What is cavernous angioma?
Cavernous angioma is a collection of abnormal vessels that is located in the brain or spinal cord and, in some cases, subcutaneously.
In various literature sources, this disease is also called “cavernous hemangioma”, “cerebral cavernous malformation”, “cavernoma”. Its dimensions vary from microscopic to several centimeters in diameter. It consists of many cavities (cavities) filled with blood and lined with a special type of cells called endothelial cells. Depending on the location in the brain, it can cause epilepsy, be a source of hemorrhages and cause severe headaches. Angioma of the left parietal lobe.
Morbidity
Cavernous angiomas occur in approximately 1 in 100-200 people. In most cases, the first symptoms appear after 30 years of age. In 20% of cases it is a genetically inherited disease, and several tumors are often detected at once.
Causes of angioma and risk factors
The disease is inherited in an autosomal dominant manner, with a probability of 50%. According to recent studies, at least three genes are associated with the hereditary form of the disease. A single formation can be detected at the birth of a child or develop during his later life. If parents and relatives did not suffer from this disease, then the angioma is called sporadic. The risk of developing such a tumor is the same for all people.
Angioma of the left parietal lobe during surgical treatment. Image: neurosurgery.wustl.edu
Symptoms of angioma
In most cases, cerebral angiomas are characterized by an asymptomatic course, but sometimes they lead to epileptic (convulsive) seizures. The type of seizure depends on the location of the tumor. Also, the presence of a mass in the brain can lead to neurological deficits, such as weakness of the upper or lower extremities, problems with vision, balance, attention and memory. Symptoms can wax and wane in waves, which is associated with repeated hemorrhages and an increase in the size of the angioma and reabsorption (absorption) of blood.
Angiomas are characterized by various types of hemorrhages:
- Slow, without changing size, since the rate of bleeding is approximately equal to the rate of blood reabsorption by the body.
- Profuse, with an increase in size and compression of the surrounding tissue of the brain or spinal cord.
- A leak in which blood enters the tissue of the brain or spinal cord through a defect in the wall of the angioma, ultimately destroying it.
What is angioma
Venous angiomas are localized in organs and tissues and can be multiple or single.
They are located in most cases on the upper half of the body. Their morphological basis is highly dilated lymphatic/blood vessels. The shape and size of pathological areas can vary, color - from colorless to red-blue. The lesions tend to progress rapidly. There are angiomas of the brain, liver, external genitalia, and bones. Angiomas are classified according to their structure:
- Simple (hypertrophic, capillary). Small venous and arterial vessels grow. If you study a photo of such an angioma, it will become clear that it is a bright red or bluish-purple spot. Its sizes can be different, even gigantic. If you press on the lesion, it will immediately turn pale due to the outflow of blood. Capillary angiomas of the skin extremely rarely transform into malignant formations.
- Branched (racellose). They are represented by plexuses of tortuous dilated vascular trunks. They are characterized by the presence of constant pulsation. The limbs and face are most often affected. Traumatization of venous branched angiomas is fraught with severe bleeding, which cannot always be stopped on its own.
- Cavernous (cavernous). They are formed by wide spongy cavities that are filled with blood. Cavernous angioma looks like a purple-bluish bumpy spot. Most often located under the skin. It feels hotter than the surrounding tissue. When stressed, it increases in size. A complex form is cavernous angioma of the brain, the treatment of which is very long and involves restoration of impaired blood flow.
- Combined. Combine subcutaneous and superficial location. Formed by overgrown vessels and other tissues (depending on location on the body).
The shape of angiomas is:
- stellate (point angiomatous formations, from which dilated small blood vessels extend in all directions);
- flat (vascular spots of pink-blue color located in the upper layers of the skin);
- nodular (seals protruding above the surface of the skin);
- serpiginous (rashes on the skin in the form of small burgundy nodules).
Cavernous angioma of the brain
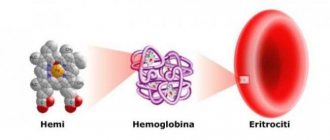
Cavernous angiomas (cavernomas) are most often congenital vascular anomalies, represented by single, much less often multiple cavities, separated inside by septa (septa) and filled with blood. The blood supply to the cavity is carried out from small arterioles and capillaries, and the outflow of blood through venules is of the same order. Due to the small caliber of the feeding vessels, the blood pressure in cavernomas is low, so the draining veins do not hypertrophy and are not visible during SCT/MRI/Angiography. A special feature of cavernomas is a very thin, defective vascular wall, so thin that the cellular elements of the blood - red blood cells - “sweat” through it and settle in the adjacent medulla. This process is called “diapedetic hemorrhage.” The products of the natural breakdown of hemoglobin (hemosiderin), contained in red blood cells, form a zone of chronic, specific and very recognizable changes on MRI around the cavernoma.
