The activated partial thromboplastin time (aPTT) test characterizes the state of one of the three mechanisms of the hemostatic system - coagulation (blood clotting). Using the APTT analysis, all types of hemophilia are diagnosed - A, B and C, as well as hereditary, autoimmune diseases and the phases of DIC syndrome are determined.
You can take the APTT test and get reliable results with a transcript of the analysis in the Laboratory of Hemostasis Pathologies at the MLC, the base clinic of Moscow State Medical University named after. Sechenov.
When is an APTT test prescribed?
APTT is part of the blood tests for hemostasis, which are taken when planning pregnancy. The test is also prescribed for genetic predisposition to thrombosis, spontaneous bleeding of unknown origin, diagnosis of hemophilia, treatment of heart attack, during pre- and postoperative examinations.
Based on the results of the analysis, the presence of coagulation inhibitors is determined - signs of systemic lupus erythematosus and antiphospholipid syndrome, severe autoimmune pathologies. The APTT test is also used to monitor heparin therapy.
Coagulogram
Factors of the coagulation, anticoagulant (anticoagulant) and fibrinolytic blood systems take part in the hemostasis system. A change in the functional state of one of the systems is accompanied by compensatory changes in the activity of the other. Violation of functional relationships can lead to severe pathological conditions of the body, consisting of either increased bleeding or intravascular thrombus formation. The study of the hemostatic system has the following goals:
- diagnosis of disorders in the hemostasis system;
- clarification of the admissibility of surgical intervention in case of identified disorders in the hemostasis system;
- monitoring treatment with direct and indirect anticoagulants, as well as thrombolytic therapy.
Currently, the usual practice for recognizing hemostasis disorders is heterogeneous and often varies in different clinics from performing one or two uninformative tests (prothrombin index, fibrinogen) to using an overloaded list of methods, some of which duplicate each other.
Many routine tests are outdated, of little value and inaccurate. To date, assessment of the results of prothrombin time using the prothrombin index is incomparable with global methodological approaches. Conditions for taking a coagulogram
Eating food, including juice, tea, coffee, and alcohol, is not allowed for 8 hours (preferably 12) before the test. You can drink plain water. If your doctor has prescribed a test while you are taking medications that affect blood clotting, please note this when taking the test.
List of coagulogram tests:
- Lupus anticoagulant;
- D-dimer;
- Antithrombin II;
- Thrombin time;
- APTT;
- INR (PTV, PTI);
- Fibrinogen;
- Screening for antiphospholipid syndrome.
Lupus Anticoagulant
Lupus Anticoagulant is an inhibitor of the blood anticoagulant system. Being present in the blood, it increases the coagulation activity of the hemostasis system, which adversely affects the process of implantation of the embryo, the course of the entire pregnancy, and the development of the fetus.
D-dimer (fibrin degradation product, D-dimer, Fibrin degradation fragment)
Determination of D-dimer level is a highly specific and sensitive marker of thrombus formation. However, its level also increases in pathological conditions accompanied by increased fibrinolysis: hemorrhagic complications, infections, wound healing, in the presence of rheumatoid factor in the blood, etc. However, the determination of D-dimer has important diagnostic value in the diagnosis of thrombosis. Its normal level allows, with 98% accuracy, to exclude conditions accompanied by increased thrombus formation.
Antithrombin III
AT III is determined by thrombin inhibition. AT III deficiency can be hereditary or acquired. The most common clinical manifestation of hereditary AT III deficiency is the development of deep vein thrombosis and, as a consequence, pulmonary embolism. The likelihood of developing thrombotic complications in patients with AT III deficiency increases with age.
Acquired AT III deficiency may be due to decreased synthesis, increased protein intake, or loss of protein. In all these cases, there is a parallel decrease in the concentration and activity of AT III. AT III is synthesized in the liver, so some liver diseases lead to decreased AT III levels. If, in parallel with the decrease in AT III, there is an increase in the thrombogenic properties of the vascular wall and activation of coagulation, then a further decrease in AT III is observed due to its consumption, which occurs in DIC caused by various pathologies: massive injuries, sepsis, inflammation of wounds, snake bites, complicated pregnancy, cancer, etc.
