russian
Hemostasiogram: prothrombin index (PTI), prothrombin time (PT), international normalized ratio, factor I (first) of the plasma coagulation system, antithrombin III (AT3), activated partial thromboplastin time, fibrin degradation product.
English synonyms
Coagulation studies (coagulation profile, coag panel, coagulogram): Prothrombin time (Pro Time, PT, Prothrombin time ratio, P/C ratio); International Normalized Ratio (INR); Fibrinogen (FG, Factor I); Antithrombin III (ATIII Activity, Heparin Cofactor Activity, Serine Protease Inhibitor); Activated Partial thromboplastin time (aPTT, PTT); D-Dimer (Fibrin degradation fragment).
Research method
Coagulometry.
Units
% (percentage), g/l (grams per liter), sec. (second), μg FEO/ml (microgram fibrinogen-equivalent units per milliliter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 12 hours before the test.
- Avoid physical and emotional stress 30 minutes before the test.
- Do not smoke for 30 minutes before the test.
General information about the study
The hemostasis system consists of many biological substances and biochemical mechanisms that ensure the preservation of the liquid state of the blood and prevent and stop bleeding. It maintains a balance between clotting and anticoagulant factors. Significant disturbances in the compensatory mechanisms of hemostasis are manifested by processes of hypercoagulation (excessive thrombus formation) or hypocoagulation (bleeding), which can threaten the patient’s life.
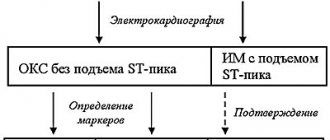
When tissues and blood vessels are damaged, plasma components (clotting factors) participate in a cascade of biochemical reactions, which results in the formation of a fibrin clot. There are internal and external pathways of blood coagulation, which differ in the mechanisms for triggering the coagulation process. The internal pathway is realized when blood components come into contact with the collagen of the subendothelium of the vessel wall. This process requires coagulation factors XII, XI, IX and VII. The extrinsic pathway is triggered by tissue thromboplastin (factor III) released from damaged tissue and the vascular wall. Both mechanisms are closely interrelated and from the moment of formation of active factor X they have common paths of implementation.
The coagulogram determines several important indicators of the hemostatic system. Determination of PTI (prothrombin index) and INR (international normalized ratio) allows you to assess the state of the external blood coagulation pathway. PTI is calculated as the ratio of the standard prothrombin time (the clotting time of control plasma after the addition of tissue thromboplastin) to the clotting time of the patient's plasma and is expressed as a percentage. INR is a prothrombin test standardized in accordance with international recommendations. It is calculated by the formula: INR = (patient prothrombin time / control prothrombin time) x MICH, where MICH (international sensitivity index) is the sensitivity coefficient of thromboplastin relative to the international standard. INR and PTI are inversely proportional indicators, that is, an increase in INR corresponds to a decrease in the patient’s PTI, and vice versa.
Studies of PTI (or a similar indicator - prothrombin according to Quick) and INR as part of a coagulogram help to identify disorders in the external and general blood coagulation pathways associated with a deficiency or defect of fibrinogen (factor I), prothrombin (factor II), factors V (proaccelerin) , VII (proconvertin), X (Stewart-Prower factor). With a decrease in their concentration in the blood, the prothrombin time increases in relation to control laboratory parameters.
Plasma factors of the extrinsic coagulation pathway are synthesized in the liver. For the formation of prothrombin and some other coagulation factors, vitamin K is required, the deficiency of which leads to disturbances in the cascade of reactions and prevents the formation of a blood clot. This fact is used in the treatment of patients with an increased risk of thromboembolism and cardiovascular complications. Thanks to the prescription of the indirect anticoagulant warfarin, vitamin K-dependent protein synthesis is suppressed. PTI (or Quick prothrombin) and INR coagulation are used to monitor warfarin therapy in patients with factors that promote thrombosis (for example, deep vein thrombosis, the presence of prosthetic valves, antiphospholipid syndrome).
In addition to prothrombin time and related indicators (INR, PTI, prothrombin according to Quick), other indicators of the hemostatic system can be determined in the coagulogram.
Activated partial thromboplastin time (aPTT) characterizes the intrinsic pathway of blood coagulation. The duration of APTT depends on the level of high molecular weight kininogen, prekallikrein and coagulation factors XII, XI, VIII and is less sensitive to changes in the levels of factors X, V, prothrombin and fibrinogen. APTT is determined by the duration of blood clot formation after calcium and partial thromboplastin are added to the blood sample. An increase in aPTT is associated with an increased risk of bleeding, a decrease is associated with thrombosis. This indicator is used separately to monitor therapy with direct anticoagulants (heparin).
