Cerebral structures require increased nutrition, since nervous tissues in general are the most voracious in the entire body.
Changes in the quality of trophism and the rate of provision of useful substances affect the state of structures right away. It takes 30 to 50 seconds for loss of consciousness to occur. The vascular network of the brain is very branched and quite fragile. Therefore, there is a real, increased risk of encountering emergency conditions.
Brain hemorrhage is a dangerous pathological process in which the arteries cannot withstand one or another negative influence, rupture, after which liquid connective tissue flows outside the vessels.
There is also a less common factor in which the artery remains intact, but its permeability increases significantly and blood cells can extend beyond the walls without obstacles or problems.
The condition is extremely serious and is accompanied by severe symptoms. Mortality averages 60%. There is evidence of less favorable figures. At least 85% of patients become disabled after hemorrhage. The main age category of victims is 50-65 years old, with a tendency to increase as the body ages.
The condition also has a more well-known synonym – hemorrhagic stroke. It is the same. Let's try to figure out what you need to know about the pathological process, its features, causes and symptoms.
Mechanism of formation
The development of the disorder is based on one factor or several pathogenetic factors at once. What exactly can affect the likelihood of a violation:
- Cardiovascular diseases. Represented by a wide group of diagnoses. In the vast majority of cases, hemorrhagic stroke develops as a complication of long-term and untreated hypertension. That is, a stable and pronounced increase in blood pressure.
Statistics show that the mechanism accounts for up to 85% of the total number of hemorrhages. This is the absolute majority. The only way to prevent an emergency condition is to undergo high-quality treatment of the underlying pathology.
- Metabolic disorders. Basically, deviation of lipid movement. That is, a disorder in which the rate of deposition and elimination of fats significantly deviates from the conventional norm.
The pathological process leads to another problem - atherosclerosis. When cholesterol deposits form on the walls of blood vessels, which interfere with blood flow. The result is that the likelihood of hemorrhagic stroke and death from complications increases significantly.
- Hormonal imbalance. We are talking about a variety of disorders: from changes in the quality and intensity of the synthesis of sex substances to problems with the production of insulin and compounds of the adrenal cortex.
- Hereditary causes. The mechanism is associated with a not yet fully understood method of transferring risks from parents to children. The disease itself, of course, is not transmitted.
If a mother, father, grandmother, grandfather has a hemorrhagic stroke, this does not mean that the same thing will happen to a descendant. But the likelihood is growing. Apparently - by several tens of percent. The topic has not been fully studied, research continues.
- Toxic damage to the body. Poisoning by vapors of non-metals, some medications. The risk of hemorrhagic stroke increases with the systematic use of antiplatelet agents, anticoagulants, and hormonal agents.
- Some forms of anemia, blood diseases. Changes in the rheological properties of connective tissue lead to disruption of the speed and quality of trophic systems and an increase in blood pressure. In some cases, vascular permeability increases. The result is an increased risk of cerebral hemorrhage.
Mechanisms exist in isolation or are combined with each other. This question needs to be clarified, since the therapy strategy and its essence depend on the origin of the pathological process.
Brain hemorrhage
A cerebral hemorrhage is nothing more than a hemorrhagic stroke. Recently, the prevalence of this disease has shown an increasing trend. The consequences of such a stroke, especially a large one, can be very serious and can be fatal.
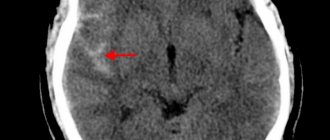
Hemorrhagic stroke most often develops when arteries rupture. The spilled blood soaks part of the brain, which is why this type of stroke is also called a cerebral hemorrhage. Most often, hemorrhagic stroke occurs in people suffering from arterial hypertension and develops against the background of increased blood pressure. At some point, the vascular wall cannot withstand the sharp rise in blood and ruptures. A more rare cause of hemorrhagic stroke is a ruptured aneurysm. An arterial aneurysm is usually a congenital saccular protrusion on the wall of a vessel. The wall of such a protrusion is thinner than the wall of the vessel itself, and a slight increase in blood pressure in stressful situations or during physical exertion is often enough to rupture it.