In addition, a decrease in AT III synthesis is observed during therapy with estrogens and synthetic drugs with estrogenic effects, nephrotic syndrome and gastrointestinal diseases, when the loss of protein exceeds the rate of its synthesis. In these cases, a parallel decrease in AT III and albumin is observed.
Thrombin time (TV)
Gives a general assessment of the final stage of blood coagulation. This is an indicator of the transition of fibrinogen to fibrin, the state of the anticoagulant system. Does not depend on the internal and external activation system, but depends on the concentration of fibrinogen, the presence of abnormal fibrinogen, the activity of antithrombins, the processes of polymerization and stabilization of fibrin.
In the clinic, TV determination is used to monitor heparin therapy (especially high molecular weight heparin) and fibrinolytic therapy; for the diagnosis of activation of fibrinolysis, indirect diagnosis of hypo- and dysfibrinogenemia.
Clinical and diagnostic value
TV shortening:
- hyperfibrinogenemia (more than 6 g/l);
TV extension:
- severe hypofibrinogenemia (less than 1.0 g/l), dysfibrinogenemia;
- heparin therapy with regular heparin (the test detects relatively low concentrations of the anticoagulant - from 0.05 IU/ml of blood);
- the presence of fibrin polymerization inhibitors (PDF, paraproteins, etc.);
- increase in immunoglobulins;
- use of asparaginase, streptokinase, urokinase;
- a decrease in fibrinase activity (factor XIII) does not affect thrombin time.
Activated partial thromboplastin time (APTT)
APTT evaluates the intrinsic pathway of activation of the coagulation process. The test is also called kaolin-kephalin time. It is a simple and comprehensive test, sensitive to deficiencies of all coagulation factors. But it is mainly used to evaluate factors VIII, IX, XI, XII and prekallikrein. Sensitive to excess plasma anticoagulants. Does not depend on platelet count.
This test is one of the main tests for monitoring heparin treatment. In patients receiving heparin therapy, the aPTT lengthens by 1.5–2 times, which indicates the effectiveness of treatment.
Determining the APTT allows you to finally resolve the issue of tolerance to heparin: for this purpose, the APTT is determined 1 hour before the next administration of heparin. If the APTT is prolonged by more than 2.5 times compared to the norm, an increased sensitivity to heparin is noted, its dose is reduced or the interval between injections is increased.
Clinical and diagnostic value
of test extension:
- hypocoagulation and bleeding tendency;
- hemophilia (A, B, C);
- significant deficiency of factors II, V, X, XII, fibrinogen;
- von Willebrand disease;
- heparin therapy with unfractionated heparin (the test detects low concentrations of the anticoagulant - from 0.05 IU/ml of blood);
- treatment with indirect anticoagulants;
- the presence of blood clotting inhibitors (PDF, lupus anticoagulant).
A shortened test indicates hypercoagulability and a tendency to thrombus formation;
and is also observed during normal pregnancy and taking oral contraceptives. Prothrombin (thromboplastin) time (PT)
By means of PT with calculation of the international normalized ratio (INR) and prothrombin index (PI), the external mechanism is assessed in total. Prothrombin time depends on the content of prothrombin itself - factor II, as well as factors V, VII, X and fibrinogen. Used to diagnose thromboembolic and hemorrhagic conditions, to monitor treatment with indirect anticoagulants.
Clinical and diagnostic value
Prolongation of prothrombin time (PI decreases, INR increases) - a tendency to hypocoagulation. Main reasons:
- violation of protein-synthetic function of the liver;
- vitamin K deficiency (usually due to impaired breakdown and absorption of fats in the intestines);
- treatment with indirect anticoagulants;
- deficiency of factors II, V, VII, X;
- heparin therapy with regular heparin (the test responds to relatively high concentrations of the anticoagulant - from 0.5 IU/ml of blood);
- hypo-, dysfibrinogenemia, impaired fibrin polymerization;
- the presence of clotting factor inhibitors (PDF, lupus anticoagulant);
- medications: anabolic steroids, antibiotics, acetylsalicylic acid in large doses, laxatives, methotrexate, nicotinic acid, thiazide diuretics, etc.
