What do your tests say?
Leukocytes
Leukocytes are usually called a large group of cells, united under the definition of “white blood cells”. These are colorless blood cells. They come in several types: lymphocytes, monocytes, basophils, eosinophils and neutrophils. All of them have a nucleus and are capable of active amoeboid movement. The role of leukocytes in our body is enormous and very important. They absorb bacteria and dead cells and produce antibodies. These are our protector cells. Without them, no immunity would be possible and, accordingly, any kind of fight by the body against disease would be impossible.
Leukocytes can be found not only in the blood, but also in the lymph. This type of leukocyte is called lymphocyte. According to their structure, all leukocytes are divided into granular and non-granular. Each type of leukocyte guards the safety of the body in its own way, that is, it performs its own specific functions.
Lymphocytes produce a special type of proteins - antibodies, which neutralize foreign substances and their poisons that enter the body. Some antibodies “work” only against certain substances, others are more universal - they fight the pathogens of not one, but several diseases. Due to the long-term preservation of antibodies in the body, its overall resistance increases. Monocytes, also known as blood phagocytes (from the Greek “phagos” - devouring) absorb pathogens, foreign particles, as well as their remains.
- Neutrophils are capable of phagocytosis, like monocytes. But their function as body cleansers is even broader: neutrophils destroy viruses, bacteria and their waste products - toxins; they detoxify the body, i.e. disinfect it.
- Eosinophils - participate in inflammatory processes, allergic reactions, cleansing the body of foreign substances and bacteria.
- Eosinophils contain antihistamines that manifest themselves in allergies.
- Basophils - contain histamine and heparin, save the body in case of inflammation and allergic reactions.
The average number of leukocytes ranges from 4 to 9 thousand in 1 μl of blood. The quantitative relationship between individual forms of leukocytes is called the leukocyte formula. Normally, leukocytes are distributed in the following ratios:
- basophils - 0.1%,
- eosinophils - 0.5-5%,
- band neutrophils 1-6%,
- segmented neutrophils 47-72%,
- lymphocytes 19-38%,
- monocytes 2-11%.
If changes occur in the leukocyte formula, this indicates pathological processes in the body. However, 18 however, it must be remembered that leukocytosis - an increase in the number of leukocytes in the blood - can be not only pathogenic, but also physiological. White blood cells increase in number, for example, during pregnancy. And even active digestion promotes the growth of leukocytes. This is not outside the norm. Physiological leukocytosis occurs in healthy people, pathological - in painful conditions. Causes of physiological leukocytosis:
- food intake (the number of leukocytes does not exceed 10x109-12x109 cells/l);
- physical labor;
- taking hot and cold baths;
- pregnancy;
- childbirth;
- premenstrual period.
By the way, precisely because of the possible distortion of the analysis picture due to physiological leukocytosis, blood must be donated on an empty stomach. Before “going to the hospital” you should not engage in heavy physical work. For pregnant women, women in labor and postpartum, their own standards have been established. The same applies to children.
Pathological leukocytosis manifests itself when:
- acute and some chronic infections;
- inflammatory diseases;
- intoxications (nitrobenzene, carbon monoxide, food, quinine, arsenous hydrogen);
- severe oxygen starvation;
- allergic reactions;
- purulent-septic processes;
- malignant formations;
- blood diseases (leukemia, diseases of the hematopoietic system);
- comatose states;
- myocardial infarction;
- epilepsy;
- pregnancy at 5-6 months.
Pathological leukocytosis also manifests itself:
- during lactation;
- after heavy blood loss;
- with extensive burns;
- during the premenstrual period;
- after heavy physical or mental stress;
- after administration of camphor, insulin, adrenaline.