Fibrinogen is a blood clotting factor I produced in the liver. Thanks to the action of the coagulation cascade and active plasma enzymes, it is converted into fibrin, which is involved in the formation of a blood clot and thrombus. Fibrinogen deficiency can be primary (due to genetic disorders) or secondary (due to excessive consumption in biochemical reactions), which is manifested by impaired formation of a stable blood clot and increased bleeding.
Fibrinogen is also an acute-phase protein; its concentration in the blood increases in diseases accompanied by tissue damage and inflammation. Determining the level of fibrinogen as part of a coagulogram is important in the diagnosis of diseases with increased bleeding or thrombus formation, as well as for assessing the synthetic function of the liver and the risk of cardiovascular diseases with complications.
The blood anticoagulation system prevents the formation of excess amounts of active clotting factors in the blood. Antithrombin III is the main natural inhibitor of blood clotting, which is synthesized in the liver. It inhibits thrombin, activated factors IXa, Xa and XIIa. Heparin enhances the activity of antithrombin 1000 times, being its cofactor. The proportional ratio of thrombin and antithrombin ensures the stability of the hemostatic system. With primary (congenital) or secondary (acquired) AT III deficiency, the blood coagulation process will not be stopped in a timely manner, which will lead to increased blood clotting and a high risk of thrombosis.
The formed thrombus undergoes fibrinolysis over time. D-dimer is a fibrin degradation product that allows the fibrinolytic activity of plasma to be assessed. This indicator increases significantly in conditions accompanied by intravascular thrombosis. It is also used in dynamic monitoring of the effectiveness of anticoagulant therapy.
What is the research used for?
- For a general assessment of the blood coagulation system.
- For the diagnosis of disorders of the internal, external and general pathways of blood coagulation, as well as the activity of the anticoagulant and fibrinolytic systems.
- To examine the patient before surgery.
- To diagnose the causes of miscarriage.
- For diagnosing DIC syndrome, venous thrombosis, antiphospholipid syndrome, hemophilia and assessing the effectiveness of their treatment.
- To monitor anticoagulant therapy.
When is the study scheduled?
- If DIC syndrome or pulmonary embolism is suspected.
- When planning invasive procedures (surgical interventions).
- When examining patients with nosebleeds, bleeding gums, blood in the stool or urine, hemorrhages under the skin and in large joints, chronic anemia, heavy menstrual flow, sudden loss of vision.
- When examining a patient with thrombosis, thromboembolism.
- When lupus antibodies and antibodies to cardiolipin are detected.
- With a hereditary predisposition to disorders of the hemostatic system.
- With a high risk of cardiovascular complications and thromboembolism.
- For severe liver diseases.
- With repeated miscarriages.
- When monitoring the hemostatic system against the background of long-term use of anticoagulants.
- Prothrombin according to Quick: 70 - 120%.
- INR
What do the results mean?
Reference values (table of normal coagulogram indicators)
| Age | Reference values |
| Less than 3 days | 1,15 — 1,35 |
| 3 days – 1 month | 1,05 — 1,35 |
| 1 month – 1 year | 0,86 — 1,22 |
| 16 years | 0,92 — 1,14 |
| 6 – 11 years | 0,87 — 1,20 |
| 11 – 16 years | 0,97 — 1,30 |
| More than 16 years | 0,8 — 1,2 |
| Week of pregnancy | Reference values |
| 13-21st | 0,56 — 1,1 |
| 21st-29th | 0,5 — 1,13 |
| 29-35th | 0,58 — 1,17 |
| 35-42nd | 0,15 — 1,14 |
- Fibrinogen: 1.8 - 3.5 g/l.
| Week of pregnancy | Reference values |
| 1-13th | 2.12 - 4.33 g/l |
| 13-21st | 2.9 - 5.3 g/l |
| 21st-29th | 3 - 5.7 g/l |
| 29-35th | 3.2 - 5.7 g/l |
| 35-42nd | 3.5 - 6.5 g/l |
- Antithrombin
| Age | Reference values |
| Less than 3 days | 58 — 90 % |
| 3 days – 1 month | 60 — 89 % |
| 1 month – year | 72 — 134 % |
| 1-6 years | 101 — 131 % |
| 6-11 years | 95 — 134 % |
| 11-16 years old | 96 — 126 % |
| More than 16 years | 66 — 124 % |
| Week of pregnancy | Reference values |
| 13-21st | 74 — 115 % |
| 21st-29th | 73 — 114 % |
| 29-35th | 76 — 112 % |
| 35-42nd | 70 — 116 % |
- Activated partial thromboplastin time (aPTT): 21.1 - 36.5 seconds.