Shortening of prothrombin time is rare and has no independent diagnostic value. Together with a shortening of APTT, it indicates a tendency towards hypercoagulation:
- thrombosis;
- increased activity of factor VII (trauma, necrosis);
- pregnancy, childbirth;
- medications: acetylsalicylic acid in small doses, oral contraceptives, corticosteroids, vitamin K, barbiturates, antihistamines, caffeine.
Currently, recording the results of prothrombin time using the prothrombin index does not meet modern requirements.
To unambiguously interpret the results of prothrombin time measurements, regardless of the laboratory, INR is used: this method allows you to mathematically correct the difference given by thromboplastins with different sensitivities. Calculated using thromboplastin standardized to the international sensitivity index. Determination of fibrinogen content
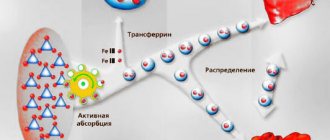
Its concentration is determined by the time of clot formation in diluted platelet-free plasma with the addition of excess highly active thrombin (according to Clauss). Fibrinogen is synthesized in the liver, from where it enters the blood. Changes in fibrinogen concentration are observed in various diseases - primarily in disorders of the hemostasis system and acute inflammation.
An increase in the amount of fibrinogen, even within normal values, is considered a risk factor for cardiovascular diseases.
Clinical and diagnostic value
Increased concentration (tendency to hypercoagulation):
- physiological (pregnancy, menstruation);
- mild forms of hepatitis;
- kidney disease;
- acute phase reactions, myocardial infarction;
- collagenoses;
- radiation sickness;
- malignant tumors (especially lung cancer);
- estrogens, oral contraceptives.
Decreased concentration (a decrease below 0.5–1 g/l causes bleeding):
- congenital afibrinogenemia, hypo- and dysfibrinogenemia;
- severe liver damage;
- condition after bleeding, injury, burn;
- bone marrow lesions (leukemia, tumor metastases);
- activation of fibrinolysis (including drugs);
- phenobarbital, anabolic steroids, unfractionated heparin in high doses.
In DIC syndrome, changes in coagulogram tests depend on the form and stage of the process.
Antiphospholipid syndrome (APL)
This is a group of diseases caused by the presence of antibodies to phospholipids. Antiphospholipid antibodies (APL) are autoantibodies of the IgG and IgM class, capable of binding to the antigenic determinants of phospholipids (cardiolipin, phosphatidylserine, phosphatidylinositol, phosphatidylic acid, phosphatidylcholine) and phospholipid binding proteins. Binding with cardiolipin occurs with the obligatory participation of a cofactor, rg-glycoprotein I.
The reasons for the production of APL have not been established. Presumably, long-term persistence of viruses that are tropic to the vascular endothelium causes: morphological and functional changes in endothelial membrane cells with the development of hypercoagulation syndrome, stimulation of B-lymphocytes, which under certain conditions produce aPL.
APL bind to phospholipids of cell membranes, changing the conformational and metabolic structure of the cell, which leads to disruption of cell function with the development of stasis and thrombosis. Due to the fact that vessels of different sizes and different locations are affected, the range of clinical manifestations of APS is diverse - thrombosis, strokes, obstetric pathology, thrombocytopenia. The incidence of aPL in various pathological conditions is presented below.
Pathological condition/APL detection frequency, %:
- Recurrent venous thrombosis: 28–71
- Recurrent miscarriage: 25–64
- Transverse myelitis: 50
- Thrombocytopenia: 27–33
- Hemolytic anemia: 38
- Arterial thrombosis: 25–31
- Pulmonary hypertension: 20–40
The most significant manifestation of APS is obstetric pathology associated with placental decidual vasculopathy - recurrent miscarriage, antenatal fetal death (usually in the 1st and 2nd trimester), severe forms of gestosis, intrauterine growth retardation.
In the population, aPL is found in 2–4% of the population. The incidence of aPL increases in patients with autoimmune, inflammatory, infectious diseases, malignant tumors, while taking oral contraceptives, psychotropic drugs. APS can be primary (there are no signs of other autoimmune diseases) or secondary (against the background of other autoimmune diseases, most often systemic lupus erythematosus). There is also a seronegative variant of APS, characterized by the absence of aPL and lupus anticoagulant in the presence of clinical manifestations of APS. In this form, only antibodies to glycoprotein I are detected.