A rupture of a vessel on the surface of the brain allows blood to enter the space surrounding the brain (subarachnoid space). This type of stroke is called subarachnoid hemorrhage. The most common cause is a ruptured aneurysm.
Symptoms of a stroke:
- sudden weakness;
- paralysis or numbness of the muscles of the face, limbs (often on one side);
- speech impairment;
- blurred vision;
- severe sharp headache;
- dizziness;
- loss of balance and coordination, gait disturbance.
Causal factors of hemorrhage
Knowing the causative factors that can lead to cerebral hemorrhage will help prevent their effects on the body. The main factors are:
- arterial hypertension (chronic increase in blood pressure, especially when there is no treatment for this pathology);
- diabetes mellitus (a condition that develops with a constant increase in blood glucose levels, against which various complications develop);
- vascular aneurysms (expansion of an artery along any length), which can be either congenital or acquired during life;
- traumatic damage to cerebral vessels, especially after injury from a sharp object;
- hemorrhagic diathesis (conditions that are accompanied by increased fragility of the vascular wall);
- uncontrolled use of anticoagulants (drugs that prevent blood clotting). They are usually prescribed after thromboembolic conditions;
- damage to blood vessels by amyloid (a substance that is deposited in the vascular wall and leads to a change in the strength of the vessel);
- tumor lesion;
- infectious and inflammatory process in brain tissue (encephalitis) and others.
Regardless of the primary cause affecting the nervous tissue, a change in vascular permeability occurs towards its increase. Ultimately, this leads to rupture of the vascular wall. This is accompanied by the appearance of hemorrhage in the brain. However, very rarely, diapedetic intracerebral hemorrhage may appear, which is characterized by the release of formed elements of blood and plasma through an intact vascular wall. This becomes possible as a result of the expansion of the spaces between endothelial cells (choroid cells). This is how damage to the brain or spinal cord occurs.
Most often, cerebral hemorrhages affect the cerebral hemispheres. Less commonly, hemorrhages may develop in the brainstem or cerebellum. A hemorrhagic stroke that affects the brain stem leads to disruption of vital functions, since the respiratory center, the center of the cardiovascular system, etc. are located in the medulla oblongata. The consequences in this case are very serious. The symptoms in this case are vivid and progress quickly. Therefore, signs of such hemorrhage are easily diagnosed. In this case, surgery is the only method of salvation, but it is not always effective.
Treatment of hemorrhagic stroke
Treatment of hemorrhagic stroke is aimed at quickly stopping the hemorrhage formed in the cerebral artery, as well as removing a blood clot from it that puts pressure on the brain. In such cases, neurosurgical surgery is indicated.
In addition, when treating hemorrhagic stroke, high blood pressure pills are prescribed, which must be taken strictly as prescribed by the doctor.
Classification
The condition is divided according to three bases. The first criterion is the localization of the violation. The most common variants of the disorder are:
- Lateral.
- Lobar.
- Subcortical or subcortical.
- Thalamic.
- Cerebellar.
- Mixed.
- Stem.
Most likely, this terminology will mean nothing to a patient without special knowledge. The point is different. Depending on the location of the pathological change, the symptoms will be one or another. Plus, prognoses are determined by the essence of the disorder and its location. You need to clearly know where the hemorrhage occurred.
Another basis for classification is the type of lesion.
Highlight:
- Actually parenchymal process. When blood enters the brain tissue and permeates it. It is considered a very dangerous type of disorder. Potentially more lethal than the second one.
- Subarachnoid hemorrhage. Liquid connective tissue extends into the space between the cerebral membranes. The main pathological effect concerns compression of the brain, as a result of increased intracranial pressure.
However, the risks are less. Since there are not as many factors of damage as in the first case.