Cavernomas can be localized in any part of the brain, mainly in the cerebral hemispheres, as well as in the brain stem, cerebellum, subcortical ganglia, corpus callosum and lateral ventricles. In approximately 30-40% of cases, cavernous angiomas are combined with another type of vascular malformation - venous angiomas. Venous angiomas are an anomaly in the development of venous vessels in the form of a “bundle” of small veins (“Gorgon’s head”) gathering into one large drainage vein.
The incidence of cavernous angiomas is several cases per million population.
What is the danger of having a cavernous angioma?
Cavernomas can remain asymptomatic throughout life. However, in a number of patients, clinical manifestations can be of two types, both individually and in combination:
- Hemorrhage. Sometimes, an increase in blood pressure inside a cavernoma leads to local destruction of the vascular wall and the formation of intracerebral hemorrhage. Unlike AVMs, hemorrhages from cavernomas are never massive and do not pose a threat to the patient’s life, with the exception of extremely rare cases of cavernomas located in the lower parts of the medulla oblongata, where the centers of cardiovascular and respiratory regulation are located. However, when the focus of hemorrhage is located in any functional area, even a small volume of hemorrhage can lead to the appearance of neurological symptoms (for example, the development of contralateral hemiparesis when the focus is located in the precentral gyrus of the frontal lobe).
- Epileptic syndrome . In some cases, due to the chronic presence of hemosiderin in the medulla or with the development of acute hemorrhage, a focus of pathological brain bioactivity may form, clinically manifested by epileptic seizures of various structures (convulsive, non-convulsive, absence seizures, vegetative, polymorphic and others).
Thus, cavernomas extremely rarely pose a threat to the patient’s life, but can have a significant impact on the quality of life
How to diagnose a cavernoma?
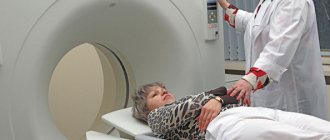
Magnetic resonance imaging (MRI) is the most informative method for diagnosing cavernomas. In T1 and T2 scanning modes, a cavity surrounded by a black rim of hemosiderin may be visible, with signs of acute and subacute hemorrhages. The most sensitive mode is T2* (“T2 with star”), which allows you to diagnose even small (1-2 mm) cavernomas that are not visible in other scanning modes
Computed tomography - its diagnostic value is limited, as a rule, to the acute period of hemorrhage (several days), when the image shows a focus of bleeding
Angiography is not informative in diagnosing cavernomas
How to get rid of a cavernoma?
In case of episyndrome formation and/or hemorrhage, two treatment methods are possible:
Surgical removal of cavernoma is a highly effective method that allows you to once and for all relieve the patient from the risk of repeated hemorrhages. Surgery is also effective if the patient has epileptic seizures, but its effectiveness is reduced in the case of a long history of epileptic syndrome
Radiosurgery is carried out according to the same principle as for arteriovenous malformations - the higher the dose, the better the effect. Therefore, cavernomas up to 1 cm in diameter are best treated, when the maximum permissible doses of radiation can be safely used. Morphological changes in this case are similar to those in arteriovenous malformations - the walls of the cavernoma and the mouths of the feeding vessels undergo hyalinosis, as a result of which the blood flow decreases, diapedetic hemorrhages stop, and the risk of repeated spontaneous intracerebral hemorrhages is reduced by 50-70%. Episodic attacks also become less frequent or disappear completely, but as in the situation with surgery, the longer the history of the disease, the less likely it is to completely recover from them
The generally accepted tactic for asymptomatic, incidentally detected cavernomas is observation.
Is it necessary to irradiate multiple cavernomas?
As in the case of single cavernomas, radiosurgical treatment is carried out only on the lesion that manifests itself clinically - hemorrhage or epileptic seizures
What to do with venous angioma?