The main criterion for the laboratory diagnosis of APS is the presence of aPL (or antibodies to cardiolipin) and lupus anticoagulant in 2 or more studies at least 6 weeks apart.
Indications for prescribing analysis for aPL:
- Obstetric pathology (recurrent miscarriage).
- Recurrent thrombosis of various locations.
- Systemic connective tissue diseases (systemic lupus erythematosus, Sjogren's syndrome).
- Thrombocytopenia.
- False-positive reaction to syphilis using cardiolipin antigen (RW, RPR).
Indications of basic coagulation tests
Test Deficiency and/or inhibition of factors/Effects of anticoagulants
XII, XI, IX, VIII, von Willebrandt, Fletcher, Fitzgerald factors V, X VII II (prothrombin) I (fibrinogen) direct/indirect.
- Thrombin time
- normal/normal/normal/extended/extended/extended/normal. - APTT
- prolonged/prolonged/normal/normal/prolonged/normal/prolonged/prolonged/prolonged. - Prothrombin time (INR)
- normal/extended/extended/extended/normal/extended/extended/extended. - Fibrinogen
- normal/normal/normal/reduced or undetectable/reduced or undetectable/normal/reduced/normal.
Note.
Prothrombin time (INR) results are inversely proportional to prothrombin index results. Outdated methods for studying hemostasis disorders and options for their replacement
Method/Disadvantages/Modern methods.
- Clotting time/Low standardization/APTT.
- Recalcification time/Low standardization/APTT.
- Plasma tolerance to heparin/Low standardization/Plasma thrombin-heparin time, determination of anti-Xa activity.
- Autocoagulation test (ACT)/Low standardization/APTT, antithrombin III activity.
- Beta-naphthol (fibrinogen B), ethanol or protamine sulfate tests / Low-informative, low-quality expression of results, often false positive / Tests for thrombinemia: quantitative determination of SFMC (soluble fibrin-monomer complexes).
Optimal complex of hemostasiological laboratory tests
Test/Hemostasis link/Diagnostic significance.
- Platelet count/Vascular platelet/Main component of platelet hemostasis.
- Von Willebrand factor (VWF)/Vascular platelet/Plasma platelet adhesion cofactor and marker of vascular wall endothelial damage.
- Prothrombin time (PT)/Procoagulant (extrinsic coagulation mechanism)/Screening test to determine the factors (fibrinogen, prothrombin, factors v, VII and X) involved in blood clotting initiated by high concentrations of tissue factor.
- APTT (aPTT)/Procoagulant (intrinsic coagulation mechanism)/Screening test to determine factors (fibrinogen, prothrombin, factors V, VIII, IX, X, XI, XII, prekallikrein and high molecular weight kininogen) involved in blood coagulation upon contact activation. A phospholipid-dependent screening test that provides insight into disorders associated with the effect of the lupus anticoagulant - VA.
- Thrombin time (TT)/Procoagulant (fibrin formation)/Screening test of the last stage of blood coagulation - reaction between thrombin and fibrinogen - anticoagulant activity of antithrombin III.
- Fibrinogen/Procoagulant (substrate)/The main substrate from which fibrin is formed under the action of thrombin.
- D-dimer/Procoagulant and fibrinolytic (activation of coagulation in vivo)/Fibrin degradation product, one of the most specific tests for the diagnosis of DIC syndrome, thrombophilia and thrombosis, a marker of thrombin formation, fibrin formation and activation of secondary fibrinolysis.
- Antithrombin III/Anticoagulant/Basic physiological anticoagulant, for which heparin is a cofactor, inactivates thrombin and active factors IX, X, XI, XII.
- Protein C / Anticoagulant / Physiological anticoagulant, in the activated state, inactivates active factors V, VII, inhibits plasminogen activator (activity manifests itself mainly in the microcirculatory bed).
- Lupus Anticoagulant (LA) Confirmatory Test/Done as part of an extended screening test to confirm the presence of LA.
It is possible that this range of studies is insufficient for patients with severe pathology of the hemostatic system, but in the case of preliminary screening and monitoring of therapy, it seems necessary and sufficient.