The third basis for classification is the severity of the pathological process.
These options are called:
- Mild degree. If the amount of bleeding into the brain is minimal. Happens quite often. In some cases, the patient does not understand at all what happened until neurological disorders increase. The outlook for recovery is good.
- Average degree. There is a pronounced clinical picture. Everything is noticeable from the very first second of the pathological process. Deviation requires urgent hospitalization and treatment in an intensive care unit. Even in this case, the chances of recovery are rather dim.
- Severe form. Doesn't bode well for the patient. In more than 80% of cases, a person dies from massive death of brain tissue. In 20% of situations he remains deeply disabled for the same reasons. There is almost no chance of restoring at least the basic functions of cerebral structures and ensuring adequate life activity.
These classifications are actively used in medical practice to describe the pathological process, its essence and dynamics.
Causes
Development factors have already been named earlier; it is worth specifying the described mechanisms and identifying the exact provocateurs. Among them:
Hypertension
Stable increase in blood pressure. It is considered an independent cardiovascular disease. It occurs frequently, especially in patients of the older age group. Almost in 90% of cases, albeit to varying degrees of severity.
The higher the blood pressure level, the more serious the risks. Since the vessels are in a state of constant increased load, they wear out faster. At a certain point, they simply cannot stand it and burst. Which leads to an emergency.
The cause of cerebral hemorrhage is an excessive impact on the internal lining of the artery, its muscle layer, dystrophy and, as the final result, a sharp rupture and leakage of liquid connective tissue.
Diabetes
An endocrine disease that stands apart. It is characterized by a stable, regular increase in blood sugar levels.
In addition, the pathology poses a danger to all tissues of the body. First of all, it is the blood vessels that suffer. A pathological narrowing of the lumen of the arteries develops. The tissues do not receive enough nutrition.
In addition, the phenomena of degeneration of the internal lining and muscle layer are increasing. The result is the same as in the previous case.
The disease cannot be treated as such, so the likelihood of encountering a hemorrhagic stroke is enormous and is growing every year.
By the way, this is one of the main factors in the death of patients with diabetes.
Smoking
Subjective reason. The problem is not only and not so much with nicotine, but with other toxic substances. The quality of vessels is affected by cadmium, arsenic vapors, sulfur structures, carbon compounds and other chemicals.
If you smoke regularly, the likelihood of a stroke increases. Because the vessels quickly wear out and narrow.
Alcohol consumption
About the same thing happens, only the poisons are different. When ethanol is processed, acetaldehyde and acetic acid are produced. They are dangerous for the heart and arteries. Which becomes the culprit that provokes hemorrhage.
Drug use
According to research, patients who love cocaine and synthetic stimulants are especially at risk.
The cause of intracerebral hemorrhage is thinning of the walls of blood vessels, increased pressure, and degeneration of the arteries. The result is obvious.
Arrhythmias
Oddly enough, the very nature of cardiac output determines the condition of the blood vessels. It turns out that the load on the arteries is distributed unevenly. Sometimes she is high, sometimes she is low. The pressure rises and falls.
In such an emergency mode, the body works constantly. This can't end well. The result of arrhythmias is cerebral hemorrhage. Provided that rhythm disturbances are not corrected in a timely manner.
Read more about the types of arrhythmias, possible risks and treatment here.
Atherosclerosis
Deposition of fatty compounds on the walls of blood vessels. Cholesterol plaques interfere with blood flow. The result is increased pressure as local resistance has to be overcome.
Gradually, the artery wears out, a wall protrusion of the vessel (aneurysm) is possible, then the likelihood of hemorrhage increases significantly. It makes sense to treat the disease at the earliest stage, while the chances of recovery are high enough.
Vascular defects
Congenital or acquired disorders. For example, too narrow a lumen or degeneration of the walls. Various options are possible. The bottom line is that they potentially increase the likelihood of a stroke.