Typically, leukocytosis is associated with an increase in the number of neutrophils, less often - other types of leukocytes. Thus, the most common causes of pathological leukocytosis are infectious diseases (pneumonia, sepsis, meningitis, pyelonephritis, etc.). These may include infectious diseases that primarily affect cells of the immune system (infectious mononucleosis and infectious lymphocytes), as well as various inflammatory diseases caused by microorganisms (peritonitis, phlegmon, etc.). Some infectious diseases always occur with leukopenia. These are typhoid fever, malaria, brucellosis, measles, rubella, influenza, viral hepatitis in the acute phase. If there is no leukocytosis in the acute phase of an infectious disease, this is an unfavorable sign, meaning that the body has weak reactivity (resistance).
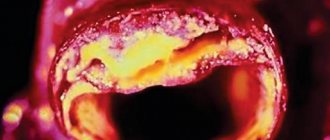
The level of leukocytes increases in people suffering from inflammatory diseases of non-microbial etiology - such as, for example, rheumatoid arthritis, systemic lupus erythematosus. The same applies to infarctions of various organs - myocardium, lungs, etc., since they are based on aseptic (microbial-free) inflammation.
Metastases to the bone marrow can disrupt hematopoiesis and cause leukopenia. This is also facilitated by the proliferation of body tissue as a result of new cell formation, diseases of the blood system, leukemic (more than 50x109-80x109 cells/l of leukocytes) and subleukemic (50x109-80x109 cells/l of leukocytes) forms. In the leukopenic form and aleukemic 20 (the content of leukocytes in the blood is below normal) forms of leukocytosis will not occur. When the spleen is removed (splenectomy), leukocytosis is observed with indicators of 15x109-20x109 cells/l with an increase in the number of neutrophils up to 90%.
But besides leukocytosis, there may also be its opposite. This is leukopenia - a decrease in the number of white blood cells in the blood - which is usually an accompanying symptom:
- radiation injury - exposure to ionizing radiation (X-rays, radiation);
- contact with certain chemicals (benzene, arsenic, DDT, etc.);
- collagenosis (systemic lupus erythematosus);
- taking medications (cytostatic drugs, some types of antibiotics, sulfonamides, etc.);
- viral and severe bacterial infections;
- diseases of the blood system, in particular leukopenic and aleukemic forms of leukemia, as well as other forms in case of overdose of cytostatics;
- functional diseases of the central nervous system;
- hematopoietic disorders, its insufficiency (bone marrow hypoplasia);
- diseases of the spleen, in which there is increased destruction of blood cells in this organ (liver cirrhosis, which occurs with an enlarged spleen);
- lymphogranulomatosis;
- some endocrine diseases (acromegaly, Cushing's disease and syndrome);
- some infectious diseases (typhoid fever, malaria, influenza, measles, brucellosis, viral hepatitis, prolonged septic endocarditis);
- metastasis of tumors to the bone marrow;
- inflammatory diseases (endometritis, gastritis, colitis, cholecystoangiocholitis - a lot of leukocytes are excreted from the body, therefore, in severe inflammatory and purulent-septic diseases, the initially occurring leukocytosis is replaced by leukopenia).
Leukopenia is often found in old people and exhausted people suffering from inflammatory and purulent-septic diseases. A lack of leukocytes is also observed in Addison's disease, and sometimes in thyrotoxicosis.
Page 5 of 11
Chronic neutrophilic leukemia
Chronic neutrophilic leukemia (CNL) is a rare myeloproliferative disease, when, due to abnormal changes in the stem (maternal) blood cell, a tumor appears from its descendants. In CNL, the descendants of the diseased stem cell are diseased neutrophil cells.
Healthy neutrophils (or neutrophil granulocytes) are one of the body's main defenses. Neutrophils make up about half of all immune cells. If you look at them through a microscope, you can see small granules inside the cells where the “weapons” of neutrophils are stored, which is why they are also called neutrophil granulocytes. Neutrophils, without understanding, destroy everything that is clearly different from the cells of their own body. If, for example, we have a splinter on our finger, then, in order to prevent bacteria from entering the blood, granulocytes will limit skin damage by a cordon, and then will attack the foreign body until it dissolves, or until the person removes it himself. Pus is what remains from such a struggle between neutrophil granulocytes.