- D-dimer
a) For men and non-pregnant women: 0 - 0.55 mcg FEU / ml.
b) For pregnant women:
| Week of pregnancy | Reference values |
| Until 13th | 0 - 0.55 µg FEO/ml |
| 13-21st | 0.2 - 1.4 µg FEO/ml |
| 21st-29th | 0.3 - 1.7 µg FEO/ml |
| 29-35th | 0.3 - 3 µg FEO/ml |
| 35-42nd | 0.4 - 3.1 µg FEO/ml |
INR and PTI
Reasons for increased INR and decreased PTI (or prothrombin according to Quick) in the coagulogram
(Indicate a possible deficiency of factors in the external pathway of hemostasis and a tendency to increased bleeding).
- DIC syndrome (disseminated intravascular coagulation) during the period of hypocoagulation.
- Hypofibrinogenemia (factor I deficiency).
- Dysfibrinogenemia (synthesis of a defective protein that is not able to participate in the cascade of biochemical reactions).
- Hereditary or acquired deficiency of factors II, V, VII.
- Factor X deficiency (eg, purpura in amyloidosis).
- Vitamin K deficiency.
- Hemorrhagic disease of newborns.
- Malabsorption with impaired fat absorption (due to celiac disease, chronic diarrhea).
- Acute leukemia.
- Antiphospholipid syndrome.
- Congestive heart failure.
- Liver pathology (hepatitis, cirrhosis, alcoholic liver disease).
- Obstruction of the biliary tract, obstructive jaundice.
- Pancreas cancer.
- Zollinger-Ellison syndrome (pancreatic adenoma).
- Toxic shock syndrome.
- Nephrotic syndrome (excessive urinary excretion of factors V and VII).
- Oral anticoagulants (warfarin).
Reasons for a decrease in INR and an increase in PTI (or prothrombin according to Quick) in a coagulogram
(Indicate a tendency to form blood clots).
- DIC syndrome (period of hypercoagulation).
- Deep vein thrombosis (initial stages).
- Polycythemia.
- Pregnancy (last months).
- Increased activity of factor VII.
APTT
Reasons for increased aPTT in the coagulogram
(Indicate the predominance of hypocoagulation).
- Deficiency of factors VIII (hemophilia A), IX (hemophilia B), XI, XII, X, V, II.
- Von Willebrand factor deficiency.
- Prekallikrein deficiency.
- Hypo- or afibrinogenemia.
- Vitamin K deficiency.
- DIC syndrome (chronic or acute during hypocoagulation).
- Liver cirrhosis, liver failure.
- Malabsorption.
- Leukemia.
- The use of direct and indirect anticoagulants and fibrinolytics.
Reasons for decreased aPTT in the coagulogram
(Indicate the predominance of thrombus formation).
- DIC syndrome (hypercoagulation phase).
- Malignant neoplasms.
- Acute blood loss (immediately before taking the test).
Fibrinogen
Reasons for increased fibrinogen levels in the coagulogram
(Indicates an increased risk of blood clots and cardiovascular complications).
- Acute infection (eg, pneumonia, tuberculosis).
- Autoimmune diseases (rheumatoid arthritis, reactive arthritis).
- Acute coronary syndrome, myocardial infarction.
- Burns.
- Cancer (breast, kidney, stomach).
- Multiple myeloma.
- Hodgkin's disease (lymphogranulomatosis).
- Glomerulonephritis, nephrotic syndrome, nephrosis.
- Pregnancy.
- Eclampsia.
- Cerebrovascular disease, stroke.
- Hepatitis.
- Postoperative period.
- Rheumatic fever.
- Tissue damage.
Reasons for decreased fibrinogen levels in the coagulogram
(May indicate an increased risk of bleeding).
- Dysfibrinogenemia.
- Hereditary afibrinogenemia.
- DIC syndrome.
- Fibrinolysis.
- Hemophilia A and B.
- Liver pathology (hepatitis, cirrhosis).
- Abortion.
- Premature placental abruption.
- Late stage of cancer.
- Embolism (amniotic fluid, meconium, fat, tissue).
- Anemia.
- Eclampsia.
- Leukemia.
- Malabsorption.
- Shock.
- Sepsis.
- Post-transfusion reactions.