The question often arises: how to get rid of venous angioma? Firstly, you should know that venous angiomas never manifest themselves as hemorrhages or epileptic seizures. Secondly, although they represent a venous network that is abnormal in structure, they nevertheless take full part in the local venous circulation of the brain. The only option for the appearance of clinical symptoms associated with venous angioma is the spontaneous development of thrombosis of the draining vein. This situation is more hypothetical than real. In this case, the patient will experience cerebral venous infarction with severe swelling at the site of impaired venous outflow. And only one way can help cope with such a situation - thrombolytic and anticoagulant therapy. Attempts to surgically or radiosurgically influence venous angiomas not only do not make any sense, but in a similar manner to thrombosis will lead to gross local disturbances of venous blood flow. Thus, the mere presence of venous angioma is not a reason for any treatment.
Which cavernoma treatment method is best?
From the point of view of preventing recurrent hemorrhages, the effectiveness of surgical treatment is higher. However, when cavernomas are localized in functionally important or hard-to-reach areas of the brain (for example, in the subcortical nuclei, brain stem), surgery itself has a high risk of residual neurological deficit, and radiosurgery can largely avoid these complications. Therefore, the decision on the optimal method of influence is made individually, taking into account all possible factors, incl. and taking into account the informed choice of the patient himself
Fig. 1 Result of radiosurgical treatment of brainstem cavernoma. On the left is a cavernous angioma of the lateral surface of the brain stem at the time of Gamma Knife radiosurgery. On the right - a significant reduction in the size of the cavernoma 3.5 years after radiosurgery. No recurrent hemorrhages
Causes of angioma formation
Angioma in newborns is a standard clinical picture, since this disease in most cases is congenital. The source of the development of neoplasms in adulthood are persistent fetal anastomoses located between the veins and arteries. The proliferation of blood vessels in a benign tumor leads to the growth of the tumor itself.
The causes of angioma are as follows:
- hereditary predisposition;
- changes in hormonal levels;
- diseases of the gastrointestinal tract;
- dysfunction of lipid metabolism;
- skin pigmentation disorders.
In rare cases, venous angiomas of the skin occur after trauma to the skin area (bruises, cuts). They can also accompany malignant neoplasms of internal organs and cirrhosis of the liver.
Angiomas: causes of appearance
Until now, scientists cannot name the exact reasons for the appearance of vascular formations. Doctors agree that vascular pathology begins during embryonic development. Infectious diseases suffered by the mother can affect this. Toxicosis, anemia of a woman during pregnancy, and serious hormonal fluctuations also contribute to the appearance of abnormalities. Acquired angiomas occur due to sunburn, liver disease, skin injuries, and increased fragility of blood vessels.
Symptoms of angioma
Symptoms of angioma depend on the type of vascular tumor, its size and location. In newborns, it is diagnosed immediately or several months after birth, and can grow very quickly, covering large areas of the skin.
Vascular angiomas can affect:
- Integumentary tissues - skin, mucous membranes of the genitals, subcutaneous tissue. Angiomas are also found in the mouth.
- Musculoskeletal system - muscles, bones. A severe form of the disease includes hemangioma of the vertebral body.
- Internal organs.
If integumentary hemangiomas cause cosmetic defects, then hemangiomas of internal organs provoke the occurrence of disturbances of important functions - urination, breathing, vision, defecation.
Angiomas of muscles and bones are accompanied by:
- skeletal deformation;
- severe pain in the joints;
- frequent fractures;
- radicular syndrome (compression of the spinal nerves).
Venous angiomas of the brain (cerebellum, left/right frontal lobe, etc.) are very dangerous. They lead to subarachnoid hemorrhage and epilepsy. Also, due to compression of the brain vessels by the tumor, the following symptoms may occur:
- convulsions;
- headache;
- nausea, vomiting;
- dizziness;
- noise in the head;
- taste disturbances;
- speech problems.
During the growth process, angiomas can become inflamed, causing phlebitis and thrombosis. A common complication is bleeding due to trauma.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Prevention of angioma
It is impossible to prevent the occurrence of congenital vascular pathologies, so effective prevention does not exist. There are several ways to reduce the risk of abnormalities such as red spots. Women are advised to carefully plan their pregnancy, and while carrying a child, follow all the recommendations of the obstetrician-gynecologist.
As for senile vascular anomalies, their occurrence can be prevented by avoiding prolonged exposure to the sun and cold, and by building a healthy diet rich in minerals and vitamins. It is also recommended that older people lead a healthy lifestyle and do not ignore physical activity agreed upon with their family doctor.
Diagnostics
Angiomas located on the surface of the skin are diagnosed during examination and palpation. The characteristic coloring, ability to contract and increase in size when pressed and strained allow the doctor to easily make the correct diagnosis.