CNL is more common in older people. As a rule, at the initial stage, patients feel well. Malaise, weakness, heaviness in the hypochondrium, severe sweating, fever, skin itching appear later, and the liver and spleen become larger in size, where tumor cells settle. In the blood test, the number of neutrophils increases significantly, and there may be other changes.
Diagnosis
The diagnosis of CNL is made on the basis of a prolonged increase in blood neutrophils (more than 25x109\l). When making a diagnosis, it is very important for the doctor to exclude other causes of changes that may appear as a result of another tumor, infectious or autoimmune process. Therefore, the patient is thoroughly examined: histological, cytological and cytogenetic examination of the bone marrow ; computed tomography and special tests to identify other diseases may be required.
Treatment
Currently, the generally accepted method of treating CNL is the prescription of drugs, the constant use of which reduces the number of tumor cells and improves the patient’s well-being, while such drugs have minimal side effects on the body. Over time, CNL always progresses to acute leukemia, which is treated according to acute leukemia . Young patients can be completely cured by undergoing a maternal blood stem cell transplant. Doctors are constantly trying new treatment methods using new drugs.
Due to the fact that CNL is a rare disease and it can manifest itself very differently in each individual patient, there are no clear figures on the effectiveness of treatment and the life expectancy of patients. The specialized literature describes cases where patients with effective treatment lived up to twenty years.
- Back
- Forward
Leukocytosis, monocytosis and neutrophilia: signs of severe depression.
To date, there are few reports that severe depression is accompanied by abnormalities in total white blood cell count (ie, leukocytosis) and white blood cell count (ie, neutrophilia, monocytosis, lymphopenia). These results, however, have not yet been confirmed in a large, well-controlled study. Leukocytosis was observed in patients with severe depression compared with normal subjects, while results were intermediate in those with minor depression. Leukocytosis was significantly more severe in men with major depression compared with women with major depression. The major leukocytosis associated with depression appears to be characterized by neutrophilia and monocytosis. There was a significant positive relationship between the overall severity of the disease, on the one hand, and the degree of leukocytosis, neutrophilia and monocytosis, on the other. The total numbers of both phagocytic cell populations (i.e., monocytes and neutrophils) were significantly and positively associated. These results may indicate the presence of an inflammatory process in patients with severe depression, especially men.
An increased white blood cell count, or leukocytosis, is a common laboratory finding. Appropriate evaluation of the specimen depends on which lines are enlarged and on the morphological data obtained from the analysis of the peripheral blood smear for further investigations. The presence of blasts causes acute leukemia and may require a bone marrow biopsy. Lymphocytosis can be morphologically divided into polymorphic and monomorphic populations. Polymorphic lymphocytosis is most consistent with a reactive process, while monomorphic populations belong to a lymphoproliferative neoplasm. The differential can be further narrowed based on morphological data. Myeloid leukocytosis can occur in a number of reactive conditions, as well as in myeloid malignancies. The types of cells present and morphology may help guide additional studies.
Leukocytosis is one of the most common laboratory pathologies in medicine and one of the most common reasons for hematological consultations. Effective evaluation of leukocytosis requires a careful history, a thorough physical examination, a thorough CBC and peripheral blood smear, judicious use of laboratory and radiological studies, and careful analysis. Definitive diagnosis may require bone marrow aspiration and biopsy, imaging studies, and specialized molecular tests. The differential diagnosis of leukocytosis includes physiological responses to a wide range of infectious and inflammatory processes, as well as numerous primary hematologic disorders such as leukemias, lymphomas, and myeloproliferative neoplasms. Leukocytosis can have various causes, including infectious, inflammatory, autoimmune and allergic. In addition, malignant causes of leukocytosis are discussed, including myeloproliferative disorders, acute leukemia, and chronic leukemia, as well as the treatment and monitoring of patients with these diseases.