Antithrombin III
Reasons for increasing the level of antithrombin III in the coagulogram
(Increased risk of bleeding).
- Conditions accompanied by cholestasis (viral hepatitis, pancreatitis, pancreatic cancer).
- Kidney transplantation.
- Vitamin K deficiency.
- Therapy with indirect anticoagulants (warfarin).
- Menstruation.
- Hyperglobulinemia.
Reasons for the decrease in the level of antithrombin III in the coagulogram
(The risk of blood clots increases; the likelihood of recurrent miscarriages in pregnant women increases).
- Congenital deficiency of AT III.
- DIC syndrome.
- Deep vein thrombosis.
- Liver pathology (cirrhosis, liver failure).
- Nephrotic syndrome.
- Conditions accompanied by protein loss.
- Thromboembolism of the pulmonary arteries.
- Myocardial infarction.
- Inflammatory bowel diseases.
- Cancer diseases.
- The period of pregnancy (late stages) or newborn (first days).
- Liver transplantation.
- Malabsorption.
- Postoperative period.
- Sepsis.
D -dimer
Reasons for increased D-dimer levels in the coagulogram
(Indicates excessive thrombus formation and fibrinolysis).
- Arterial and venous thrombosis.
- Pulmonary embolism.
- DIC syndrome.
- Eclampsia.
- Fibrinolysis.
- Myocardial infarction.
- Acute infection, active inflammatory process.
- Pregnancy (last months).
- Liver diseases.
- Malignant neoplasms.
- Postoperative period.
- Injury.
What can influence the result?
Factors distorting the result of the analysis:
- the presence of a lupus anticoagulant in the patient’s blood (directly inhibits coagulation factors);
- sharply increased or decreased hematocrit;
- transfusion of donor blood components in the last month (distorts the fibrinogen indicator, APTT).
Factors that increase INR and PT and decrease PTI (or prothrombin according to Quick):
- drinking alcohol, fatty foods;
- medications: antibiotics, anabolic steroids, aspirin (in large doses), acetaminophen, allopurinol, warfarin, vitamin A, heparin, glucagon, diuretics, MAO inhibitors, indomethacin, kanamycin, clofibrate, corticotropin, levothyroxine, mercaptopurine, methyldopa, mefenamic acid, mithramycin, nalidixic acid, neomycin, nortriptyline, propylthiouracil, reserpine, streptomycin, sulfonamides, tamoxifen, tetracyclines, tolbutamide, phenylbutazone, phenytoin, quinidine, quinine, chloral hydrate, chloramphenicol, cholestyramine, cimetidine, ethanol.
Factors that reduce INR and PT and increase PTI (or prothrombin according to Quick):
- excess intake of vitamin K from food (found in beef or pork liver, green tea, broccoli, chickpeas, cabbage, turnips, soy, green leafy vegetables);
- diarrhea and vomiting (due to dehydration and increased blood viscosity);
- medications: vikasol (vitamin K analogue), antacids, antihistamines, ascorbic acid, barbiturates, griseofulvin, digitalis, diuretics, colchicine, corticosteroids, caffeine, xanthines, meprobamate, oral contraceptives, rifampicin, theophylline, phenobarbital, chloral hydrate.
Factors that increase APTT: antibiotics, asparaginase, aspirin, warfarin, heparin, thrombolytic drugs (streptokinase, urokinase), quinine, cholestyramine, cyclophosphamide, enoxaparin.
Factors that increase fibrinogen content: estrogens, oral contraceptives.
Drugs that reduce fibrinogen levels: atenolol, valproic acid, lipid-lowering drugs, corticosteroids, progesterone, thrombolytic drugs (streptokinase, urokinase), fluorouracil, estrogens, fibrin degradation products, nicotine.
Drugs that increase the content of AT III: anabolic steroids, androgens, progesterone-containing oral contraceptives, warfarin.
Drugs that reduce AT III levels: heparin, estrogen-containing oral contraceptives, fibrinolytics, L-asparaginase, fluorouracil. Surgery, prolonged bed rest.
Factors that increase the content of D-dimer: thrombolytic drugs (streptokinase, alteplase, urokinase), estrogen-containing drugs, high levels of rheumatoid factor or tumor marker CA 125 in the blood.
How is the test done?
No special preparation is required. Like any blood test, it is taken in the morning on an empty stomach. Blood is taken from a vein in the bend of the elbow. Pregnant women get tested at the antenatal clinic. Decoding is the responsibility of the gynecologist with whom the expectant mother is registered. If all blood parameters are normal, this test is taken every trimester, that is, only three times:
- at the first visit to the gynecologist about pregnancy;
- around the 23rd week;
- shortly before birth - at the 34th - 36th week (this is especially important for those who are indicated for a cesarean section).