If the localization of the lesion is more complex (internal organs, bones, brain), a number of diagnostic measures are required:
Skeletal hemangiomas are identified using x-rays of the spine, ribs, bones, skull and pelvis.
To identify angiomas of internal organs, antiography (contrast x-ray examination of blood vessels) of the kidneys, brain, lungs, etc. is performed.
Pharyngeal angiomas are examined by an otolaryngologist.
Ultrasound diagnostics allows you to determine the exact depth of growth of the angioma, its structure and location features. If a vascular angioma is suspected, the doctor may additionally prescribe a puncture. The resulting yellowish liquid is examined in the laboratory. This makes it possible to differentiate angioma from lymphadenitis, lipoma, cyst, hernia.
An example of removal of a cavernoma of the anterior parts of the right temporal lobe of the brain
A male patient, born in 1989, came to the Petrograd Clinical Hospital because he was concerned about complex convulsive seizures.
MRI of the brain revealed a small cavernoma of the right temporal lobe of the brain up to 1.5-2 cm in diameter.
Treatment of angioma
Treatment of angioma is aimed at stopping its growth, eliminating the pathological process and normalizing the functioning of the vascular network. Indications for urgent intervention are:
- extensive tissue damage;
- rapid growth of the tumor;
- localization in the neck, head;
- frequent bleeding;
- dysfunction of the organ in which the angioma is located.
Watchful waiting is justified only if regression of a vascular benign tumor is observed.
Among the most common treatments for angiomas:
- Diathermoelectrocoagulation. Cauterization with electric current is indicated if it is necessary to remove hard-to-reach punctate angiomas and angiofibromas. The method cannot be used if the angioma is deep and occupies a large area.
- Laser treatment. Using a laser, the doctor removes pathological tissue layer by layer. The advantage of laser treatment of angiomas is minimal bleeding.
- Radiation treatment. Allows you to achieve good results when removing angiomas of complex anatomical localization.
- Surgery. It is used if the vascular tumor is deep and it is not possible to remove it without affecting the surrounding healthy tissue.
- Cryotherapy. Makes it possible to remove simple small angiomas of any location. During the procedure, liquid nitrogen is applied to the tumor. The method is painless and does not cause bleeding.
- Sclerosing therapy. Seventy percent alcohol is injected into the tumor. The treatment is painful and is suitable if the angioma is located in the deep layers of the skin.
- Hormonal therapy. Relevant if the lesion is extensive, angiomas grow quickly.
- Excision of angiomatous areas followed by reconstruction of the vessel.
- Ligation of the arteries supplying the angioma. A ligature is applied to the end of the artery, as a result of which the neoplasm gradually dies.
It is possible to treat angioma with folk remedies:
- Apply the kombucha to the tumor site and fix it. After a day, replace the compress. The duration of such treatment is 2-3 weeks.
- Dilute a tablespoon of copper sulfate with 100 ml of clean water. Wipe the neoplasm with the resulting liquid 4-5 times a day for 10 days.
- Apply a compress of onion pulp to the affected area of skin for 10 days. Change the bandage every 12 hours.
- Cover the angioma with fresh grated carrots and tie gauze on top. Change 3 times a day.
- Mix fresh celandine juice in a ratio of 1:4 with petroleum jelly and add a drop of 0.25% carbolic acid. Use the ointment daily in the morning and evening.
- If the angioma has affected the internal organs, you can use the following recipe: pour 3 tablespoons of potato flowers into 300 ml of boiling water. Leave in a thermos. Drink half a glass 3 times a day half an hour before meals. The treatment course is 2 weeks.
It should be remembered that any folk recipe can be used only after consultation with your doctor. Some medicinal plants can provoke the growth of angiomas, so preparing decoctions and infusions from them yourself is not recommended.
Advantages of laser removal of angiomas on the body:
- Selectivity of the laser beam - only the vessels that make up the tumor are destroyed;
- Bloodlessness - the procedure for laser vaporization of a hemangioma takes place without a drop of blood, even if the formation is large;
- High cosmetic result - after laser removal of angioma there are no traces left on the skin;
- Single use - removal of angioma is carried out at one time;
- No anesthesia required.
Rice. 4. Angioma under microscopy consists of vessels
Rice. 5. Removal of angioma on the body with a laser
Danger
A small spot formed on the skin can go unnoticed or be ignored by the patient for a long time. Since it can transform into a malignant formation, the lack of necessary treatment can lead to dire consequences.