Benefits of analysis
APTT is a highly focused study that diagnoses several pathologies of hemostasis. The coagulation mechanism of hemostasis ensures the “sealing” of damage in blood vessels with fibrin clots and is influenced by blood coagulation factors.
Using the APTT test, you can detect a deficiency of the main factors affecting coagulation:
- 2nd, prothrombin;
- 5th, proaccelerin;
- 8th, antihemophilic globulin;
- 9th factor;
- 10th, Fr. Stewart-Prower;
- 11th, Dr. Rosenthal;
- 12th, Dr. Hagemann.
Normal indicators
| Index | Reference value | Unit |
| Prothrombin time | 9,0–15,0 | sec. |
| Prothrombin according to Quick | 78–142 | % |
| INR | depends on the presence of concomitant pathology in the patient for which he receives anticoagulant therapy | |
| APTT | 25,4–36,9 | sec. |
| Thrombin time | 10,3–16,6 | sec. |
| Fibrinogen | 2,00–4,00 | g/l |
| up to 5.6 (2nd and 3rd trimester of pregnancy) | g/l | |
Decoding
The standard for the test is 24-35 seconds. Physiological changes in hemostasis occur in the body of expectant mothers, so the APTT during pregnancy is reduced to 17-20 seconds. The type of pathology is determined based on the shortening or lengthening of the APTT.
What does it mean if APTT is higher than normal?
Prolongation of APTT is a sign of deficiency of blood coagulation factors: 8th in hemophilia A, 9th in hemophilia B, 11th in hemophilia C, as well as von Willebrand disease - an inherited tendency to spontaneous bleeding.
If the marker increases, additional tests are performed for lupus anticoagulant and antiphospholipid syndrome, and if the patient receives heparin injections, the dose of the drug is adjusted.
What does it mean if APTT is below normal?
A shortening of the activated partial thromboplastin time indicates the risk of developing thrombosis - blockage of blood vessels, or thromboembolism - a blood clot breaking off and entering the circulating blood. Low aPTT determines the first phase of disseminated intravascular coagulation.
If venous blood is collected incorrectly or the sample is contaminated, a decrease in the marker is also observed - in such cases, the analysis is repeated.
Indications for the purpose of the study
Coagulogram (hemostasiogram) is a comprehensive hematological study aimed at assessing the state of the hemostasis system (blood clotting), or blood clotting indicators. The hemostasis system includes blood cells (platelets) and specific substances (clotting factors) dissolved in blood plasma and contained in platelets. When the integrity of the vessel wall is violated, the coagulation system is activated and a blood clot is formed, preventing blood loss.
Some time after the bleeding stops, fibrinolysis begins - the process of dissolving the blood clot after restoring the damaged vessel wall to resume blood flow.
Indications for a coagulogram are conditions accompanied by increased bleeding or, conversely, increased thrombus formation.
Increased bleeding leads to hemorrhagic syndrome. It is manifested by the formation of hematomas, pinpoint hemorrhages under the skin (petechiae), bleeding of the mucous membranes (nosebleeds, bleeding from the gums), the appearance of blood in the stool, urine, prolonged menstrual bleeding, as well as possible hemorrhages in the internal organs and body cavities. The most dangerous manifestation of hemorrhagic syndrome is hemorrhage in the brain - hemorrhagic stroke, which can lead to rapid impairment of brain function, including death. A hereditary disease associated with blood clotting disorders (decreased or absent clotting factors) is called hemophilia.
The opposite situation - thrombosis - is the formation of blood clots (thrombi) inside blood vessels, preventing the free flow of blood.
People with obesity, diabetes mellitus, heart rhythm disturbances (the most significant of which are atrial fibrillation and flutter), low physical activity, and patients after major operations (for example, joint replacement, heart valve replacement, emergency operations, etc.) are at risk of increased thrombosis. , with varicose veins, previous myocardial infarctions, strokes, and various autoimmune diseases.
Thrombosis in a certain area of the vascular bed is accompanied by an acute or gradual disruption of the blood supply to any organ with disruption of its functions and subsequent tissue necrosis.
In addition to the above conditions, a coagulogram is performed before operations to assess the risk of bleeding, when prescribing certain medications, and also necessarily in case of liver diseases, since most of the proteins of the blood coagulation system are synthesized in this organ.