During pregnancy, blood is donated for a coagulogram every trimester.
If there are deviations from the norm, coagulation testing will have to be performed more often.
The need and frequency of testing for coagulation during pregnancy
For pregnant women, a coagulogram is an extremely important analysis. With its help, the balance of the coagulation and anticoagulation systems is monitored.
- The absence of such a balance carries, as mentioned above, consequences that threaten the health of the expectant mother and fetus.
- An imbalance towards the anticoagulation system can cause metrorrhagia, placental abruption, blood loss during and after childbirth in a woman in labor, and towards the coagulation system it thickens the blood, forming blood clots. In this case, a child who receives oxygen exclusively from the placenta experiences oxygen starvation, hypoxia develops, brain pathologies may develop, the woman suffers from leg pain and the development of blood clots, and this can also cause a heart attack, stroke or miscarriage.
The test procedure is as follows: before taking blood, it is better to fast, that is, take the test on an empty stomach. Blood is taken from a vein on the bend of the elbow, and the result of the hemostasiogram is deciphered by your attending physician.
If the indicators are normal, the diagnosis is carried out three times as planned:
- During the registration of a pregnant woman (usually the 1st trimester),
- In the second trimester,
- A week or two before giving birth, which is especially important for women who are preparing to give birth by cesarean section.
In case of complications or abnormal pregnancy, homeostasis is checked much more often in order to respond adequately and prescribe effective treatment.
The normal indicators for a woman during this period, due to changes in physiology, are somewhat different from the indicators before conception, since the female body sets up another blood circulation through the utero-placental-fetal blood flow (insuring itself from significant blood loss). Therefore, only your registered doctor can diagnose the coagulogram results.
Indications for additional testing
Sometimes a pregnant woman has to take a coagulogram test more often than once per trimester. This happens in cases where a woman has the following pathologies:
- Autoimmune diseases.
- Liver diseases.
- Phlebeurysm.
- Disturbances in the functioning of the urinary, endocrine and hematopoietic systems.
- Vascular pathologies.
- Condition after surgery.
- Multiple pregnancy.
- Predisposition to increased blood clotting.
- Tendency to bleed.
- Deviations from the norm discovered during the first study.
- Having bad habits.
- Miscarriage.
- Fetoplacental insufficiency, gestosis.
Deciphering violations in the results and their causes
Below is a table of deviations from the norm in the coagulogram, which are dangerous during pregnancy and their possible causes.
| Index | Numerical value within normal limits | Possible deviation | Causes |
| APTT | 15-20 seconds | increase to 25-39 sec. reduction to 10-12 sec. | vitamin K deficiency, von Willebrand disease, liver disease. DIC syndrome, inflammatory processes. |
| Fibrinogen | 6 g/l | Increase over 6 g/l | Infectious diseases, necrotic processes, burns and injuries, lupus, heart attack, tumor |
| D-dimer | 250 ng/ml | Increase more than 4.5 times | Preeclampsia, kidney disease, internal hematomas and hemorrhages |
| Platelet level | 150-350 * 1099 per 1 l. blood | increase; decrease. | diarrhea, toxicosis, frequent vomiting, thromboembolism, dehydration, chronic bleeding, poor nutrition, disorders of the immune system. |
Coagulogram norms and interpretation
The test results are interpreted by a gynecologist. Coagulogram indicators should have the following values during pregnancy:
- Fibrinogen. During pregnancy, the level of this protein should be normal in the first trimester. In the second trimester it rises to 4–5 g/l. Closer to childbirth, the normal level is 6 grams/liter.
- Thrombin time. This indicator during pregnancy is slightly higher than normal. Its value should be between 11 and 18 seconds. If it is higher than normal, there may be liver pathologies.
- APTT. As for the activated partial thromboplastin time, in expectant mothers it is slightly reduced, which is the norm during this period. Its value is from 17 to 20 seconds.
- Prothrombin. This is one of the most important hemostasiogram indicators for a pregnant woman, since exceeding the norm can lead to placental abruption. This figure should be between 78 and 142%.
- Prothrombin time. This important indicator is normally no more than 18 seconds and should not change during pregnancy. Otherwise, you should definitely consult a doctor to find out the cause and take action.