If such a change is detected, you need to adhere to the rules of prevention: do not overexert yourself physically, eat right, etc. The treating specialist helps develop the strategy.
Heart defects
Also congenital or acquired. Most often, anatomical changes in the condition of the valves occur.
There are more dangerous variants of the pathological process, complex ones. Read more about the types of heart defects here.
Treatment is carried out by cardiology specialists and specialized surgeons.
Obesity
Increased body weight is associated with two disorders: increased blood pressure (hypertension) and changes in the nature of lipid metabolism (atherosclerosis).
Anemia
Basically, rare forms of the pathological process. The disorder is caused very rarely, in no more than 0.5% of cases.
Wrong lifestyle
A diet high in fat, carbohydrates, also sitting in one place, lack of mobility (so-called physical inactivity). They increase the risk, but do not themselves cause cerebral hemorrhage.
Hormonal imbalances
An increase in the concentration of substances in the adrenal cortex, pituitary gland or thyroid gland.
Use of certain drugs
To increase blood flow, oral contraceptives, and other medications.
These reasons need to be eliminated as quickly as possible. In the early stages, it is still possible to prevent the irreparable.
How to avoid a stroke?
Symptoms of a stroke appear suddenly. You can’t be prepared for this, and there is no magic pill that will neutralize an attack. Therefore, it is very important to follow stroke prevention measures.
In 25% of patients, a repeat case is recorded in the next 5 years. To prevent an attack, you must adhere to the following rules:
- lead a healthy and active lifestyle. Proper nutrition and regular exercise will help reduce weight, blood pressure, and improve vascular elasticity;
- control blood pressure and cholesterol levels in the blood. Eat less fatty foods and take medications if necessary;
- monitor your blood sugar levels (read how to treat diabetes);
- quit smoking;
- do not be nervous;
- check your health.
At the resort, you can undergo a vascular and cardiovascular disease treatment program to reduce the likelihood of a stroke in the future.
Subscribe to our blog to learn even more about how to stay healthy - treatment methods, disease prevention, as well as relaxation in the Caucasian Mineral Waters.
Precursor symptoms
The preceding signs or so-called aura do not always develop. This is rather an exception to the rule, since in most cases the opposite is observed.
Hemorrhage occurs suddenly. If we talk about manifestations that will indicate the approach of an emergency condition, they can be as follows:
- Intense heat in the chest, flushing of the face. A sudden sensation that comes out of the blue. As a rule, there are no objective reasons.
- Numbness of half the face. In addition, tingling may occur. Paresthesias indicate sudden, acute ischemia. This is a very alarming sign, even if nothing followed after it. You need to pay close attention to such “calls” and urgently run to the doctor.
- Problems with speech perception. The native language that a person has spoken for many years suddenly turns out to be incomprehensible. This is the first sign of a malnutrition of the temporal lobes of the brain, into which blood may bleed.
- Problems with coordination of movements. Acute dizziness. May result in a fall and injury.
Attention:
Aura or precursors of a pathological process occur in only 5-10% of the total number of cases. Much more often, the disorder debuts directly from the main clinic.
All possible symptoms of pre-stroke in women are described in detail here.
Signs of the acute phase
{banner_banstat9}
The complex of manifestations of the deviation is very bright and clearly visible, since the lesion is severe.
Hemorrhagic stroke is much more severe than its ischemic “brother”, since a whole group of factors accumulate that affect the functional activity of the brain.
Among them:
- Actually, an acute malnutrition of that part of the cerebral structures that received oxygen and nutrients through the destroyed vessel. As a rule, in the case of ischemic stroke, this is where it all ends. But not with cerebral hemorrhage.
- Inflammatory, necrotic processes in the very focus of trophic disturbances. They develop almost immediately. Pathological changes continue and complicate them. Both the main vessel itself and the nervous tissue at the local level suffer, which only aggravates the situation.
- Inflammation in the periphery. Changes in the structure of nerve tissue outside the lesion itself.