Where to get tested for APTT in Moscow
You can take an APTT test and get advice from an experienced hemostasiologist at the Women's Medical Center on Zemlyanoy Val. Our Hemostasis Pathology Laboratory has high-precision blood analyzers, high-quality reagents and consumables, which guarantees the reliability of the research results.
Along with the APTT test, you have the opportunity to take tests close to it: 2-TEG, extended hemostasiogram, tests for VA and APS, Antithrombin, and also determine the anti-Xa activity of heparin in the blood. In the experimental laboratory of the MLC, we are engaged not only in diagnostics: we research and practice new methods for treating hematological diseases.
In one of the private laboratories you are another statistical unit, but with us you are a patient who is ready to be helped by the best doctors in Moscow.
Preparation for the procedure
The essence of a coagulogram is to assess the activity of proteins of the blood coagulation system.
Therefore, proper preparation for this analysis is extremely important. Blood is taken on an empty stomach; the last meal should be at least 8-10 hours before the test. It is recommended to exclude excess amounts of fatty, sweet and protein foods. The drinking regime remains normal. The day before it is necessary to avoid stressful loads and intense sports. If the patient is taking any medications that affect coagulogram parameters, then, depending on the goals set for the study, it is necessary to either continue or stop taking them a few days before. This should be discussed with your doctor before taking the test.
If you need urgent results, you can contact the INVITRO offices, where express diagnostics are carried out. In this case, the analysis will be ready in about 2 hours.
Some of the proteins of the blood coagulation system are acute phase proteins. They are produced during stress, which includes not only physical and emotional stress, but also illness. Consequently, any persistent or short-term, but intense stress in the body can lead to changes in coagulogram parameters.
Dehydration (dehydration) is one of the reasons for blood thickening and an increase in the concentration of coagulation factors, which also leads to a distortion of the result.
The state of the blood coagulation system changes during pregnancy, both in the direction of increasing and decreasing the activity of a number of proteins.
The use of many medications affects the blood coagulation system. Thus, the first generations of oral contraceptives lead to an increased risk of thrombosis, and anticoagulants lead to bleeding. The list of drugs that affect the activity of the coagulation system is huge. When receiving any drug therapy, you should first consult with your doctor about the possible effect of a particular drug on the test result.
Taking certain medications by a pregnant woman, for example, warfarin, rifampicin, phenytoin, barbiturates, affects the production of clotting factors in the fetus. The child may subsequently be at high risk of bleeding.
Blood clotting mechanisms
Violation of the integrity of tissues and blood vessels activates the launch of a sequence of biochemical reactions of protein factors that ensure coagulation during bleeding. The final result is the formation of a blood clot from fibrin strands. There are 2 main pathways leading to blood clotting:
- internal - for its implementation, direct contact of blood cells and the subendothelial membrane of blood vessels is required;
- external - activated by the protein antithrombin III, secreted by damaged tissues and blood vessels.
Each of the mechanisms individually is ineffective, however, forming a close relationship, they ultimately help stop bleeding. Violation of the compensatory mechanisms of the hemostatic system is one of the reasons for the development of thrombosis or bleeding, which poses a threat to human life and health. This is what emphasizes the importance of timely diagnosis of the state of the hemostatic system.
How much does a coagulogram cost, when can I expect results?
You can take such an analysis at any private diagnostic center, and the cost will depend on the region and the pricing policy of a particular institution. In Moscow, a screening coagulogram will cost an average of 1000 rubles, and an extended one - 3500 rubles. Meanwhile, the study can be done free of charge, if there is evidence for it: just contact a doctor at your place of residence, present your compulsory health insurance policy and get a referral. A blood coagulogram is performed in any state laboratory at a clinic or hospital.
The period for receiving analysis results depends on the workload of the institution, but usually is no more than two days. In emergency situations, a hemostasiogram is performed immediately and the report is sent to the attending physician.
Expectant mothers have the right to a free blood coagulogram as part of pregnancy management and preparation for childbirth. If there are no signs of pathology, the analysis is performed three times, that is, in each trimester.
Video: Dr. Evdokimenko - simple tips on blood thinning, prevention of atherosclerosis and thrombophlebitis.