- Lupus anticoagulant. This is an indicator of the presence of antibodies that contribute to an increase in aPTT. There should be no antibodies during pregnancy. If they are detected, then this is a sign of gestosis or an autoimmune disease.
- RFMK. The norm in the first trimester is 78-130 units, in the second - 85-135, in the third - 90-140.
- Antithrombin III. This is an anticoagulant component of hemostasis, which is considered one of the main parameters of the analysis. Normally it should be 75-125%. If it is below 75%, then there is a tendency to form blood clots. If it is above 125%, there is a risk of bleeding.
- D-dimer. Shows the process of blood clot formation. During pregnancy it may increase slightly. The normal value is from 33 to 726 ng/ml. If it rises sharply in a pregnant woman, this may indicate gestosis, diabetes mellitus, or kidney disease.
During pregnancy, it is very important to monitor all coagulogram indicators and, if necessary, undergo treatment
If pregnancy proceeds with complications, for example with gestosis, disturbances occur in blood coagulation. The lifespan of platelets decreases, fibrinolytic activity increases. In the absence of treatment for gestosis, there is a high probability of developing a severe complication - disseminated intravascular coagulation syndrome (DIC syndrome). At the first stage - hypercoagulation - many small blood clots form, blood circulation between mother and child is disrupted. Then comes hypocoagulation - the breakdown of blood clots when coagulation factors are depleted. And the third stage is the complete absence of coagulation (acoagulation), which leads to uterine bleeding and, most often, to the death of the fetus.
Deciphering the coagulogram of a pregnant woman is quite a difficult matter. Each woman is individual and each needs a special approach. Even if the indicators deviate slightly from normal values, do not panic. The main thing is to undergo all additional examinations on time and correct unwanted changes at an early stage together with your doctor.
At what stage of pregnancy is a coagulogram performed?
The question of how often to take a coagulogram during pregnancy cannot be answered unambiguously. The patient’s examination protocols indicate the need for hemostasiograms to be taken three times throughout the entire pregnancy, once per trimester:
- during registration (up to 12 weeks);
- at 20–24 weeks of pregnancy (time of the second screening);
- at 32–36 weeks of pregnancy (to prepare for delivery).
However, this test scheme is only suitable for those patients who do not have a complicated medical history, pregnancy proceeds without complications, and previous coagulogram results were within normal limits. In all other cases, the timing of the analysis is decided by the attending physician.
Important! Before any surgical intervention (appendectomy, cholecystectomy, cesarean section), donating blood for a coagulogram is mandatory!
Additional coagulation analysis may be prescribed for the following conditions:
- smoking during pregnancy;
- fetoplacental insufficiency;
- fetal hypoxia;
- delayed growth and development of the fetus;
- Rhesus conflict;
- varicose veins;
- history of infertility and miscarriage;
- multiple pregnancy;
- disruption of the cardiovascular, urinary and other organ systems.
Rules for taking a coagulogram test during pregnancy
Blood for hemostasiogram analysis is taken from a vein with a syringe. In order for the result to be the most reliable, it is necessary to prepare for a coagulogram test during pregnancy, adhering to such measures as:
- Before the procedure, do not eat food for 7-8 hours. Most often, blood donation occurs in the morning, so you must come on an empty stomach. In the morning you are allowed to take a couple of sips of water and brush your teeth.
- It is advisable to limit yourself from stress and anxiety during any tests.
- Avoid increased physical activity for two days preceding the procedure.
Detailed coagulogram during pregnancy: what indicators are included?
There are two types of coagulogram: standard and expanded. As a screening method, a standard type of coagulogram is used, including the following indicators:
- Tests for rheumatoid arthritis: what tests to take and their meanings
- APTT (activated partial thromboplastin time). This indicator determines the optimal time for the formation of a blood clot. A decrease in aPTT threatens the development of DIC syndrome (disseminated intravascular coagulation) in the postpartum period; an increase in the indicator means an increased risk of bleeding.
- Fibrinogen. It has a protein nature and is produced in the liver. Refers to the main link in thrombus formation. Fibrinogen levels increase slightly before labor. A sharp increase in the indicator is characteristic of the development of an infectious process.
- Thrombin time. Shows how long it takes fibrinogen to transform into fibrin, and then fibrin forms a blood clot.
- Prothrombin (or prothrombin index, PTI). It is one of the components of blood plasma. Shows how active the plasma prothrombin complex is compared to the plasma prothrombin time. An increase in the level of PTI is characteristic of placental abruption.
An extended coagulogram during pregnancy includes additional indicators:
- Prothrombin time (or PTT). An indicator showing how many seconds it takes to form thrombin from prothrombin, which is involved in the formation of a blood clot.