- Compression of the brain by a clot of accumulated blood. The space of the cranium is closed and does not change. Therefore, any deviations of this kind are potentially fatal and dangerous.
Liquid tissue puts pressure on nerve fibers and causes secondary ischemic processes, and then possible necrosis with the gradual development of neurological deficit.
Symptoms of hemorrhage in the brain are caused by the cumulative effect of various damaging factors, compression, necrosis at the source of the stroke, ischemia of tissues that do not receive nutrition and oxygen.
As for the clinical picture itself, the signs will be as follows:
- An acute headache, unbearable and very strong, is the first manifestation of hemorrhage in the structures of the brain. It occurs with lightning speed, suddenly and provokes forced body positions. The person tries to find a position in which the sensation will be less noticeable.
For reference:
The pain goes away gradually, as tissues die further and the pathological process worsens, which is quite remarkable.
- Dizziness. Changes in the perception of space, disturbances in orientation in the surrounding reality. The person also cannot coordinate his own actions. Forced to take a sitting or lying position. In the place where he was caught in an emergency.
- Speech disorders. Because the facial muscles and the entire articulatory apparatus are paralyzed. There may also be problems with the perception of other people's statements. Aphasia develops suddenly and lasts for many months.
Attention:
If the patient is lucky enough to survive and not remain a “vegetable,” speech function will have to be restored for at least a year.
Read more about the rehabilitation process after a stroke in this article.
- Nausea, vomiting. They develop just as suddenly. Moreover, it does not matter at all whether a person took food or not.
- Numbness of half the body. The result of paralysis or paresis. The disorder affects the side opposite the one where the cerebral hemorrhage occurred. Since the organization of nervous activity is mirror, cross. Gradually, sensitivity may be restored or only become stronger.
- Intolerance to sounds and smells. Everything that affects analyzers and sense organs. All such effects provoke an attack of severe headache, nausea and vomiting. All manifestations become more intense.
- Tachycardia. Increased heart rate. Reflex phenomenon. It usually does not pose a great danger, but creates additional discomfort for the patient.
- The simplest visual hallucinations. Signs of cerebral hemorrhage are flickering flies, lightning, bright dots before the eyes, the patient sees flashes of blue, golden color, black spots and geometric shapes. This is the result of poor nutrition of the occipital lobe of the brain. In the absence of a sufficient amount of oxygen, the cortex becomes excited and begins to produce non-existent images.
- Loss of consciousness. Fainting is a typical sign of cerebral hemorrhage and develops in 4 stages: from a feeling of unreality to the actual syncope episode. On average, it takes from 1 to 5 minutes for the state to fully develop. With extensive bleeding, coma is possible.
These are common signs of the disorder.
Stroke: types, risk group and signs
Stroke is an acutely developing dysfunction of the nervous system due to damage to the blood vessels of the brain.
There are three types of stroke:
- ischemic - as a result of occlusion (impaired patency) of blood vessels, blood clots or atherosclerotic plaques block blood vessels in the brain. Leads to a heart attack.
- hemorrhagic - bleeding into the brain tissue. Leads to a heart attack.
- Transient cerebrovascular accident (TCVA) lasts 2-5 minutes, during which blood does not flow to the brain. It develops over time and does not lead to a heart attack.
Who is at risk?
At risk are people who:
- have hypertension;
- have heart disease;
- suffer from excess weight;
- genetically predisposed to stroke;
- smoke;
- over 55 years old;
- have elevated blood cholesterol levels;
- suffer from apnea;
- They move little.
Stroke occurs more often in men. Blood pressure problems are one of the common causes of stroke. If you have sudden surges in blood pressure, it may also be helpful to read how to treat hypotension and how to treat hypertension.
How can you tell if a person is having a stroke?
A distinctive feature of all signs is that they occur abruptly. Suddenly:
- numb face, arms, legs;
- difficult to pronounce words;
- vision has deteriorated;
- severe headache;
- balance and coordination of movements are impaired.