Particular attention should be paid to angiomas located in places of increased friction with clothing (neck, chest, abdomen, shoulders), on the scalp. Frequent traumatization can lead to inflammation of a benign tumor and its rapid growth and bleeding.
The greatest danger to life is posed by angiomas of the brain and internal organs. As practice shows, if you do not treat a cerebral angioma, the prognosis is unfavorable - the area of accumulation of blood vessels will increase, which will lead to their rupture, hemorrhage in the brain and death.
What if you have an angioma?
If you have an angioma, it should still be removed. Removal can be done with a coagulator or radio knife, but in most cases they leave a noticeable scar on the skin. This is explained by the fact that angioma consists of vessels, and the coagulator and radio knife cannot separate the vessels from other tissues and cauterize everything. It is better to remove angiomas on the body using a laser, since a laser beam of a certain wavelength is capable of destroying only tumor vessels without affecting neighboring tissues.
Diagnosis of arteriovenous malformations
In most cases, vascular malformations do not manifest themselves in any way, and therefore can be discovered incidentally during examination for other diseases. Angiography allows you to make the most accurate diagnosis of arteriovenous malformation. This is an x-ray research method, which consists of injecting a radiopaque substance into the patient’s artery, which allows blood vessels, their location, course, diameter and other parameters to be clearly and clearly recognized on the x-ray. Unfortunately, this procedure is invasive and comes with some risk of complications (stroke, anaphylactic shock). Currently, the so-called superselective angiography, in which a thin catheter is inserted into the artery, through which the doctor injects a radiopaque substance directly into the area of the vascular malformation.
The two most commonly used methods for diagnosing arteriovenous malformations today are computed tomography and magnetic resonance imaging (CT and MRI). Both methods are non-invasive and completely safe, while CT involves the use of X-rays, and MRI uses an electromagnetic field. In addition, MRA (magnetic resonance angiography) is currently used to diagnose vascular pathologies. All these methods allow you to accurately diagnose malformations and determine the necessary parameters.
3. Treatment of hemangiomas
Among the treatment methods for hemangioma are the following:
- traditional surgery;
- radiotherapy;
- embolization or sclerosis of tumor vessels;
- puncture vertebroplasty.
Regarding surgery
, then today this technique is rarely used. During this operation, the affected soft and bone tissues are usually excised. The operation poses a certain risk for the patient, since it is often accompanied by heavy bleeding.
Radiation therapy
has been used to treat hemangioma since the 30s of the last century. It consists of irradiating the tumor, as a result of which a scar forms in its soft tissues. At the same time, the tumor remains unchanged in the bone tissue. This technique has certain advantages over surgical intervention, however, it does not give the desired result.
A more progressive way to combat hemangioma is embolization or sclerosis of the tumor.
by blocking (thrombating) the vessels feeding it with a special substance. Among the disadvantages of the method, the excessive technical complexity of performing this operation is noted.
Today, the most popular and advanced technique is puncture vertebroplasty.
, during which the affected vertebra is filled with a special polymer composition with the addition of a contrast agent. This method is characterized by the highest efficiency and the minimum number of complications.
About our clinic Chistye Prudy metro station Medintercom page!
2. Symptoms of the disease
are asymptomatic in most cases
without causing any pain or disruption of any body functions. These spinal tumors are discovered by chance during an examination.
Hemangiomas usually do not show a tendency to grow, and therefore in this case they do not require treatment - periodic diagnostic monitoring is quite sufficient. However, among this type of tumors there are also quite aggressive ones that can grow quickly, while squeezing nearby nerve pathways. In this case, pain occurs and the risk of a so-called vertebral compression fracture increases with all the ensuing consequences in the form of various neurological disorders. There are also cases where the hemangioma spread beyond the vertebra and put pressure on the contents of the spinal canal, resulting in paralysis and lack of sensitivity below the tumor location. These are the hemangiomas that require immediate treatment.
Visit our Neurosurgery page
1.What are hemangiomas?
Vertebral angiomas, or otherwise hemangiomas
, are a benign tumor formed by blood vessels, which often (about 10% of cases) occurs in the vertebral body.
Hemangioma most often occurs in the thoracic spine, and least often in the cervical spine. The most common option is single neoplasms in a single vertebra, but there are also lesions of several vertebrae at once - from two to five.
A must read! Help with treatment and hospitalization!