- Antithrombin III. This is a protein that slows down blood clotting. A decrease in it during pregnancy carries a risk of developing pathological thrombosis, and an increase carries a risk of bleeding.
- Platelets. Blood cells responsible for the state of the coagulation system. They are the ones who fill the fibrin networks, forming a blood clot. A slight decrease in platelets during pregnancy is a common occurrence, but significant fluctuations are a sign of pathology (a decrease in their production or, conversely, increased destruction). A significant decrease in the indicator carries the risk of developing DIC syndrome.
- INR (international normalized ratio). This is a calculated indicator characterizing the ratio of the patient’s prothrombin time to the total average thrombosed time. An increased INR carries a risk of bleeding, a decreased INR carries a risk of thrombosis. The indicator is often determined to monitor the condition when treating patients with anticoagulants and antiplatelet agents.
- D-dimer. One of the main indicators of the thrombus formation procedure. Determining d-dimer in a coagulogram during pregnancy and before conception makes it possible to timely identify the risk of thrombosis and begin timely treatment with anticoagulants.
- Lupus anticoagulant. Antibody formation indicator. Normally, it should be absent during pregnancy. Its presence in the blood indicates either the presence of autoimmune diseases or the development of Rh conflict.
- RFMC (soluble monomer complexes). An indicator that allows you to assess the massiveness of thrombus formation. During pregnancy, it can be 2–3 times higher than the non-pregnant norm. A significant increase occurs in shock conditions: disseminated intravascular coagulation syndrome, trauma, extensive thrombosis.
Normal values
In laboratories, methods for studying biomaterial and normal indicators may differ. Reference values are always indicated on the analysis results form. Table. Reference values of coagulogram.
| Main indicators of hemostasis | Norm |
| Clotting time | 5-10 minutes |
| APTT | 30-42 seconds |
| Thrombin time | 15-18 seconds |
| Prothrombin time | 9.3-13.3 seconds |
| Prothrombin index | 70-120% |
| INR (international normalized ratio | 0,82-1,18 |
Fibrinogen:
|
|
| Antithrombin III | 71-115% |
If the analysis data differs from the standard, it means that the patient has problems in the coagulation system.
Hemostasiogram - interpretation of indicators
A blood test for a coagulogram can be of two types:
- the main one - allowing to identify the quantitative content of fibrinogen, prothrombin, INR, aPTT and thrombin time;
- advanced - in addition to the main parameters, D-dimer, lupus AK and antithrombin are subject to study
- Fibrinogen is a coagulation factor formed from fibrin. The higher the amount of fibrinogen, the higher the risk of blood clots. The decrease in fibrinogen occurs synchronously with total protein in a biochemical blood test;
- Prothrombin and INR are indicators of blood clotting rate. Prothrombin is the second coagulation factor, and INR (international normalized ratio) is a laboratory indicator of the external pathway of the hemostatic system;
- APTT (activated partial thromboplastin time) is an indicator of blood clotting time from the moment of bleeding to the onset of clot formation against the background of reagents;
- Thrombin time is an indicator of the time (in seconds) during which a clot forms. In DIC syndrome, thrombin time is not determined;
- D-dimer is an additional indicator for assessing the blood coagulation system. It is a fibrin breakdown product. A significant increase may have a physiological etiology, since the D-dimer increases with increasing period;
- Antithrombin III is a specific protein responsible for blood thinning;
- Lupus anticoagulant is an indicator of the disease “systemic lupus erythematosus,” in which antibodies to blood enzymes are produced.
The table shows an example of normal values and deviations from the norm.
| Index | Norm | Pathology |
| fibrinogen | 4.0-6.0 g/l | Increase: heart attack, stroke, burns, postpartum period, surgical actions; Decreased: lack of vitamins, taking anticoagulants, development of disseminated intravascular coagulation |
| PV | 78-142% | Increased: thrombosis, taking thinning drugs; Decreased: DIC syndrome, blood diseases |
| TV | 10-18 sec | Increased: heparin use, liver failure, bleeding; Reduction: 1st stage of internal combustion engine |
| APTT | 17-20 sec | Increased: hemophilia, APS (rare); Decrease: bleeding, 1st phase of DIC |
| D-dimer | 1st trimester – 750 ng/ml 2 trimester up to 1000 ng/ml 3rd trimester up to 1500ng/ml | Increases in thrombophilia, disseminated intravascular coagulation syndrome, diabetes mellitus; A decrease in the indicator has no diagnostic value, with the exception of the therapy performed. |
| antithrombin | 70-115 % | Increase: taking anticoagulants; Decrease: thrombosis |
| Lupus AK | negative | Appearance means APS, HIV, Systemic lupus erythematosus |
Differences in results between pregnant and non-pregnant women
Indicators of the coagulation system have a significant difference between pregnant and non-pregnant patients:
- Why do my legs hurt during early and late pregnancy, what should I do?