Social reminders contain three points to check:
- a person cannot smile;
- cannot raise both arms;
- unable to pronounce his name clearly.
If a stroke is confirmed, diagnosis is carried out in a hospital setting.
How to help a person with a stroke?
It is important to provide assistance to the patient as soon as possible in order to stop the process of brain destruction. The sooner help is provided, the less consequences there will be for the brain! Save the memo “What to do before the ambulance arrives”:
Consequences of an attack
Although a stroke occurs when there is a problem in the brain, the effects are not limited to the brain. After a stroke, other parts of the body may remain paralyzed. Speech and memory may deteriorate and not recover. Depression and mood swings may appear.
Focal manifestations
{banner_banstat10}
In this case, everything depends on the localization of the pathological process, which part of the cerebral structures does not receive enough nutrition and oxygen.
- If the frontal lobe is damaged, epileptic seizures, disturbances in behavior, thinking, and motor activity occur.
- Parietal region - disorders of smell, touch, loss of the ability to count and read.
- Temporal structures - auditory deceptions of perception, convulsive seizures, memory impairment.
- Occipital lobe - visual hallucinations, vision problems.
- Cerebellum and extrapyramidal system - loss of balance, movement coordination disorders, dizziness.
Attention:
In case of hemorrhage in the brain stem - dysfunction of breathing and cardiac activity. Patients die in 100% of cases.
The clinic urgently needs to stop, just like the primary pathological process.
The bleeding is extremely severe. In 50–90% of cases, death is observed.
The severity of symptoms is determined by the formation of secondary brainstem symptoms - swelling of the brainstem, displacement, herniation.
The spilled blood triggers a whole cascade of biochemical reactions, leading, in the first 2 days, to the development of vasogenic cerebral edema (acute period). On the third day, delayed vasospasm develops, which leads to the development of necrotizing angiopathy and calcium cell death.
It is possible for hemorrhage to develop through diapedetic bleeding - due to prolonged spasm of the vessel, slowing down the blood flow in it, and its subsequent persistent expansion. In this case, disruption of the functioning of the endothelium occurs, the permeability of the vessel wall increases, and plasma and blood elements leak out of it into the surrounding tissues. Small hemorrhages merge to form hemorrhagic foci of various sizes.
You should be especially careful about headaches. It may be a harbinger of a brain catastrophe.
The development of stroke is acute (apoplexy), sudden with a rapid increase in neurological symptoms.
Rapidly growing headache - especially severe, with nausea and vomiting, “hot flashes and pulsations” in the head, pain in the eyes when looking at bright light and when rotating the eyes to the sides, red circles before the eyes, breathing problems, palpitations, hemiplegia or hemiparesis ( paralysis of the limbs of the same name - right-sided or left-sided), impaired consciousness of varying degrees of severity - stunning, stupor or coma. Here is a scenario for the development of a hemorrhagic stroke.
A sudden onset of the disease with the development of an epileptic attack is possible. Against the background of complete health on the beach, during strong emotions at work, during an injury, a person falls with a cry, throws back his head, convulses, breathes hoarsely, foam comes out of the mouth (possibly with blood due to biting the tongue).
The gaze is turned towards the hemorrhage, the patient seems to be looking at the affected side of the brain, on the side of the hemorrhage there is a wide pupil (mydriasis), possibly divergent strabismus, the eyeballs make “floating” movements, the gaze is not fixed; on the side opposite to the hemorrhage, atony (drooping) of the upper eyelid develops, the corner of the mouth droops, and the cheek does not hold air when breathing (the “sail” symptom).
Meningeal symptoms appear - it is impossible to tilt your head forward and touch your chin to the chest, it is impossible to lie on your back and bend your leg at the hip joint to straighten it at the knee.