General information
Every qualified doctor knows that it is best to begin the treatment of any patient by collecting an anamnesis, which is nothing more than a collection of information about the state of a person’s health.
As a rule, any medical examination begins with asking the patient himself about previous diseases or surgical interventions, allergic reactions or hereditary predisposition to certain ailments, and so on.
Then the doctor prescribes a series of laboratory tests or simply tests that will help supplement the anamnesis with information about the development of the disease, as well as information necessary for choosing a treatment method or further diagnosis.
Coagulological studies (abbreviated as coagulogram ) occupy an important place among laboratory blood tests that are necessarily carried out in preparation for surgery, for example, during a planned cesarean section or during pregnancy .
To whom and why is a coagulogram prescribed?
The study of hemostatic and fibrinolytic properties of blood is indicated in the following situations:
- Preparation for planned or emergency surgery, including cesarean section;
- Heart and vascular diseases - myocardial infarction, stroke, coronary heart disease, atrial fibrillation, angina pectoris, pulmonary embolism, varicose veins, thrombophlebitis and deep vein thrombosis;
- Pathologies of the hematopoietic system - hemophilia, thrombocytopenia, anemia, von Willebrand-Diane disease, frequent nosebleeds, unexplained bruises, abnormally heavy menstruation and intermenstrual bleeding;
- Chronic liver diseases - fatty or alcoholic hepatosis, cirrhosis, hepatitis;
- Autoimmune diseases – scleroderma, rheumatoid arthritis, systemic lupus erythematosus;
- Pregnancy (for preventive purposes), severe toxicosis, gestosis, threat of miscarriage, miscarriage;
- Suspicion of existing DIC syndrome;
- Long-term use of hormonal contraceptives that thin the blood (Warfarin, Aspirin, Heparin, Trental and others);
- Treatment with hirudotherapy sessions.
Preparation and delivery of analysis
In order for the research results to be accurate and reliable, it is necessary to adhere to the following rules of preliminary preparation:
- Bring infants for analysis no earlier than 1 hour after feeding;
- Children aged 1 to 5 years should be brought in 2-3 hours after eating;
- Children over 5 years of age and adults should abstain from food for 12 hours;
- 30 minutes before donating blood for a coagulogram, sit down and calm down;
- Immediately before the analysis, do not smoke, stop drinking alcoholic beverages 24 hours before;
- Warn the laboratory technician about all medications taken the day before.
Blood for this study is taken from a vein in the elbow. It is very important that the hand in this place does not have any damage, otherwise platelets, fibrin or clotting factors may get into the sample, and this will distort the results of the coagulogram. For reliability, blood is drawn into two tubes, only the second of which is used for testing.
What does elevated D-dimer mean?
Even a slight increase in this indicator may indicate probable thrombosis. If the D-dimer reaches 273 ng/ml or higher, it is deadly.
D-dimer is elevated in many diseases:
- cardiac ischemia;
- acute coronary syndrome;
- thrombosis of the pulmonary artery (PE) or deep veins;
- DIC syndrome;
- acute or chronic heart failure;
- infections, injuries;
- sepsis;
- hematomas;
- kidney disease;
- preeclampsia and gestosis in pregnant women;
- coronavirus COVID-19;
- old age (over 80 years);
- malignant neoplasms.
The D-dimer level depends on the size of the clot, as well as the time and duration of taking thrombolytic drugs or anticoagulants.
With a decreased D-dimer level, the patient's risk of bleeding increases, so the patient needs to consult a hematologist and other specialists. Doctors conduct additional examinations and laboratory tests and prescribe an appropriate course of treatment.
What should the normal indicator be?
The normal level of D-dimer in blood plasma is 250 ng/ml. this indicator confirms that the patient is not at risk of thrombosis. In pregnant women, this figure can reach 1000 ng/ml or more, i.e. grow 3–4 times.
Normal D-dimer levels in pregnant women:
- up to 450–500 ng/ml in the 1st trimester;
- up to 900–920 ng/ml in the 2nd trimester;
- up to 1450–1500 ng/ml in the 3rd trimester.
If a pregnant woman, on the contrary, has a low level, she is urgently referred to a hematologist, who will prescribe medications. A decrease in dedimer during pregnancy is a sign of long-standing problems with blood clotting that arose long before pregnancy. With good treatment, childbirth proceeds normally.