- Fibrinogen in non-pregnant women is 2 units less.
- APTT is slightly elevated in women who are not in an interesting position.
- D-dimer is no more than 250 ng/ml.
Increasing values (extending interval)
- Liver pathologies;
- Uremia (intoxication of the body due to kidney disease);
- DIC syndrome;
- Deficiency of protein intake in the body;
- Pathological pregnancy (miscarriage, placental abruption);
- Cardiovascular diseases (heart attack, stroke);
- Pneumonia (pneumonia);
- Hyperbilirubinemia (increased levels of bilirubin in the blood);
- Tuberculosis (infectious disease caused by Koch's bacillus);
- Hypofibrinogenemia (with the level of fibrinogen in the blood less than 0.5 g per 1 l) in acquired or congenital form;
- Dysfibrinogenemia (defect in the structure of fibrinogen at the molecular level);
- Paraproteinemia (presence of defective and abnormal protein compounds in the plasma);
- An increase in fibrin and fibrinogen breakdown products in the blood;
- The presence of anticoagulants in the plasma (antithrombins, hirudin, heparin and others);
- Fibrinolytic therapy (a type of treatment aimed at restoring blood flow by dissolving a blood clot);
- Development of autoimmune antibodies to thrombin;
- Production of lupus anticoagulant (antibodies against enzymes of the circulatory system);
- Myeloma multiforme (cancer of blood plasma cells) and other oncological processes.
Preparation rules
You need to carefully prepare for the clotting test, following the following rules:
- Blood sampling is done only on an empty stomach;
- the fasting period should be at least 12 hours;
- on the eve of the procedure, do not eat spicy and fatty foods, smoked foods, and avoid alcohol;
- You should not smoke before donating blood;
- a few days before the analysis, stop anticoagulant medications (Aspirin, Citramon, Warfarin);
- Immediately before testing you need to be at rest.
Decoding the results
Hemostasiogram data are interpreted exclusively by the attending physician. Deciphering its results requires specific knowledge.
Basic analysis includes several indicators:
- Prothrombin time (PT) is how quickly a thrombin clot forms after adding calcium and thromboplastin to a sample. For adults this time is shorter than for children. This point of the hemostasiogram allows you to assess the effectiveness of anticoagulant treatment. If after therapy the PT value increases by at least 1.5-2 times, then it is considered effective.
- Activated partial thromboplastin time (aPTT) is the time period spent on the formation of a blood clot after the introduction of specific reagent substances. When calculating the APTT, the biochemical process of hemostasis is simulated, allowing one to evaluate the content of thrombus inhibitors, anticoagulants and plasma factors in the blood. APTT standards in individual laboratories may vary depending on the reagents used.
- Thrombin time (TV) - displays how long it takes for a blood clot to form after the addition of thrombin. This is the last stage of hemostasis, in which insoluble fibrin (the main component of a blood clot) is formed from fibrinogen under the influence of thrombin. TV helps diagnose congenital pathologies of the fibrinogen protein. Considered in conjunction with APTT and PT to assess the effectiveness of heparin therapy.
- Prothrombin index (PTI) is the percentage ratio of the reference prothrombin time to the same indicator (PT) of the blood being tested. Due to the use of different reagent substances by laboratories, this indicator may differ significantly. Recently, the international INR indicator has been used instead of PTI. It shows the ratio of the PV of the test sample and the PV of the control tube, therefore it is considered more significant.
- Fibrinogen is a protein produced by the liver, which is the first factor in the formation of blood clots. It is dissolved in the blood plasma and, under the influence of coagulation factors, precipitates, becoming the basis of a blood clot. The concentration of fibrinogen increases during infectious inflammation, injury and stress. This means that you should not take the test during acute respiratory infections and acute inflammatory processes.
- Antithrombin III is a natural anticoagulant that inhibits the activity of thrombin, preventing excessive clotting. The main place of its production is the liver. The indicator is valuable if there is a tendency to thrombosis.
These are just the main indicators of a simple (basic) hemostasiogram. They should be deciphered together, comparing with reference values.