The course of extensive hemorrhages in the cerebral hemisphere can be complicated by secondary stem syndrome. Disturbances in breathing, cardiac activity, and consciousness increase, muscle tone changes in the form of periodic tonic spasms with a sharp increase in tone in the extremities (hormetonia) and increased tone of the extensor (extensor) muscles and relative relaxation of the flexor muscles (decerebrate rigidity), the development of alternating syndromes is possible ( syndromes that combine damage to the cranial nerves on the side of the hemorrhage with disorders of movement and sensitivity on the opposite side).
43-73% of hemorrhages end with a breakthrough of blood into the ventricles of the brain. When blood breaks through into the ventricles, the patient’s condition sharply worsens - a coma develops, bilateral pathological signs, protective reflexes appear, hemiplegia is combined with motor restlessness in non-paralyzed limbs (violent movements seem conscious (patients pull the blanket over themselves, as if they want to cover themselves with a blanket), hormetonia, symptoms of damage to the autonomic nervous system deepen (chills, cold sweats, a significant increase in temperature) The appearance of these symptoms is prognostically unfavorable.
At the first symptoms of a stroke, immediate help is required - you need to call an ambulance and hospitalize the patient.
Diagnostics
There is not much time for examination. It is necessary to urgently take the person to the hospital, study his general condition and begin action.
The emergency list of activities is as follows:
- Blood pressure measurement.
- Quickly interview the patient if he is conscious.
- Listening to heart sounds.
- Basic neurological examination. Checking reflexes.
Next, primary measures are taken to restore the functional activity of the body. Once the condition becomes stable, there is time to study the situation in more detail.
Special examinations are prescribed:
- Anamnesis collection.
- Doppler ultrasound of the brain. Duplex scanning of vessels of cerebral structures. To assess the quality of local blood flow.
- REG. In order to identify the electrical activity of nerve tissue.
- MRI. To assess the extent of damage and prospects for recovery. Develop treatment tactics.
- Hormone analysis, as well as blood biochemistry with an expanded picture of the lipid spectrum.
Diagnosis is carried out under the supervision of a neurologist. A cardiologist, neurosurgeon, and endocrinologist are also involved, if necessary.
Time is running out. The first few days and even months there is a real risk of relapse. No one survives a second hemorrhagic stroke.
Read the full algorithm for providing first aid for a stroke here.
Treatment
Therapy is etiotropic and symptomatic. That is, it is necessary to fight both the manifestations and the causes of the pathological process.
If we talk about correcting the main factor:
- Hypertension. Drugs are prescribed to lower blood pressure. Calcium channel blockers, ACE inhibitors, sartans, centrally acting agents, diuretics. In strictly controlled dosages.
- Diabetes. Diet low in carbohydrates and without sugar. Insulin as needed during an acute attack.
- Bad habits. Refusal of cigarettes, alcohol, drugs. If necessary, get help from a narcologist.
- Arrhythmias. Specialized means for recovery: Amiodarone, Quinidine, beta blockers.
- Atherosclerosis. Fibrates, statins, nicotinic acid. Diet correction.
- Heart and vascular defects. Operation. Plastic or prosthetics.
- Anemia. Depends on the type. The use of iron supplements, vitamins, etc.
- Hormonal imbalances. Correction with synthetic substituents or other methods. Depends on a situation.
- Wrong lifestyle. Sufficient level of physical activity, drinking regime, etc.
- Use of certain medications. Refusal or replacement of medications.
Treatment of cerebral hemorrhage concerns eliminating the very cause of the pathological process and correcting the symptoms of the disorder.
Prevention
The disease is extremely serious and dangerous. It is much easier to avoid it than to treat it later. Prevention measures include:
Blood pressure control
- proper nutrition;
- monitoring weight changes (especially when you are overweight);
- control of blood pressure, preventing its increase;
- fight against atherosclerotic phenomena;
- getting rid of bad habits - smoking, alcohol;
- If possible, avoid stress and overexertion.
To prevent relapse, restorative and vitamin preparations are prescribed. Constant supervision by a specialist is required.