Norms and interpretation of coagulogram during pregnancy
During the period of bearing a child, the total volume of circulating blood in a woman increases by an average of 25%. This is necessary to simultaneously serve the organisms of the expectant mother and fetus. In addition, you need to insure against extensive blood loss in case of miscarriage, premature placental abruption, and also before the decisive natural event - childbirth. Consequently, the activity of the blood coagulation and anticoagulation systems also increases during pregnancy: in the second trimester - by 15-20%, in the third - sometimes by 30% compared to a healthy woman who is not expecting a child.
It is very important to donate blood for a coagulogram three times during pregnancy. Deviations from the norm will promptly indicate to the doctor the risk of spontaneous abortion, uterine bleeding, fetoplacental insufficiency, gestosis, DIC syndrome, preeclampsia and eclampsia, as well as extensive blood loss during childbirth or during cesarean section.
Of course, expectant mothers are worried about this and want to know the interpretation of the results of a coagulogram during pregnancy. To begin with, we present to your attention a table of norms by trimester, and then we will tell you what deviations in the indicators mean.
| Indicator, unit | I trimester | II trimester | III trimester |
| Thrombin time, sec. | 10,6-13,4 | 10,4-13,2 | 10,2-12,8 |
| Prothrombin,% | 78-142 | 78-142 | 78-142 |
| APTT, sec. | 35,7-41,2 | 33,6-37,4 | 36,9-39,6 |
| D-dimers, ng/ml | Up to 286 | Up to 457 | Up to 644 |
| AVR, sec. | 60,1-72,6 | 56,7-67,8 | 48,2-55,3 |
| Platelets, *109/l | 302-316 | 274-297 | 241-262 |
| Prothrombin index,% | 85,3-90,1 | 91,1-100,4 | 105,7-110,5 |
| RFMK, units | 78-130 | 85-135 | 90-140 |
| Antithrombin III, % | 74 — 115 | 73 — 114 | 70 — 116 |
| Fibrinogen, g/l | 2,91-3,11 | 3,03-3,46 | 4,42-5,12 |
Interpretation of coagulogram results during pregnancy
Normally, the first trimester is characterized by some inhibition of both coagulation and anticoagulation functions of the blood, and then, as it approaches childbirth, the indicators increase. The table below shows the probable causes of deviations from the norms.
| Index | Decline | Promotion |
| APTT | Stage 1 DIC syndrome, thrombosis | Stage 2-3 of DIC syndrome |
| Prothrombin time and INR | Stage 1 of DIC syndrome, approaching labor | Stage 2-3 of DIC syndrome |
| Prothrombin | less than 70% – stage 1 of DIC syndrome | threat of placental abruption |
| Thrombin time | less than 10 seconds – stage 1 of DIC syndrome | more than 26 seconds – stage 2-3 of DIC syndrome |
| Antithrombin III | less than 50% of the norm – fetoplacental insufficiency, threat of placental abruption | threatened miscarriage, uterine bleeding, hepatitis |
| D-dimers | almost never occurs and has no significance | gestosis, diabetes mellitus, kidney failure |
| Fibrinogen | less than 3 g/l – severe toxicosis, gestosis, stage 2-3 of DIC syndrome, vitamin deficiency | Stage 1 DIC syndrome, acute infection, heart attack, stroke, malignant process |
| Lupus anticoagulant | the appearance indicates gestosis, preeclampsia, threat of miscarriage, placental abruption, premature birth | |
| RFMK | almost never occurs and has no significance | an increase of more than 4 times – stage 1 of DIC syndrome, threat of placental abruption |
If several indicators in a coagulogram during pregnancy deviate from the norm, this does not mean that the expectant mother and baby are in serious danger. Only if almost all study parameters are abnormal should the alarm be sounded.
In conclusion, I would like to emphasize that only a qualified gynecologist can draw the right conclusions by looking at the results of a hemostasiogram of a pregnant woman. Each organism is individual, and while carrying a child, everyone adapts differently to changing conditions. You should not make hasty conclusions and panic ahead of time - this in itself is very harmful during such a period. Take care of yourself and be healthy!